Diode Laser in Management of Tracheobronchial Typical Carcinoid: A Case Report with Review of Literature
Navin Bhambhani1, Jayesh Gori2, Vishwanath Masurkar3, Sonal Thombre4
1 Consultant Oncosurgeon, Sir H.N. Reliance Foundation Hospital and Jupiter Hospital, India.
2 Registrar, Department of Surgical Oncology, Fortis Hospital, Mulund, India.
3 Clinical Associate, Department of Surgical Oncology, Jupiter Hospital, Thane, India.
4 Physician Assistant, Department of Surgical Oncology, Jupiter Hospital, Thane, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jayesh Gori, 35, Odhav Aashish, Janardhan Park, Raghunath Nagar, Wagle Estate, Thane (W)-400604, Maharashtra, India. E-mail : Jayeshgori26feb@gmail.com & docnavin@yahoo.co
Tracheobronchial carcinoids are relatively uncommon neoplasms with malignant (though indolent) potential and variable behavior. Clinical presentation is usually similar to any obstructive tracheobronchial lesions or rarely with presentation of carcinoid syndrome. Management varies from Pneumonectomy to use of lung sparing bronchoscoplastic techniques. We report the case of a 32-year-old male patient diagnosed with carcinoid of left main bronchus. Patient was successfully treated with trans-bronchoscopic diode laser. At 24 months of follow up patient remains asymptomatic and recurrence-free.
Bronchoscoplastic techniques, Endoscopic Resection, Laser fulgurations
Case Report
A 32-year-old, married, non smoker, hindu male was referred to our hospital with complains of increasing breathlessness, with minimal productive cough since 2 months, mild grade fever on and off since 15-20 days. His father had expired a year back due to carcinoma of lung.
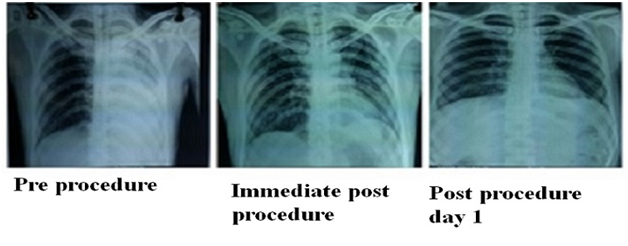
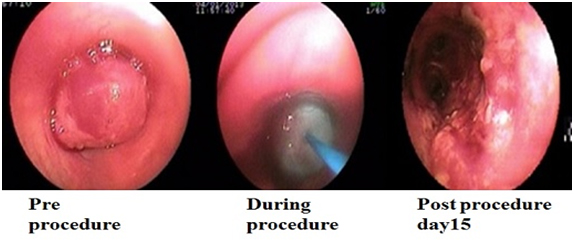
He was presented in casualty with tachycardia (pulse- 110/minutes) and tachypnea (Respiratory rate- 30/minutes) with average general condition. All investigation reports i.e. CBC, Renal function test, Liver function test including PT-INR and ECG were within normal range. Chest radiograph was suggestive of complete collapse of left lung with mild pleural effusion and CECT thorax revealed a 1.2x1.0 cm sized enhancing soft tissue density lesion in the proximal left main bronchus 1.5-2.0 cm distal to carina with complete occlusion of the left main bronchus and resultant collapse of the left lung [Table/Fig-1,2]. Flexible bronchoscopy confirmed a raised red glistening vascular, lobulated mass about 1.5 cm away from carina with near complete obstruction of left main bronchus. The biopsy was suggestive of small rounded cells with uniform nuclei arranged in trabecular pattern without necrosis i.e. well differentiated carcinoid tumour.
Series of chest x rays showing improvement in left lung expansion
CT images showing Pre Procedure and Post Procedure changes
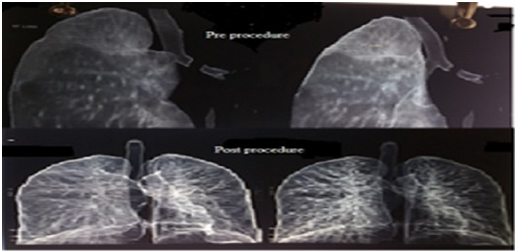
The lesion was excised bronchoscopically using Diode contact laser (GaAIAs) of 4W power. Complete bronchoscopic excision of left main bronchus mass under local anesthesia and sedation was achieved. The pedunculated mass was negotiated with difficulty and the left main bronchus entered to assess distal extent of the lesion. Repeated laser fulgurations of the entire lesion done and the tumour delivered piecemeal using cup and multipunch crocodile forceps. Entire mass including base were excised and removed bit by bit followed by Bronchoscopic lavage and aspiration of collected secretions [Table/Fig-3]. Haemostasis was confirmed. Patient tolerated procedure well without any post procedure bleeding. Postoperatively patient was observed in ICU for a day and shifted to ward. The radiographs showed improved lung expansion with symptomatic improvement. Patient was discharged on postoperative day 5 [Table/Fig-1]. Final histopathology report was suggestive of typical Carcinoid. Check bronchoscopy on postoperative day 15 was suggestive of shaggy tags at laser resection bed 2 cm from carina. After a multidisciplinary meeting (MDM) surveillance was planned with 6 monthly bronchoscopy and annual CT scan thorax. On regular follow up with bronchoscopy, till 2 years there was no evidence of diseases.
Discussion
Carcinoids tumours are classified as typical (<2 mitoses/2 mm2) or atypical (2-10 mitoses, necrosis, architectural disruptions) [1]. Primary broncho-pulmonary carcinoids are rare and account for 0.4%to 3% of resected lung cancers. Young age, central tumour and no nodal enlargement favors typical carcinoid. Usually patients with peripheral tumours are asymptomatic and while patients with central tumours are symptomatic with cough, recurrent pneumonia, and/or haemoptysis [2].
The various techniques for the management vary from pneumonectomy to endoscopic resections. The mainstay of treatment of carcinoids is surgical resection. For typical carcinoid (TC) tumours 90% or higher survival at 5 and 10 years survival is achieved with low recurrence (3% to 5% only) [2]. Management for tracheobronchial carcinoids ranges from surgical resection to bronchoscopic treatment.
Typical carcinoids with the following features can be cured bronchoscopically: Small volume (<4–5 cm3), central strictly endoluminal location, pedunculated or limited implantation base (<1.5 cm2) and minor wall infiltration, good bronchoscopic tumour accessibility with clearly visible distal tumour margin, high-resolution CT scans showing no extra luminal tumour extension [3]. In intraluminal typical bronchial carcinoid Brokx HA et al., suggests that initial bronchoscopic treatment is a potentially more tissue-sparing alternative than immediate surgical resection [4] and also as suggested by Zdenko et al., it also results in histologically confirmed disappearance of tumour [5]. In this case, we were able to resect tumour bronchoscopically and sampled base confirmed a negative margin.
Ishiguro T et al., reported treatment of ten patients with tracheobronchial malignant tumours using high power diode contact laser (GaAIAs) with no incidence of massive Haemorrhage or serious respiratory failure and suggested diode laser are useful and safe for the treatment of obstructive lesions due to tracheobronchial polypoidal tumours [6]. Zdenko et al., reported 25 years of experiences with Nd; YAG laser (exclusively for 18 years) and Diode laser (8 years) of 1244 patients with malignant and benign lesions suggest that the Nd; YAG laser is more effective in cases of larger tumour masses and Diode laser is more precise with less risk of haemorrhage, perforation and other complications [5]. The present case met the criteria for bronchoscopic laser resection and had an uneventful recovery. He continues to be disease free on surveillance.
Conclusion
In literature, only limited study on use of high power diode contact laser (GaAlAs) system with a flexible broncho fiberscope is available. proof of efficacy of this technique in management of tracheobronchial lesions requires studies with larger number of cases. However, rarity of such tumours makes it impossible to obtain such data. Keeping in mind the low mitotic index of well differentiated carcinoids, with good prognosis, prolonged survival and low recurrence rate encourage treatment using more conservative and less invasive methods such as diode laser in the management of obstructive tracheobronchial lesion.
[1]. Travis WD, Rush W, Flieder DB, Falk R, Fleming M V, Gal AA, Survival analysis of 200 pulmonary neuroendocrine tumours with clarification of criteria for atypical carcinoid and its separation from typical carcinoidAm J Surg Pathol 1998 22(8):934-44. [Google Scholar]
[2]. Escalon J, Detterbeck F, From Carcinoid Tumours. In: Shields T, LoCicero JI, Reed C, Feins RGeneral thoracic surgery 2009 7th edPhiladelphiaLippincott Williams & Wilkins:1539-54. [Google Scholar]
[3]. Sergio C, Pierfranco F, Carlo T, Curative Bronchoscopic Laser Therapy for Surgically Resectable Tracheobronchial Tumours: Personal ExperienceJournal of Bronchology and Interventional Pulmonology 2002 9(2):90-95. [Google Scholar]
[4]. Brokx HA, Risse EK, Paul MA, Grünberg K, Golding RP, Kunst Initial bronchoscopic treatment for patients with intraluminal bronchial carcinoidsJ ThoracCardiovasc Surg 2007 133(4):973-78. [Google Scholar]
[5]. Tudjman Z, Ostojic V, Results and 25 years’ experience with laser therapy in tracheobronchial endoluminal processesLaser in Medicine 2013 1(2):1-12. [Google Scholar]
[6]. Ishiguro T, Sawa T, Yoshida T, Yokoyama M, Murakawa S, Azuma K, Treatment of tracheobronchial malignant tumours using a new high power diode contact laser (GaAlAs) systemGan To Kagaku Ryoho 2002 29(12):2205-08. [Google Scholar]