Intra-articular proximal tibia fractures i.e. tibial plateau fractures, account for almost 1% of all fractures and usually result from axial loading combined with some varus and valgus forces [1]. These fractures present in a wide range of patterns, with varying degrees of displacement, depression of articular surface and the predominance of involvement of the tibial condyle, either medial, lateral or both. The Schatzker classification system [2], widely used for these fractures, classifies them into six grades, out of which the grade V (bicondylar) and grade VI (bicondylar with diaphyseal discontinuity) are the most severe injury patterns, associated with high incidence of complications, especially those relating to overlying soft tissues, infection, articular malreduction and neurovascular.
The goal of treatment in such fractures is the anatomical restoration of the articular surface congruity, prevention of post traumatic degenerative joint disease, healing of the crucial soft tissue cover and early mobilization so as to prevent joint stiffness [3,4]. The choice of treatment depends upon the patient’s age, his medical condition, the fracture configuration, degree of fracture displacement and condition of the overlying soft tissue cover, associated bony injuries and any neurovascular complications. Open reduction and internal fixation with plates and screws has been termed as the ‘gold standard’ treatment for these fractures so as to achieve a precise anatomic reduction of the joint surface which is solid enough to allow early mobilization; but these modalities of internal fixation, especially with a compromised soft tissue envelope and bulky metallic hardware, have been associated with complications [5]. Of late, the minimally invasive fixation systems and reduction of the intra articular fragments under arthroscopic visualization has also been used for these fractures [6,7]. The role of external fixators, either half-pin or ring and wire, has been evaluated in various studies of comminuted complex tibial plateau fractures, and quite encouraging results have emerged [8–12]. The present study has been conceptualized to study the definitive treatment of such complicated tibial plateau fractures by JESS (Joshi’s External Stabilization System) along with limited internal fixation of the articular surface, in some cases, by means of percutaneously inserted condylar screws. JESS was originally developed by an eminent Indian Orthopaedic surgeon, Dr. B.B. Joshi and his team. It is a wire based external fixator system, the kirshner wires being connected to rings and connecting rods by means of link joints. Such fixator systems are expected to restore reasonable metaphyseal reduction, using ligamentotaxis, by distraction of the head and shaft assembly [10,13,14]. The concept of ligamentotaxis is that, for traction to be effective it must be balanced by counter traction provided by ligaments and soft tissue surrounding the bone. This pull and counter pull aligns the fracture fragments while restoring the length; and the external fixator helps to maintain this tissue tension [14].
JESS is light weight, inexpensive and simple to use. Such fixator systems being minimally invasive, avoid further trauma to the soft tissues by obviating the need of big incisions, allow easy local surveillance and wound care besides permitting early mobilization of the knee in the immediate postoperative period, thus preventing joint stiffness so commonly encountered in intra-articular injuries. With this study, we intend to assess the outcome of the use of JESS, which is a wire based circular external fixator, in the treatment of such high grade tibial plateau fractures, as regards its functional results and complications, if any.
Materials and Methods
The present prospective, uncontrolled study was done on 20 patients of tibial plateau fractures, admitted in a tertiary care teaching hospital at Udaipur, between 2011 and 2013 and classified as Schatzker’s grade VI [2].
All the patients were applied calcaneal traction and advised elevation of the limb, till the day of surgery; and were constantly observed for any deterioration in the distal neurovascular status of the limb. Patients with open injuries were taken up immediately for wound debridement and irrigation before the definitive fixation was done. Prophylactic intravenous cephalosporins and aminoglycosides were administered to all the cases till at least three days after surgery. The condition of the soft tissues, apart from the general condition of the patient, was the most important factor in deciding the time up to surgery. A valid, informed consent for surgery was obtained from the patients and they were taken up for surgery when the swelling of the soft tissue cover showed a reversing trend. Preoperatively, anteroposterior and lateral radiographs of the upper tibia, 3D CT images of the knee, and routine pre-anaesthetic investigations were done.
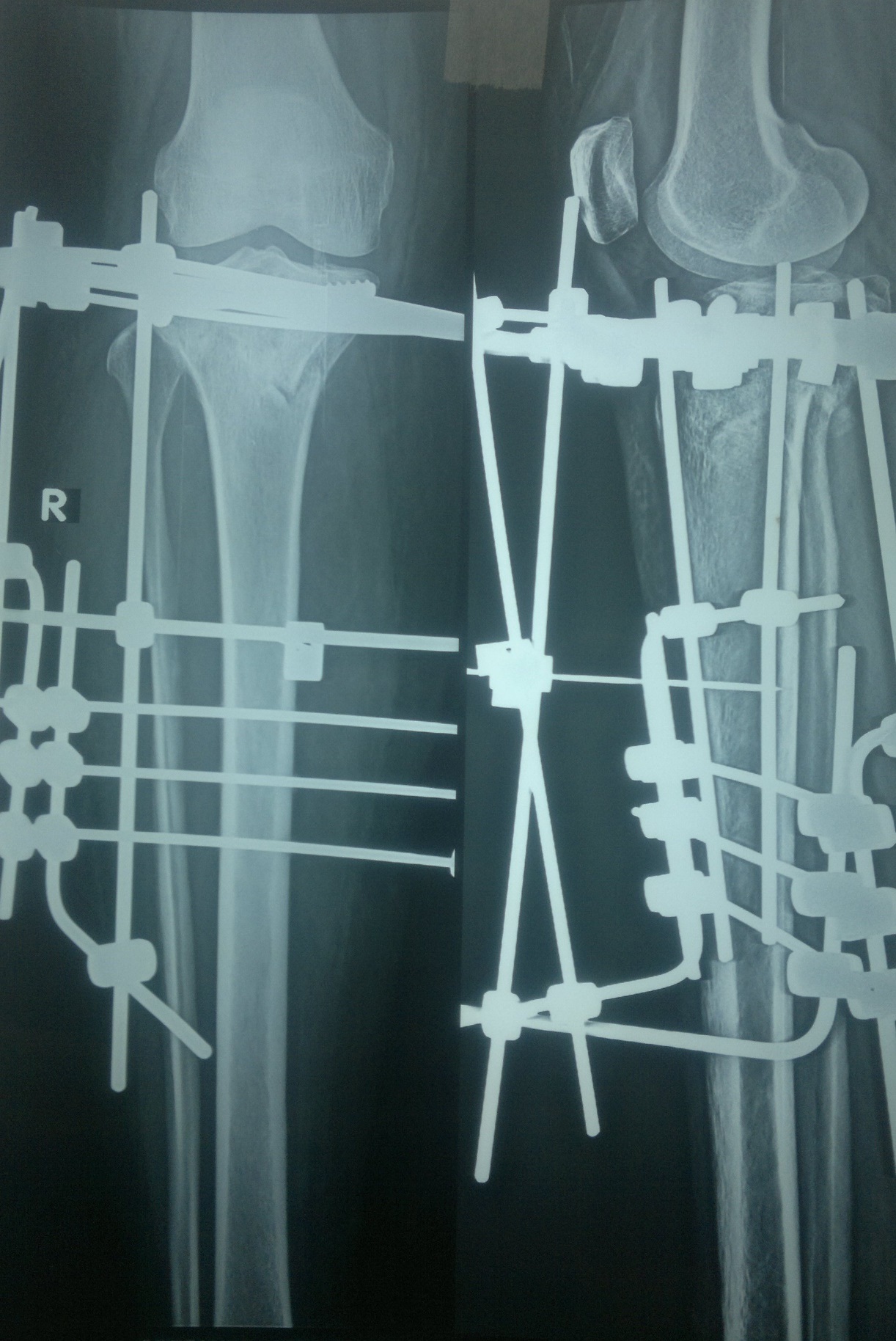
The patients were administered, either general or spinal anaesthesia, as decided by the anaesthetist. No tourniquet was used. The reduction of articular fragments was done percutaneously under image intensifier. Limited incisions for minimal open reduction were given to elevate the articular fragments through a small anteromedial cortical window in the metaphyseal region, if the articular in congruity was more than 3 mm [10,13]; and guide pins inserted after reduction, over which cannulated, 7 mm partially threaded, lag screws were inserted in the juxta articular region, either one or two in number, so as to engage the major condylar fragmentsin a lag fashion and also to maintain reduction of articular surface [8,10]. The screws were not used in cases where the intraarticular fragments were minimally displaced. In this series, additional fixation with periarticular lag srews was done in 16 (80%) patients. Three, long, smooth Kirchner wires of 3 mm diameter were then inserted in the proximal tibial condylar fragment through the safe zones, at least 1.5 cm away from the articular surface; one inserted from posteromedial to exit on the anterolateral aspect; the second inserted from posterolateral to exit on the anteromedial aspect and the third from direct lateral to direct medial aspect in between the first two wires. These wires were then fixed to head rings, which were half rings, by means of link joints after tensioning. These head rings were two in number and concentric, so as to provide the desired stability to the ring assembly of the proximal condylar fragment. Then, 3 Kirchner wires of 3 mm each were inserted in the tibial shaft from lateral aspect to exit from the medial side. The head ring assembly was then connected to the shaft assembly while giving manual traction to reduce the metaphyseal fragments by ligamentotaxis. The assembly was then locked by way of a series of connecting rods and link joints, after checking the reduction as well as alignment under the image intensifier, so as to provide a secure, stable and rigid frame; as seen in [Table/Fig-1].
Showing components of JESS assembly

From the first postoperative day, patients were put on a physiotherapy regimen consisting of knee mobilization exercises, both passive and active-assisted. Pin tract cleaning with hydrogen peroxide and povidone iodine was done daily [8,15]. Touch-down weight bearing was allowed until radiological union was evident. The fracture union was determined using radiographic and clinical assessment at follow up visits in the orthopaedic clinic, scheduled at 6, 12, 18 and 24 weeks postoperatively. The patient was looked for complications, if any and functional outcome was assessed using the KSS (Knee Society score) criteria [16,17]. JESS was removed after the patient was advised full weight bearing, on evidence of clinical and radiological union; and he was instructed to put on a removable long leg brace while walking, for few days.
Results
Of the 20 patients, 16 patients (80%) were male. Twelve cases (60%) involved the left tibia and 8 (40%) fractures were on right. The mean patient age was 39.4 years (range 28-54 years). Road traffic accidents, especially fall from motorbikes, accounted for most of the injuries (n=12), while pedestrian accidents (n=4), injury due to fall from height (n=3) and injury due to fall while playing (n=1) were the other modes of injury. Compound injury was present in 7 patients (35%), with 3 having grade II and 4 patients having grade III compound injury. Associated fractures and/or head injury was present in 8 patients (40%).
Preoperatively, all the patients had associated soft tissue complications, ranging from swelling and bruising of the soft tissue cover, to blister formation in 8 cases (40%) and impending compartment syndrome in 3 patients (15%). Fasciotomy was not needed in any of the patients. One patient (5%) with associated fracture neck fibula had foot drop, which recovered spontaneously in 6 weeks.
The mean duration between admission and day of surgery was 6 days (range 1-12 days). There were no significant intraoperative complications. Blood transfusion was not required for any of the patients during this surgery. The mean interval between surgery and discharge from hospital was 4 days (range 2 – 14).
The mean follow-up period was 24 weeks (range 18–32 weeks). The range of motion averaged 115 degrees of flexion (range 90-125 degrees), with 3 patients (15%) reporting an extension lag of 5-10 degrees, up till 24 weeks of follow up. [Table/Fig-2] shows a preoperative radiograph and [Table/Fig-3] depicts a 6 week postoperative radiograph of the same patient showing good intra articular reduction. [Table/Fig-4,5] show the range of motion of the knee in a patient at 14 weeks postoperatively. The mean interval between surgery and full weight bearing was 15 weeks (range 12-24 weeks).
Preoperative X-ray of a patient

Postoperative X-ray of same patient at 6 weeks
Picture showing range of movement in a patient after removal of JESS at 14 weeks


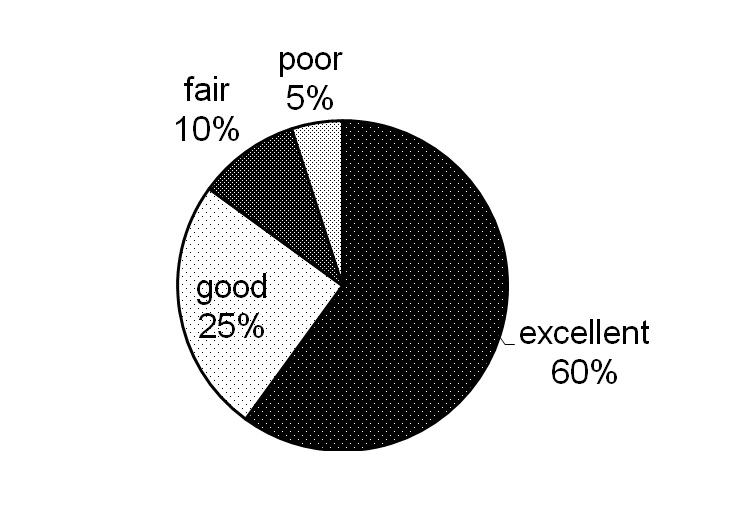
The clinical and functional results were assessed using the parameters of pain, knee range of motion, any flexion contracture or extension lag, varus-valgus alignment and stability in both anteroposterior and mediolateral aspects, using the KSS (Knee Society Score) criteria [16,17]. In this study, excellent results (KSS > 80) were seen in 12 patients (60%), good results (KSS 70-79) were seen in 5 patients (25%), fair (KSS 60-69) in 2 patients (10%) and poor (KSS < 60) in 1 patient (5%); as shown in [Table/Fig-6].
Pie chart showing functional results as percentage of total
Complications seen were, pintract infections in 2 cases (10%), which were managed by oral antibiotics and regular pin site dressings; and 1 case of non union (5%), in which the tibial plateau fracture extended into proximal 1/3 of the tibial shaft with severe comminution. The non union was seen at the level of proximal tibial diaphysis. At 26 weeks of follow up, this patient was advised internal fixation with bone grafting, but the patient did not report again. No systemic complications or deep infections were encountered in any case. Soft tissue complications, wound breakdown, or any significant functional impairment due to varus/valgus instability was not seen.
Discussion
Soft tissue complications in high grade tibial plateau fractures may range from swelling, bruising, open wounds and blister formation, to limb threatening compartment syndrome. The conventional double plating technique of internal fixation of these fractures involves incisions through the compromised soft tissue cover, extensive soft tissue stripping and hence, devitalization of the already traumatized fracture fragments. Consequently, these techniques have often been associated with complications like overlying soft tissue necrosis, problems in wound healing, exposure of metallic hardware and high rate of deep infection including osteomyelitis [5]. Plating with a relatively newer technique of less invasive stabilization system (LISS) has also been reported to have a higher incidence of postoperative malalignment and symptomatic hardware irritation [6].
The advent of newer devices and techniques has led many surgeons to use external fixators, with or without limited internal fixation, for the definitive management of the comminuted tibial plateau fractures using the principle of ligamentotaxis, with excellent outcome [18–21]. The Canadian Orthopaedic Trauma Association [11], reported lower rate of early postoperative complications and better functional score in patients treated with external rather than internal fixation, for these fractures. Even in the presence of severe soft tissue compromise, the external stabilization systems, in contrast to traditional techniques of internal fixation, allow for early surgery and hence, early stabilization of the fracture with minimal devitalization [18].
Babis et al., in their study of high energy tibial plateau fractures treated with hybrid external fixators reported excellent and good results in 85% patients while the reported complications in their series were deep infection (3%), pin tract infection (9.1%) and deep venous thrombosis (3%) [8]. Catagni et al., in their series of grade V and VI tibial plateau fractures treated with circular external fixators, reported 50.85% excellent and 45.76% good results [19]. Kataria et al., in their study using small wire external fixation with beaded “olive” wires, reported 94.7% excellent and good functional results [13]. Muhammad AK et al., have reported 81.8% excellent and good functional scores, using Illizarov ring fixator and beaded olive wires, for tibial plateau fractures [22]. The results in our study and other studies [10] using JESS are comparable with the above studies using either hybrid external fixators or other types of circular fixators, with or without beaded olive wires.
JESS, using simple k-wires rather than tensioned beaded olive wires as used in other circular fixators, may have a disadvantage in not providing inter fragmentary compression across the fractured condylar fragments. Hence, in this study, minimal internal fixation with one or two percutaneously inserted cancellous screws were used in some cases, for lag effect across condylar fragments and maintaining reduction of the articular surface. Such additional lag screw fixation has been used in many studies of tibial plateau fractures treated with external fixators, with favourable results [8,10,19,21]. Katsenis et al., in their study of type V and VI tibial plateau fractures, treated with small wire external fixators, used additional minimal internal fixation even while using beaded wires and reported excellent and good function in 76% patients [4].
The results in our study using JESS, with minimal internal fixation by lag screws in some cases, are comparable to the above studies using other types of external fixators with or without beaded olive wires, with an added advantage of JESS being its light weight, less bulk, inexpensive assembly and a relatively simple method of application. Eighty five percent of the patients in our study were observed to have excellent and good functional results (KSS score > 70). Except for one case of non union, no other significant complications were seen. The limitations of this study may have been a lack of direct comparison with other treatment methods. Hence, this study can provide a platform for a more detailed comparative study envisaging different treatment modalities in use for such fractures.
Conclusion
The findings from this study suggest that JESS is a useful, minimally invasive technique of fixation for the definitive management of high grade tibial plateau fractures without any significant complications; and is comparable to other types of external fixator systems being used for such fractures.