The tympanic cavity is an air-containing space within the temporal bone, which communicates with the nasopharynx through the eustachian tube and with the mastoid air cells by means of the tympanic antrum. It constitutes an extension of the upper respiratory tract and is subject to viral and bacterial invasion through eustachian tube. Pathology of ear is the third most common reason of visiting an otorhinolaryngologist, with inflammatory conditions of the middle ear being a frequent reason to prescribe antibiotics and perform surgery in children and teenagers [1].
Earlier, in majority of the cases, a diagnosis was made by clinical examination alone. However, with an increase in the prevalence of infective pathologies of the ear, it was suggested that the current approach to preventing and treating these conditions was not adequate. Therefore, especially in complicated and recurrent conditions, imaging plays an important role, as imaging findings may fundamentally influence the treatment [2,3].
With the advent of helical scanning techniques, CT is increasingly the imaging study of choice for definitive preoperative temporal bone imaging [4]. HRCT is widely used in diagnosis of inflammatory middle ear diseases, such as chronic otitis media or cholesteatoma and in evaluation of middle ear following mastoidectomy or tympanoplasty [5,6].
This prospective study aimed to study normal variations, congenital anomalies and infective pathologies of the temporal bone along with their complications on HRCT and to correlate these imaging findings surgically, wherever available.
Materials and Methods
The ethics committee of our institute approved this prospective study and an informed consent was taken from all patients included in it. The prospective study included 50 patients with clinically suspected temporal bone or ear pathologies. However patients with history of trauma and those with known or detected neoplasm related to temporal bone were excluded.
All the patients underwent a detailed clinical ENT examination followed by HRCT temporal bone. They were evaluated with Multidetector High Resolution Computed Tomography - SIEMENS SOMATOM EMOTION 6. No financial burden was incurred on the patient.
Scans were acquired in the helical mode to reduce motion artifacts. Scanning parameters of 130 kV, 150 mAs, 1-2 mm section thickness, 0.5 mm collimation were taken. With the patient in supine position, axial projections were obtained by serial 1-2 mm thin sections of the temporal bone with the line joining the infra-orbital rim and external auditory meatus perpendicular to the table. The images were reconstructed with a bone algorithm.
Coronal and sagittal reformatting was done to a slice thickness of 0.69 mm. Each HRCT image were analysed for specific features relevant to the evaluation of pathologies of temporal bone and interpreted in detail to define:
The type, location and extent of lesion.
Bony erosions of middle ear walls.
The integrity of the ossicular chain, facial nerve canal and labyrinth.
Involvement of hidden area, mastoid air cell system.
Results
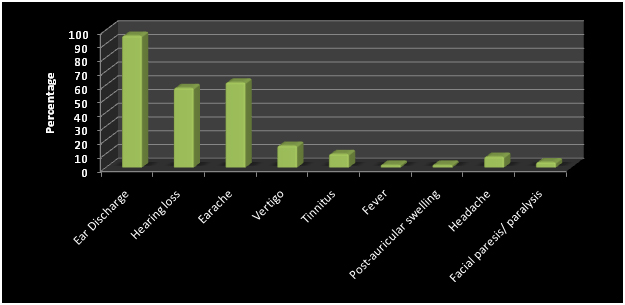
Out of 50 included cases in the study, surgical exploration was done in 46 cases. In this study, the youngest patient was of 3 months and the eldest was of 65 years. Fourteen patients (28%) belong to 11 -20 years of age group. [Table/Fig-1] shows the age distribution of patients. The most common presenting symptom was ear discharge. [Table/Fig-2] shows the presenting complaints of patients.
Age distribution of patient studied
| S.No. | Age Group | Number (n=50) | Percentage |
|---|
| 1. | <10 Years | 7 | 14% |
| 2. | 11-20 Years | 14 | 28% |
| 3. | 21-30 Years | 13 | 26% |
| 4. | 31-40 Years | 4 | 8% |
| 5. | 41-50 Years | 6 | 12% |
| 6. | 51-60 Years | 4 | 8% |
| 7. | >60 Years | 2 | 4% |
| Mean Age±SD (Range) in years | 27.95±16.85 (3 months-65 Years) |
Clinical symptoms of patients studied
Clinical/otoscopic findings of majority of cases were suggestive of active squamosal chronic otitis media (COM) in 54% cases followed by inactive squamosal chronic otitis media (COM) in 20%, active mucosal chronic otitis media (COM) in 16%, inactive mucosal chronic otitis media (COM) in 2%. Congenital anomalies were found in 8% patients (n=4).
On HRCT, Bilateral ear involvement was seen in 24% cases while 76 % had unilateral ear involvement. [Table/Fig-3] describes the HRCT findings seen in 50 cases. Of the 23 patients diagnosed with a soft tissue density in the epitympanum on HRCT, 20 patients belonged to the category of unsafe CSOM. There were 8 patients (16%) in which soft tissue density was seen involving epitympanum, mesotympanum, hypotympanum, aditus as well as antrum. Scutum was eroded in 21 patients on HRCT (42%) and was intact in 29 patients (58%). Among these, 19 (90.47%) patients had unsafe CSOM and 2 (9.52%) has safe CSOM.
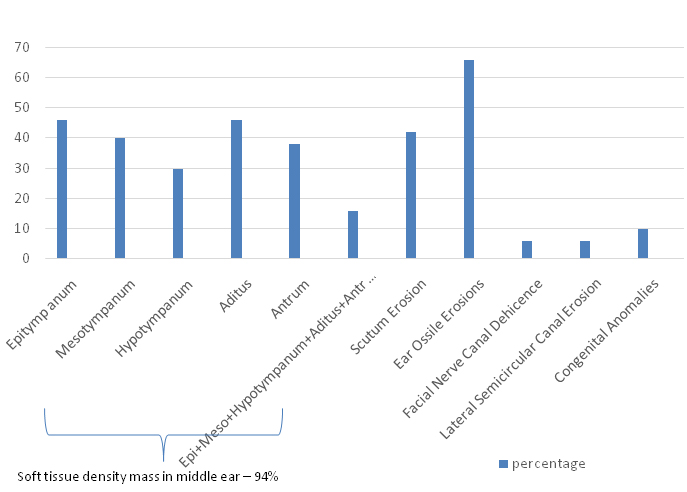
HRCT diagnosis of cholesteatoma was made in 30 patients. Out of these 30 patients, intraoperative findings of CSOM with cholesteatoma were seen in 25 (83.33%) and CSOM without cholesteatoma in 05 (16.66%). There were 25 patients that HRCT diagnosed accurately. Five patients were over diagnosed by HRCT. HRCT diagnosed facial canal dehiscence in 3 patients. Ossicular erosion was found in 33 patients on HRCT. During surgery, ossicular erosion was found in 31 patients. Correlation between HRCT and intraoperative findings in cholesteatoma, facial canal dehiscence and ossicular erosion is shown in [Table/Fig-4a&b] showing the sensitivity/ specificity in these respective entities.
Correlation between hrct and intra-operative findings
| HRCT Diagnosis (Positive in ‘n’ no. of patients) | Intraoperative findings (In ‘n’ no. of patients) |
|---|
| Positive | Negative |
|---|
| Cholesteatoma (n=30) | n=25 | n=5 |
| Facial canal dehiscence (n=3) | n=2 | n=1 |
| Ossicular erosion(n=33) | n=31 | n=2 |
Sensitivity/ specificty of HRCT
| HRCT Diagnosis | SENSITIVITY (%) | SPECIFICITY(%) |
|---|
| Cholesteatoma | 89.29 | 77.22 |
| Facial Canal Dehiscence | 33.33 | 97.50 |
| Ossicular erosion | 80.65 | 46.67 |
The lateral semicircular canal was found eroded in 3 (6%) cases and intact in 47 (94%) cases preoperatively. HRCT diagnosed congenital anomalies in 5 patients. Out of these, 3 patients were operated. Intra-operatively, isolated congenital aural atresia was found in 1 patient. Other 2 patients had congenital aural atresia associated with microtia, 1 of these 2 also having middle ear anomalies (abnormal ossicular chain). There was a 100% correlation between HRCT and intra-operative findings. Two patients refused surgery- one showed abnormal cochlea and other had semicircular canal malformations on HRCT.
Safe CSOM was diagnosed in 15 patients on HRCT. [Table/Fig-4c] shows correlation between HRCT and operative findings. Two patients were managed conservatively and the other 13 underwent surgery. Surgery confirmed safe CSOM in 10 patients and the other 3 turned out to be suffering from unsafe CSOM. Hence, there was a correlation of 76.92% between HRCT and surgical findings. Similarly, a correlation of 83.33% was found between HRCT and surgical findings for unsafe CSOM.
Correlation between HRCT and operative findings
| HRCT(n=50) | Operated cases(n=46) | Agreement with Intra-operative findings | Percentage |
|---|
| Congenital anomalies | 5 | 3 | 3 | 100% |
| Safe CSOM | 15 | 13 | 10 | 76.92% |
| Unsafe CSOM | 30 | 30 | 25 | 83.33% |
Discussion
HRCT imaging is necessary for anatomic determination of chronic otitis media, suspicion of congenital anomalies and to detect any loss of surgical landmarks caused by prior operation [7]. Watts et al., have shown that HRCT is less expensive and provides useful information about surgical trend [8] and, thus, if a co-ordination can be made between the otologist and radiologist with an appropriate familiarity of the surgeon with HRCT scans, preoperative imaging is essential and very helpful. Knowledge of the mastoid pneumatization aids in the planning of surgical approach e.g. whether to do canal wall down or up type of surgery [9].
Hence the present study was carried out with an aim to study any normal variation, congenital anomalies in the structure of temporal bone and to evaluate various infective pathologies of temporal bone and their complications with HRCT. In this prospective study carried out on 50 patients, the age of patients ranged from 3 months to 65 years. Mean age of patients was 27.95±16.85 years. CSOM is prevalent in all age groups; it particularly affects the patients in pediatric and younger age groups [10]. The most frequently encountered pathological process associated with unsafe type of CSOM is cholesteatoma [11]. Acquired cholesteatomas are commonly seen in patients less than 30 years [10]. In present study too, we found that the majority of patients were aged less than 30 years (n=34; 68%). which are similar to findings by Datta et al., [12]. Gerami et al., claim an average of 27.9±16.3 years [13]. Thus, most of the studies targeted to study temporal bone pathologies or normal variations have reported the mean age of patients between 25 to 30 years.
In the present study, majority of cases were males (n=29; 58%). Male to female ratio of study population was 1.38:1. Poursadegh et al., reported a male to female ratio of 1.39:1 [14]. Gerami et al., had a highly skewed male to female ratio of 2.48:1 [13]. With respect to CSOM being the major temporal bone pathology, no gender wise difference in prevalence of CSOM has been reported in community studies. However, in hospital based studies, a higher prevalence of males over females is reported in both safe and unsafe types [15].
In the present study, a total of 48 (96%) patients had active discharge. Majority had hearing loss (n=29; 58%) and pain in ear (n=31; 62%). In the series of Gomaa et al., chronic ear discharge with hearing loss was the main clinical presentation (60.7%). This probably indicates that the patients come to hospital relatively late and are reluctant for initial treatment [10].
Majority of cases (n=38; 76%) had unilateral involvement. Incidence of bilateral involvement has been reported variedly in literature. In a study by Gomaa et al., this incidence was only 3.57% [10]. In the present study, HRCT was able to provide excellent views of the mastoid air cells, antrum and aditus ad antrum in either coronal or axial planes. Mastoiditis was seen in 38 (76%) cases with majority being unilateral (n=25; 65.8%). Bilateral mastoiditis was seen in 12 (34.2%) cases. Chole et al., reported that mastoiditis is a common finding in cases with suspected temporal bone pathology and CSOM [15].
Congenital lesions of the temporal bone are quite rare [16]. The clinical diagnosis of congenial lesions is mainly based on the patient’s symptoms and manifestation only which might have a limited accuracy [17].
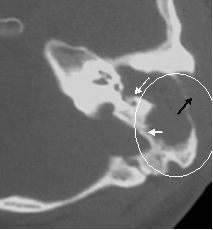
According to Mafee et al., the hallmark of cholesteatoma on HRCT is a soft tissue mass in attic and mastoid antrum associated with smooth bony expansion, scalloping of mastoid, erosion of lateral wall of attic (scutum) and erosion of ossicles [18] [Table/Fig-5]. However we could not distinguish cholesteatoma from other soft tissue disease. Walshe et al., in their study could not distinguish between mucosal disease and cholesteatoma [19]. Cholesteatoma characteristically causes bone erosion and when this feature was present in association with a soft tissue mass on CT, both Jackler et al., and O’Donoghue et al., found cholesteatoma to be present in 80% of cases explored [20,21]. Using the same criteria, we detected 25 out of 30 cases of cholesteatoma on surgical exploration.
Axial HRCT image showing soft tissue density mass in the left middle ear cavity and is extending into the mastoid antrum through the aditus (white square). Erosion of left sided ossicles and lateral cortical wall of mastoid is also seen (white arrow)

We thus diagnosed 30 patients as having cholesteatoma on HRCT. Johnson et al., emphasized that the presence of a well defined edge to a mass was a sure indication of cholesteatoma [22]. The sensitivity and specificity of HRCT to diagnose cholesteatoma preoperatively was 89.29% and 77.22% respectively in our study. We could correlate these findings with Jackler et al., who concluded sensitivity of 87% and specificity of 66% [20]. HRCT diagnosed facial canal dehiscence in 3 cases [Table/Fig-6]. Facial canal dehiscence was found to be present in 6 patients intraoperatively. There were only 2 patients that were accurately diagnosed by HRCT. We calculated a sensitivity of 33.33% and specificity of 97.50% for HRCT to diagnose facial canal dehiscence. This low sensitivity and relatively high specificity in our study could be correlated with Rai with sensitivity and specificity of 33.33% and 100% respectively [23]. Similar results were found by Alzoubi et al., Garber et al., and Garg et al., [24–26]. Gaurano et al., stated that preoperative demonstration of facial nerve canal involvement was often difficult not only because of the small size of the facial nerve canal but also due to its oblique orientation and the presence of developmental dehiscence, particularly when abutted by the soft tissue [27].
Axial HRCT image showing soft tissue density mass lesion causing erosion of the wall of the external auditory canal (white arrows), ear ossicles are absent and erosion of the tympanic segment of the facial nerve (black arrow)

In present study, HRCT could detect involvement of ear ossicles in form of medial displacement of the chain, fusion and hardening of the chain and erosion [Table/Fig-7] HRCT could correctly detect erosion in 31 cases out of 33. However, HRCT missed the involvement in 6 cases and overdiagnosed 8 cases. In 7 patients, ossicles were intact in both HRCT and intraoperatively. The sensitivity of HRCT, in the present study, for ossicular erosion was 80.65% and specificity was 46.67. Similar observations were concluded by Keskin et al., who reported their sensitivity, specificity of 80%, 46.1% respectively for ossicular erosion [28]. Visualization of ossicular chain sometimes becomes difficult owing to soft tissue around it. However, HRCT provides a good visualization which helps in detection of variances despite the presence of surrounding soft tissue.
Left extensive cholesteatoma. HRCT. axial cuts showing soft tissue density mass completely opacifying middle ear cavity. Mass is eroding ossicular chain, causing bony defect in the postero-lateral mastoid wall. The anterior limb of the left lateral semicircular canal is eroded
Lateral semicircular canal (LSCC) was found eroded in 3 cases [Table/Fig-7] and intact in 47 cases on HRCT. Of these, 46 underwent surgery and were available for evaluation. Of the 3 cases reported of having LSCC erosion on HRCT, only 2 showed erosions peroperatively and in the other 1 case, LSCC was found to be intact. However, all the 47 cases reported with intact LSCC on HRCT were found to be intact on surgical evaluation. The sensitivity and specificity of HRCT for LSCC erosion was found to be 100 % and 97.73% respectively. The positive predictive value and negative predictive value of HRCT was found to be 66.67% and 100% respectively. The findings were comparable to a study conducted by Prata et al., where the sensitivity and specificity was found to be 100% and 96.67% respectively and the positive and negative predictive values were 50% and 100% respectively [29]. As per Keskin et al., this could be attributed to the partial volume effects or may be the fact that at surgery the SCC bony contour could have not been reached [28].
Overall, the HRCT findings of present study indicated presence of congenital variances in 5 (10%), safe CSOM in 15 (30%) and unsafe CSOM with cholesteatoma in remaining 30 (60%) cases [Table/Fig-8].
Congenital microtia with external auditory canal atresia with fused ossicles. HRCT. Axial cut showing soft tissue density in middle ear cavitywith fused, laterally pushed ear ossicles and eac stenosis

In the present study, 5 cases were diagnosed as congenital anomaly on HRCT only three opted for corrective surgery. Nager et al., stated that atresia of the external auditory canal maybe an isolated anomaly [30]. This was consistent with our study where 1 patient had isolated congenital aural atresia on HRCT and the rest of the middle and inner ear structures were normal. This patient underwent canaloplasty and the findings were confirmed intraoperatively. According to Eavey et al., the most frequently encountered developmental anomaly of the external ear was microtia, also consistent with our study where 2 out of the 3 patients with congenital aural atresia has associated microtia [31]. These patients underwent plastic reconstruction of the auricle and external auditory canal. The patient with abnormal ossicular chain on HRCT also underwent exploration of the middle ear followed by ossicular reconstruction. Thus, our findings were confirmed intraoperatively.
Of the 15 patients diagnosed as safe CSOM on HRCT, 2 underwent conservative management. Of the remaining 13, surgical confirmation was achieved in 10 (76.92%) while 3 patients were found to have unsafe CSOM. Of the 30 patients diagnosed as having cholesteatoma on HRCT, 25 were confirmed on surgery (83.33%).
The other 5 patients were found to have unsafe pathology in the form of attic retraction pocket/attic granulation without cholesteatoma. Thus, HRCT showed a high agreement with surgical/final diagnosis. Despite high accuracy of HRCT, it underdiagnosed 3 cases of unsafe CSOM as safe CSOM, thus missing out the diagnosis of unsafe CSOM in 3/33 (9.1%) patients. Overall, HRCT showed an agreement with final diagnosis in 38/46 (82.6%) cases.
The results of present study thus indicated that HRCT is a useful modality through which pre-operative assessment of temporal bone pathologies can be done efficiently with a reasonable accuracy and precision for taking surgical decisions. Although, the present study has a limitation of sample size and showed that despite disagreement over some entities like facial canal dehiscence, the broad diagnosis of HRCT had a good agreement with surgical findings, thus indicating that prudent use of HRCT with a good clinical judgment provided a basis for preparation of a broad diagnosis that steered the surgical decisions in the right directions.
Recommendation
We recommend that the study should be done on large number of patients as well as at multiple centers.
Conclusion
Overall, the results of the present study showed a good agreement between HRCT and operative findings. HRCT temporal bone is an efficacious modality for accurate delineation of the anatomy and pathological involvement of temporal bone. We can hence conclude HRCT is useful for diagnosis, surgical planning and management of temporal bone pathologies.