Immunologic Cerebral Vasculitis and Extrapulmonary Tuberculosis: An Uncommon Association
Yiyi Wang1, Qian Li2, Xiaohan Zhen3, Yuan Liu4, Qi Wu5
1 Faculty, Department of Neurology, Tianjin Haihe Hospital, Tianjin, China.
2 Faculty, Department of Neurology, Tianjin Haihe Hospital, Tianjin, China.
3 Faculty, Department of Neurology, Tianjin Haihe Hospital, Tianjin, China.
4 Faculty, Department of Neurology, Tianjin Haihe Hospital, Tianjin China.
5 Faculty, Department of Respiratory, Tianjin Haihe Hospital, Tianjin, China.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Qi Wu, Tianjin Haihe Hospital, 890 Jingu Road, Jinnan, Tianjin 300350, P.R. China.
E-mail: wq572004@163.com
Infection can cause cerebral vasculitis not only by direct invasion of the vessel wall, but by immune complex deposition, or through secondary cryoglobulineamia. There are also two types of cerebral vasculitis associated with tuberculosis (TB). In TB treatment, cerebral vasculitis caused by immunologic injury received little attention than vasculitis due to direct invasion of TB infection. We report a case in a young woman who presented with fever, generalized lymphadenopathy, stroke-like events, movement disorder and coma, which was found to be active, lymph node TB with immunologic cerebral vacuities without tuberculosis meningitis.
Lymphatic tuberculosis, Intracranial multiple lesions, Coma
Case Report
A 24-year-old female sought treatment in the Outpatient Infection Clinic for fever along with generalized lymphadenopathy at the end of July 2014. Initial laboratory data showed a WBC count of 4.4 x 109/L, Platelets 322 x 109/ L, normal liver and renal function test results. ESR (Erythrocyte Sedimentation Rate) is at 50 mm/h. Three days later, on August 1, laboratory data revealed a WBC count of 5.52 x 109/ L, Platelets 379 x 109/L, Hgb at 98 g/L, an ESR level of 65 mm/h. Considering the possibility of autoimmune diseases, prednisone was used to treat fever. After one week, the fever was controlled and the drug is stopped. The initial chest film showed no definite active lung lesion.
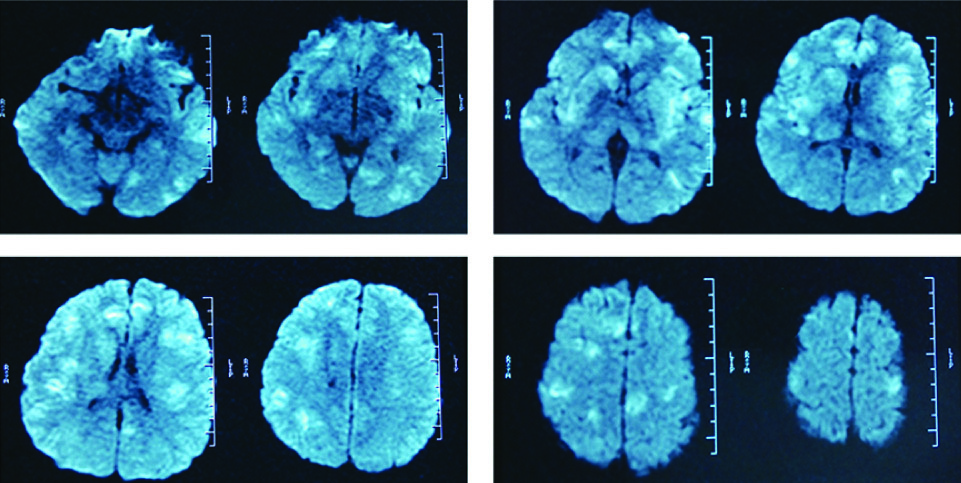
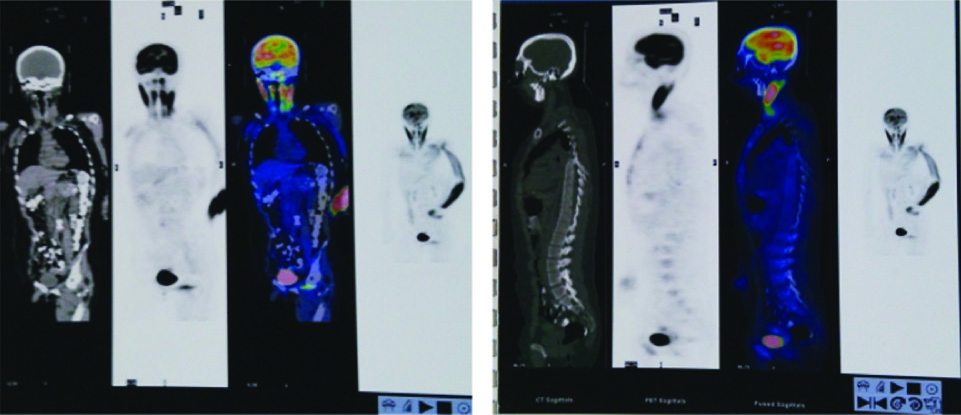
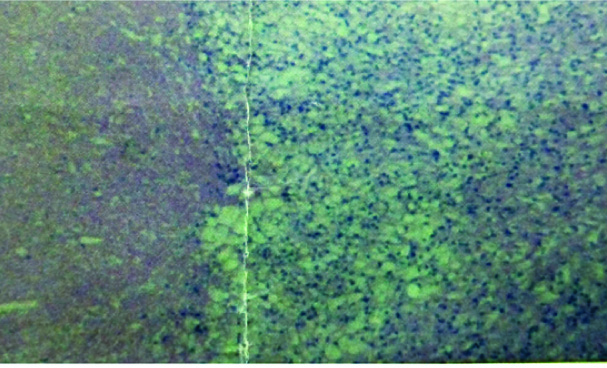
After one month, on August 25 2014, she developed drowsiness associated with fever. No history of headache, seizures, drug intake or contact with a patient of TB. The patient was admitted to hospital, when her condition got worse to coma. Physical examination revealed generalized lymphadenopathy and neurological examination revealed weakness in her right extremities and a positive Brudzinski’s sign on the right side without signs of peritoneal irritation, nausea or vomiting. Hematological and biochemical investigations revealed an increased ESR (82 mm/h) and C-reactive protein(13.09 mg/L) with a WBC count of 5.58 x 109/ L, PLT count of 422 x109/ L, Hgb at 104 g/L and normal glucose level, normal liver and renal function test results. Mantoux test was negative. Hepatitis B surface Ag, anti-Hepatitis C Virus, antinuclear antibody panel, ANCA, Anticardiolipin antibody, Anti-AQP4, ELISA for HIV, Venereal Disease Research Laboratory test for syphilis were also negative. The immunologic function revealed an increase in immunoglobulin (IgG: 1920 mg/dL, IgM: 495mg/dL), immune complexes (15.43U/ml) and a reduction of both C3 and C4 levels (C3: 78.3mg/dL, C4: 11.9mg/dL). The oligoclonal bands (OB) and TB-Ab of serum were of rhamnose positive, which indicated activation of auto immunity associated with TB infection. T-SPOT was at of negative. Cerebrospinal fluid (CSF) from a subsequent lumbar puncture revealed WBC of 8/mL, lactate level of 1.25mmol/L, protein level at 0.36 g/L, glucose level of 2.3 mmol/L, negative results on India ink staining, negative cryptococcal antigen test result, rhamnose positive on OB and an initial pressure of 184 mm H2O. Analysis of CSF was negative for bacterial culture, PCR-TBDNA, acid-fast staining. Serial CSF data at baseline and 6 month follow-up are presented in [Table/Fig-1]. Chest CT was normal. The brain magnetic resonance imaging (MRI) scan of the brain showed the multiple lesions with long TI, long T2 signal and DWI high intensity at the cerebral cortex medulla junction disturbed at cerebral hemisphere, bilateral basal ganglia and thalamus [Table/Fig-2]. Postcontrast T1W images showed intracranial small patchy slightly high signal on parietal lobe without abnormal meningeal enhancement. The PET scan showed multiple radioactive concentration were observed in bilateral cerebrum, cerebellum and neck multi-nodes [Table/Fig-3]. MRA and MRV of intracranial vessels were normal. The examination of a lmph node biopsy specimen showed lymph node tuberculosis [Table/Fig-4].
Serial CSF data at baseline and 6 month follow-up
| Date | WBC(106/L) | Pro(g/L) | Glu(mmol/L) | Cl(mmol/L) | ADA(U/L) | Lac(mmol/L) |
|---|
| 08.27.2014 | 8 | 0.36 | 2.3 | 122 | 4 | 1.25 |
| 10.08.2014 | 0 | 0.6 | 2.9 | 124 | 2.1 | 1.26 |
| 10.29.2014 | 0 | 0.45 | 3.4 | 121 | – | – |
| 11.21.2014 | 0 | 0.48 | 2.8 | 126 | – | – |
| 01.09.2015 | 0 | 0.29 | 3.5 | 119 | 0.4 | 1.68 |
These data showed that no obvious abnormal except the slight decrease in CSF glucose levels at baseline
(WBC: White blood cell; Pro: Protein; Glu: Glucose; Cl: Chloride; ADA: Adenosine deaminase; Lac:lactic acid.)
MRI scan of the brain showed the multiple lesions with DWI high intensity
The PET scan showed multiple radioactive concentration were observed in bilateral cerebrum, cerebellum and neck multi-nodes
The examination of a LYMPH node biopsy specimen showed lymph node tuberculosis
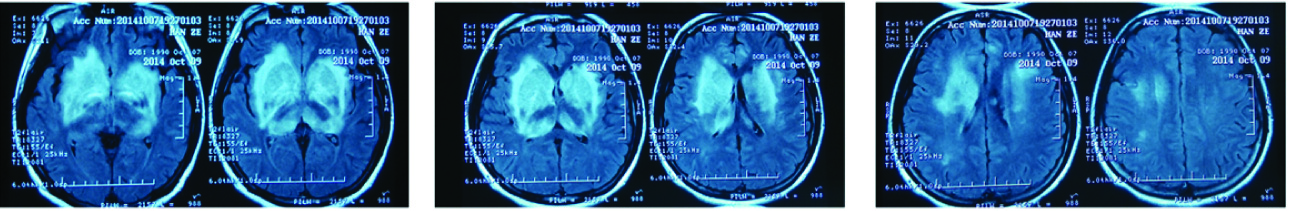
The patient was diagnosed as active, lymph node TB with secondry cerebral vasculitis. Intravenous immunoglobulin (0.4 mg/kg/day for 5 days), glucocorticoid pulse therapy (Methyl prednisone at 500mg for 5 days) and anti-tuberculous treatment with Rifampicin (450 mg/day), Isoniazid (300 mg/day), Ethambutol (75 mg/day) and pyrazinamide (1500 mg/day) (HERZ) were instituted. The patient recovered consciousness after five days, leaving decline in limbs strength, muscle morphology, dysarthria, dystonia and abnormal emotion. After one month, MRI scan of the brain showed abnormal signals at the cerebral cortex medulla junction were less, but in bilateral basal ganglia abnormal signals were obvious [Table/Fig-5], Intravenous immunoglobulin (0.4 mg/kg/day for 5 days) and glucocorticoid pulse therapy (Methyl prednisone 1g/day for 3 days) were administered. During this period, the patient complained sacroiliac pain. CT scan of the pelvis showed a sacral lytic lesion. The patient was diagnosed as sacral bone tuberculosis.
MRI scan of the brain after one month
Discussion
Central nervous system (CNS) vasculitis is inflammation of blood vessel walls in the brain or spine, which can cause a loss of brain function and in some cases, which is life-threatening. Vasculitis of CNS can be classified as primary and secondary subtype. Vasculitis can occur as a direct complication of inflammatory autoimmune conditions whose primary histopathologic characteristic is notvasculitic [1], which is secondary vasculitis. About the pathogeny of secondary subtype, it is well known that it often occurs in the following situations: accompanied by other autoimmune diseases such as systemic lupus erythematosus; infection, such as viral or bacterial; systemic vasculitic disorders such as Wegener’s granulomatosis.
Infection can cause vasculitis not only by direct invasion of the vessel wall, but by immune complex deposition, or through secondary cryoglobulineamia [1]. As a kind of vasculitis caused by infection, there are two types of cerebral vasculitis associated with TB: 1). Direct invasion: The basal exudates cause inflammatory changes in the vessels predominantly involving the circle of Willis. At first, the vessel wall is involved, in turn, subendothelial cells, leading to stenosis of the vascular lumina and thrombus formation. MRA has a typical appearance with enhancement of the basal meninges, narrowing of the basal cerebral or cortical vessels and possible multiple small infarctions from the resultant vasculitis [2]. This type of vasculitis is a catastrophic complication of tuberculous meningitis(TBM) [3]; 2) Immunologic injury: the deposit of tuberculoprotein immune complexes in the small vessel walls led the inflammatory changes of small cerebral vessels, whose levels depend on the disease activity [4]. Hepatitis B, Epstein-Barr virus can all cause vasculitis by a similar mechanism [5]. It is also possible that antibodies are formed against the M. tuberculosis antigens in the host, rather than the induction of the cell mediated mechanisms (type IV) hypersensitivity. On MRI, they may present with stroke-like lesions from spasm or occlusion and round abnormal intensities on T2 or FLAIR [6]. In clinical practice, cerebral vasculitis caused by infection direct invasion receives more attention than immunologic cerebral vasculitis. Despite a high prevalence of tuberculosis (TB) in China, reports of TB clinically presenting with immunologic cerebral vasculitis are scarce and prevalence of which in relation to TB has not been notified. There is no relevant data in the literature.
Clinical and radiological diagnosis of cerebral vasculitis is challenging as there is no vasculitis-specific symptom or imaging sign. Clinical features of acute cerebral vasculitis include headaches seizures (focal/generalized) and stroke-like events. Sub-acute cerebral vasculitis include encephalopathy, progressive cognitive change and chronic cerebral vasculitis include movement disorders, especially chorea, myoclonus. Mean while, acute or subacute encephalopathy commonly present an acute confusional state, progressing to drowsiness and coma [7]. The patient presented with stroke-like events cognitive change and coma at acute stage and movement disorder at chronic stage. Systemic features including fever, night sweats were most evident.
No leptomeningeal biopsy for the condition, imaging diagnostic tests plays an important role in the diagnosis of cerebral vasculitis. Imaging can be used to evaluate the vessels for inflammatory changes or to investigate changes in the adjacent brain parenchyma [8]. There is no specific imaging sign for immunologic cerebral vasculitis, however, multiple infarcts of different ages in various vascular territories are suggestive of cerebral vasculitis, in particular in young patients.
Conclusion
We described a case of TB immunologic cerebral vasculitis without TBM complicated with lymph node tuberculosis and sacral bone tuberculosis. Cerebral vasculitis related TBM has been reported in the literature, but to our knowledge this is the first case report to describe an immunologic cerebral vasculitis triggered by TB infection. This report delineates the association between immunologic cerebral vasculitis and TB emphasizing that diligent search for TB must be carried out in all cases of cerebral vasculitis, especially in developing countries with high prevalence of TB. Early diagnosis is of importance since the devastating symptoms of CNS vasculitis are reversible partially even completely with correct and timely treatments. Corticosteroids are the corner stone of therapy for cerebral vasculitis. The prolonged high-dose therapy and gradual withdrawal of systemic corticosteroids should be considered considering the three stages of this secondary cerebral vasculitis: acute, sub-acute and chronic stage.
These data showed that no obvious abnormal except the slight decrease in CSF glucose levels at baseline
(WBC: White blood cell; Pro: Protein; Glu: Glucose; Cl: Chloride; ADA: Adenosine deaminase; Lac:lactic acid.)
[1]. Scolding NJ, Central nervous system vasculitisSemin Immunopathol 2009 31(4):27-36. [Google Scholar]
[2]. Hähnel S, Inflammatory Diseases of the Brain [M] 2009 New YorkSpringer:25-50. [Google Scholar]
[3]. Joseph FG, Scolding NJ, Cerebral vasculitis: a practical approac [M]Pract Neurol 2002 2:80-93. [Google Scholar]
[4]. Johnson NM, Circulating immune complexes in tuberculosisThorax 1981 36(8):610-17. [Google Scholar]
[5]. Scolding NJ, The recognition, diagnosis and management of cerebral vasculitis: a European surveyEur J Neurol 2002 9(4):343-47. [Google Scholar]
[6]. Castro Caldas A, Central nervous system vasculitis associated with hepatitis C virus infection: a brain MRI-supported diagnosisJ Neurol Sci 2014 336(1-2):152-54. [Google Scholar]
[7]. Berlit P, Steinbrecher A, [Cerebral vasculitis]Fortschr Neurol Psychiatr 2002 70(12):663-77. [Google Scholar]
[8]. Gomes LJ, The role of imaging in the diagnosis of central nervous system vasculitisCurr Allergy Asthma Rep 2010 10(3):163-70. [Google Scholar]