Desensitizing Agent Reduces Dentin Hypersensitivity During Ultrasonic Scaling: A Pilot Study
Tomonari Suda1, Hiroaki Kobayashi2, Toshiharu Akiyama3, Takuya Takano4, Misa Gokyu5, Takeaki Sudo6, Thatawee Khemwong7, Yuichi Izumi8
1 Reseach Associate, Peirodontology, Department of Bio-Matrix, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan.
2 Lecturer, Peirodontology, Department of Bio-Matrix, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan.
3 Registered Dentist, Periodontology, Department of Bio-Matrix, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan.
4 Research Student, Periodontology, Department of Bio-Matrix, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan.
5 Graduate Student, Periodontology, Department of Bio-Matrix, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan.
6 Graduate Student, Periodontology, Department of Bio-Matrix, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan.
7 Graduate Student, Periodontology, Department of Bio-Matrix, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan.
8 Professor, Periodontology, Department of Bio-Matrix, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hiroaki Kobayashi, Lecturer, Periodontology, Bio-Matrix Department, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan, 1-5-45 Yushima, Bunkyo-ku, Tokyo 113 - 8549, Japan. E-mail : h-kobayashi.peri@tmd.ac.jp
Background
Dentin hypersensitivity can interfere with optimal periodontal care by dentists and patients. The pain associated with dentin hypersensitivity during ultrasonic scaling is intolerable for patient and interferes with the procedure, particularly during supportive periodontal therapy (SPT) for patients with gingival recession.
Aim
This study proposed to evaluate the desensitizing effect of the oxalic acid agent on pain caused by dentin hypersensitivity during ultrasonic scaling.
Materials and Methods
This study involved 12 patients who were incorporated in SPT program and complained of dentin hypersensitivity during ultrasonic scaling. We examined the availability of the oxalic acid agent to compare the degree of pain during ultrasonic scaling with or without the application of the dentin hypersensitivity agent. Evaluation of effects on dentin hypersensitivity was determined by a questionnaire and visual analog scale (VAS) pain scores after ultrasonic scaling. The statistical analysis was performed using the paired Student t-test and Spearman rank correlation coefficient.
Results
The desensitizing agent reduced the mean VAS pain score from 69.33 ± 16.02 at baseline to 26.08 ± 27.99 after application. The questionnaire revealed that >80% patients were satisfied and requested the application of the desensitizing agent for future ultrasonic scaling sessions.
Conclusion
This study shows that the application of the oxalic acid agent considerably reduces pain associated with dentin hypersensitivity experienced during ultrasonic scaling. This pain control treatment may improve patient participation and treatment efficiency.
Oxalic acid, Periodontal health, SPT
Introduction
Dentin hypersensitivity is frequently caused by denudation of root surfaces during periodontal treatment [1, 2]. This pain sensation is caused by thermal, chemical, mechanical, or osmotic stimuli [3]. During the therapy, gingival tissue recession and extensive root planing may trigger symptoms of dentin hypersensitivity. Because patients with periodontal disease experience progressive alveolar bone loss, many patients experience dentin sensitivity. Approximately half of the patients experience dentin hypersensitivity after scaling and root planning [4]. This symptom generally interferes with ultrasonic scaling in Supportive Periodontal Therapy (SPT), which may result in the accumulation of dental plaque and negatively influence the prognosis after periodontal therapy.
The hydrodynamic theory proposed by Brännström [5] is the most accepted mechanism of dentin hypersensitivity [6]. Thermal, tactile, or chemical stimuli on the exposed root surface affect fluid flow within the dentinal tubules, generating a neural response in the pulp. The severity of dentin hypersensitivity increases with the number of wider diameter open dentinal tubules [7]. Therefore, it is important to prevent the development of dentin hypersensitivity during periodontal treatment. Different types of materials have been designed for dental pulp stimulation, such as bonding adhesive, glutaraldehyde and oxazlate [8].
Ultrasonic scaling is an essential procedure during periodontal therapy [9] because it effectively eliminates supra- and sub-gingival plaque or calculus [10,11]. Several sessions are crucial to prevent recurrence of periodontal infection during maintenance therapy. However, some patients dislike receiving ultrasonic scaling because of worsening dentin hypersensitivity. In addition, patients’ pain reactions during the treatment makes dental professionals hesitate to attach the scaling tip to the root surface, which interferes with maintenance therapy. Therefore, studies aiming to reduce dentin hypersensitivity during ultrasonic scaling may contribute to maintain periodontal health.
The aim of this study was to evaluate the efficacy of oxalic acid application as a desensitizing agent immediately before ultrasonic scaling to reduce the development of dentin hypersensitivity during the subsequent maintenance program.
Materials and Methods
A total of 2,460 patients who received periodontal maintenance at the periodontal department of the Tokyo Medical and Dental University Hospital from August 2011 to April 2012 were examined. Twelve patients with an age range between 39-77 years (mean age = 59±11) participated in this study. They completed periodontal active therapy, such as scaling and root planning and periodontal surgery, more than 6 months before. The inclusion parameters were as follows. They must have a minimum of 20 teeth, including some with dentin hypersensitivity. Selected teeth did not have the lesions, such as caries, erosion or wedge-shaped defect and was included 5 incisors, 3 canines and 4 molars. These patients should have plaque and calculus removed by ultrasonic scaler during periodontal maintenance and complained of dentin hypersensitivity.
Following enrollment, the patients were examined for probing pocket depth (PPD), clinical attachment level (CAL), recession (REC), tooth mobility, bleeding on probing (BOP), gingival index (GI) [12] and plaque index (PlI) [13] of the tooth with hypersensitivity. After clinical examination, they received ultrasonic scaling and indicated the amount of pain related to this treatment using a visual analog scale (VAS) [14]. This score was considered the baseline VAS value. VAS was 10-cm long, with indications of “no pain” and “intolerable pain” on the left and right end, respectively.
During the next appointment, each patient received the same treatment immediately after the application of the oxalic acid desensitizing agent (Super Seal®, Phoenix Dental Inc., US). First, cotton rolls are placed on the vestibule and plaque and saliva were subsequently removed from teeth surface using a swab. Cotton pellets saturated with the agent were gently rubbed on one sensitive tooth for 5 seconds. Following application, this situation was kept on for one minute. Subsequently, ultrasonic scaling was initiated, during which the patients were again asked to record their sensitivity level using the 10-cm VAS (post-application VAS value). The ultrasonic scalers used in this study was selected one of the following devices: Solfy (J. Morita Corp., Tokyo, Japan), ENAC (Osada Electric Co., Tokyo, Japan), and Mini Piezo (EMS, Nyron, Switzerland). The patients were treated with the same device and same settings in both treatments by the same investigator. The power setting of each ultrasonic scaler was operated at the minimum. After clinical examination, they filled out a questionnaire involving questions on this agent.
Ethics: This study was approved by the Ethics Committee of the School of Dentistry, Tokyo Medical and Dental University (No. 659). All experiment was performed after obtaining written informed consent from the patients.
Statistical Analysis
The mean baseline and post-application VAS values of the 12 patients were compared using the paired Student t-test with Statview software (SAS Institute Inc. Cary, NC, USA). The p-values <0.05 were considered statistically significant. Spearman rank correlation coefficient was used to determine possible correlation between the degree of VAS value and clinical value, such as CAL and REC.
Results
[Table/Fig-1] presents the clinical parameters of the tooth evaluated in each patient and the VAS values measured at baseline and after application of dentine desensitizer. Mean PPD was 1.92 mm and mean CAL was 4.33 mm. Gingival recession was observed in almost all teeth. Most patients received periodontal maintenance at 3–6-month intervals and were able to achieve adequate levels of plaque control and gingival condition.
Cilinical parameters of all subjects in this study
| Subject | Tooth No. | PPD | CAL | REC | BOP | GI | PlI | mobility | VAS score |
|---|
| baseline | post application |
|---|
| A | 31 | 2 | 9 | 7 | 1 | 2 | 2 | 0 | 75 | 1 |
| B | 31 | 2 | 3 | 1 | 0 | 0 | 0 | 0 | 76 | 13 |
| C | 23 | 1 | 2 | 1 | 0 | 0 | 0 | 0 | 70 | 2 |
| D | 41 | 2 | 3 | 1 | 0 | 0 | 0 | 0 | 44 | 2 |
| E | 11 | 3 | 8 | 5 | 0 | 1 | 1 | 0 | 91 | 67 |
| F | 13 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 48 | 25 |
| G | 13 | 2 | 4 | 2 | 0 | 0 | 0 | 0 | 68 | 3 |
| H | 36 | 1 | 2 | 1 | 0 | 0 | 0 | 0 | 59 | 5 |
| I | 16 | 1 | 3 | 2 | 0 | 0 | 0 | 0 | 80 | 25 |
| J | 26 | 2 | 4 | 2 | 0 | 0 | 0 | 0 | 59 | 32 |
| K | 26 | 3 | 9 | 6 | 0 | 1 | 1 | 1 | 98 | 81 |
| L | 31 | 2 | 3 | 1 | 1 | 2 | 1 | 0 | 64 | 57 |
| Mean | 1.92 | 4.33 | 2.42 | 0.17 | 0.50 | 0.42 | 0.08 | 69.33 | 26.08* |
| SD | 0.67 | 2.71 | 2.27 | 0.39 | 0.80 | 0.67 | 0.29 | 16.02 | 27.99 |
BOP, bleeding on probing [positive (1); negative (0)]; CAL, clinical attachment level; GI, gingival index; PlI, plaque index; PPD, probing pocket depth; VAS, visual analog scale. *Statistical difference between VAS scores during ultrasonic scaling at baseline and post-application of the desensitizer (paired t-test; p<0.05)
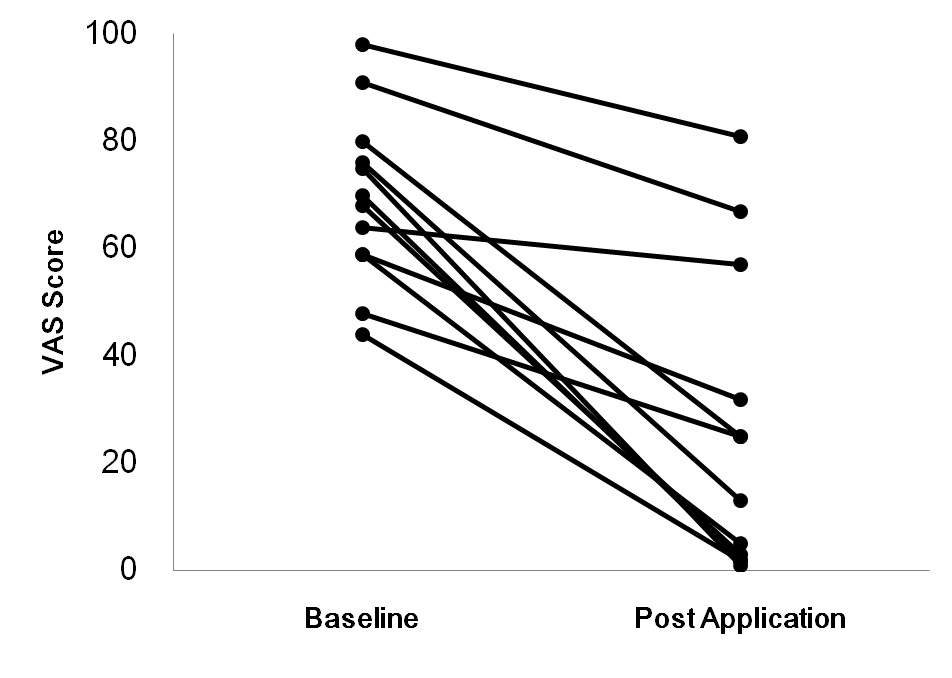
Overall, the application of the desensitizing agent immediately before ultrasonic scaling reduced the pain level to approximately 60% of baseline [Table/Fig-1]. The mean VAS score was 69.33 ± 16.02 at baseline compared with 26.08 ± 27.99 after application (p < 0.05). Furthermore, all patients experienced a reduction in VAS score in the presence of the desensitizing agent [Table/Fig-2]. We analysed the relationship between clinical parameter and improving value of VAS score. The difference between the baseline VAS value and the post-application VAS value was used as improving score of VAS value. Clinical parameters including CAL and REC were not related with improving score of VAS value (p=0.9906 and p=0.4793, respectively).
Changes in VAS value between the baseline and after application of the desensitizer. Each dot represents individual VAS values. Lines connect the VAS values from the same individual
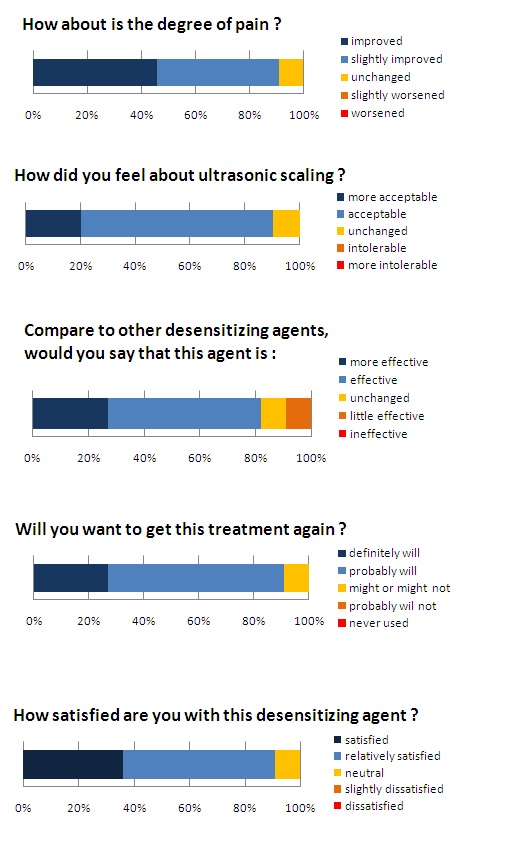
The satisfaction questionnaire, presented as stacked bar charts [Table/Fig-3], confirmed that approximately 45% subjects experienced a noticeable (improved) decrease in pain intensity during ultrasonic scaling in the presence of desensitization agent, and approximately 90% were satisfied or relatively satisfied by the treatment. The use of this desensitization agent rendered most patients (approximately 90%) less apprehensive at the idea of their next ultrasonic scaling and willing to repeat this treatment. This study suggests that the application of the desensitization agent on the denuded roots considerably reduces hypersensitivity during ultrasonic scaling treatment, which would improve patient participation and treatment efficiency.
The results of the satisfaction questionnaires
Stacked bar charts depicting the percentage of respondents filled out after this study
Discussion
After the periodontal procedures, optimal plaque control is necessary to maintain adequate periodontal conditions [15]. Most patients suffer from dentin hypersensitivity caused by denuded root surface after nonsurgical and surgical therapy with a prevalence of 62%–90% and from 77%–80%, respectively. The intensity of root sensitivity increases during the first 1–3 weeks following therapy and subsequently subside over time [16]. It was reported that meticulous plaque control after periodontal treatment reduces root hypersensitivity [17]. However, this clinical study selected the very restricted patients, who received periodontal maintenance therapy for more than 6 months and were complaining of discomfort every ultrasonic scaling. Accordingly, it is thought that the regression effect of dentin hypersensitivity might be small. In addition, all patients receiving SPT maintained good periodontal health (mean PD = 1.92, mean GI = 0.50, mean PlI = 0.42) and teeth without the substantial tooth loss, such as caries, erosion, and wedge-shaped defect was selected. The degree of attachment loss and recession was not also related the improving score of VAS value. Therefore, the results of the present study were not affected by periodontal disease and tooth conditions. The present study tested the pain relief capacity of the dentin desensitizer during ultrasonic scaling. Following application of the dentine desensitizer, a 60% reduction in self-reported pain was observed, and >80 % subjects were satisfied with this treatment. The treatment evaluation of the desensitizer was operated on a different day to avoid a change in sensitivity by repeated painful stimulation [3].
Various dentin desensitizers have been proven effective for dentin hypersensitivity [18]. In this study, an oxalic acid potassium salt desensitizing agent was used because of its easy application and immediate effectiveness. This agent reacts with the calcium in the dentinal tubules to form insoluble calcium oxalate crystals which occlude the dentinal tubules [19]. This agent is easy to use without any device and can be applied within seconds before ultrasonic scaling procedure.
Limitations
This study has two major limitations. It was conducted with a small number of patients and without a placebo group. The intensity of the pain from hypersensitivity is different among individuals and sites. So, this clinical study evaluated the effect of desensitizing agent between before and after application. But a double blind, randomized, controlled study with placebo should be required to correctly evaluate the desensitizing effect of the dentine desensitizer during ultrasonic scaling [3]. Furthermore, the questionnaire used in this study should be confirmed about validity and reliability. Many clinical trials of various desensitizing agents have been published and reported the placebo effect. It was observed that the pain reductions by placebo were 30-40% range in these trials. However, the application of desensitizing agent before ultrasonic scaling made over 60% pain reductions and that effect was enough to show the usefulness. In addition, intensity of dentin hypersensitivity in this study was evaluated by ultrasonic scaling. This method is reproducible to evaluate the pain intensity and directly indicates the effect of applying the desensitizer before ultrasonic scaling.
Conclusion
The application of the desensitizing agent before ultrasonic scaling considerably reduced the pain due to dentin hypersensitivity. This application may constitute a useful pain relief approach for dentin hypersensitivity and improve the efficiency of supportive periodontal therapy. Randomized controlled trial with placebo group is needed to verify this method.
BOP, bleeding on probing [positive (1); negative (0)]; CAL, clinical attachment level; GI, gingival index; PlI, plaque index; PPD, probing pocket depth; VAS, visual analog scale. *Statistical difference between VAS scores during ultrasonic scaling at baseline and post-application of the desensitizer (paired t-test; p<0.05)
[1]. Chabanski MB, Gillam DG, Bulman JS, Newman HN, Clinical evaluation of cervical dentine sensitivity in a population of patients referred to a specialist periodontology department: a pilot studyJ Oral Rehabil 1997 24(9):666-72. [Google Scholar]
[2]. Taani SD, Awartani F, Clinical evaluation of cervical dentin sensitivity (CDS) in patients attending general dental clinics (GDC) and periodontal specialty clinics (PSC)J Clin Periodontol 2002 29(2):118-22. [Google Scholar]
[3]. Holland GR, Narhi MN, Addy M, Gangarosa L, Orchardson R, Guidelines for the design and conduct of clinical trials on dentine hypersensitivityJ Clin Periodontol 1997 24(11):808-13. [Google Scholar]
[4]. von Troil B, Needleman I, Sanz M, A systematic review of the prevalence of root sensitivity following periodontal therapyJ Clin Periodontol 2002 29(Suppl 3):173-7.discussion 195-96 [Google Scholar]
[5]. Brannstrom M, Sensitivity of dentineOral Surg Oral Med Oral Pathol 1966 21(4):517-26. [Google Scholar]
[6]. Addy M, Pearce N, Aetiological, predisposing and environmental factors in dentine hypersensitivityArch Oral Biol 1994 39(Suppl):33S-38S. [Google Scholar]
[7]. Absi EG, Addy M, Adams D, Dentine hypersensitivity. A study of the patency of dentinal tubules in sensitive and non-sensitive cervical dentineJ Clin Periodontol 1987 14(5):280-84. [Google Scholar]
[8]. Cunha-Cruz J, Wataha JC, Zhou L, Manning W, Trantow M, Bettendorf MM, Treating dentin hypersensitivity: therapeutic choices made by dentists of the northwest PRECEDENT networkJ Am Dent Assoc 2010 141(9):1097-1105. [Google Scholar]
[9]. Oda S, Nitta H, Setoguchi T, Izumi Y, Ishikawa I, Current concepts and advances in manual and power-driven instrumentationPeriodontol 2000 2004 36:45-58. [Google Scholar]
[10]. Tunkel J, Heinecke A, Flemmig TF, A systematic review of efficacy of machine-driven and manual subgingival debridement in the treatment of chronic periodontitisJ Clin Periodontol 2002 29(Suppl 3):72-81.discussion 90-91 [Google Scholar]
[11]. Ioannou I, Dimitriadis N, Papadimitriou K, Sakellari D, Vouros I, Konstantinidis A, Hand instrumentation versus ultrasonic debridement in the treatment of chronic periodontitis: a randomized clinical and microbiological trialJ Clin Periodontol 2009 36(2):132-41. [Google Scholar]
[12]. Löe H, Silness J, Periodontal Disease in Pregnancy. Prevalence and SeverityActa Odontol Scand 1963 21:533-51. [Google Scholar]
[13]. Silness J, Löe H, Periodontal DIsease in Pregnancy. Correlation between Oral Hygiene and Periodonatl ConditionActa Odontol Scand 1964 22:121-35. [Google Scholar]
[14]. Price DD, McGrath PA, Rafii A, Buckingham B, The validation of visual analogue scales as ratio scale measures for chronic and experimental painPain 1983 17(1):45-56. [Google Scholar]
[15]. Axelsson P, Lindhe J, The significance of maintenance care in the treatment of periodontal diseaseJ Clin Periodontol 1981 8(4):281-94. [Google Scholar]
[16]. Lin YH, Gillam DG, The Prevalence of Root Sensitivity following Periodontal Therapy: A Systematic ReviewInt J Dent 2012 2012:407023 [Google Scholar]
[17]. Tammaro S, Wennstrom JL, Bergenholtz G, Root-dentin sensitivity following non-surgical periodontal treatmentJ Clin Periodontol 2000 27(9):690-97. [Google Scholar]
[18]. Lin PY, Cheng YW, Chu CY, Chien KL, Lin CP, Tu YK, In-office treatment for dentin hypersensitivity: a systematic review and network meta-analysisJ Clin Periodontol 2013 40(1):53-64. [Google Scholar]
[19]. Kolker JL, Vargas MA, Armstrong SR, Dawson DV, Effect of desensitizing agents on dentin permeability and dentin tubule occlusionJ Adhes Dent 2002 4(3):211-21. [Google Scholar]