Mesenchymal Hamartoma of Chest Wall in an Infant: Mimicking Persistent Pneumonia
Amitabh Singh1, Rachna Seth2, Gautham Pai3, Lesa Dawman4, Amit Satapathy5
1 Senior Research Associate, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India.
2 Additional Professor, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India.
3 Senior Resident, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India.
4 Senior Resident, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India.
5 Senior Resident, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rachna Seth, Additional Professor, Department of Pediatrics, All India Institute of Medical Sciences, Ansari Nagar, New Delhi, India. E-mail : drrachnaseth@yahoo.co.in
Mesenchymal Hamartoma of the chest wall (MHCW) is a very rare benign tumour. They are usually discovered in infancy. Spontaneous regression is known to occur in this benign condition. Management is surgical removal of mass if respiratory compromise is present. Conservative management is preferred modality in asymptomatic children as malignant transformation is not reported. Herein, we present a case of MHCW in a 5 month old infant presenting with acute respiratory distress with history of respiratory problem at 3 months of age. Child was suspected to have persistent pneumonia in view of radiological findings. Child’s respiratory distress improved with antibiotics and bronchodilators. Respiratory symptoms in MHCW are due to extrinsic compression of lung parenchyma. Present case had respiratory symptoms with persistent radiological findings leading to suspicion of persistent pneumonia. His respiratory symptoms and exacerbation on follow up was attributed to hyper reactive airway disease and MHCW was managed conservatively. The non-neoplastic nature, characteristic presentation, histopathology, imaging modality and management options of MHCW are discussed.
Benign chest wall mass, Benign tumour, Persistent pneumonia
Case Report
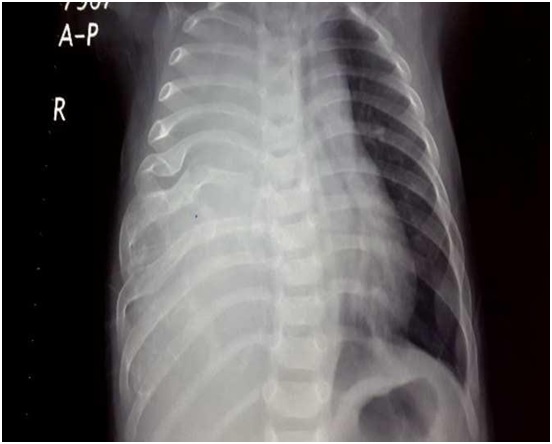
A five-month-old infant presented with complaints of recurrent cough, cold, fast breathing since 2 months of age. At presentation, child had fast breathing, fever, chest retraction and poor oral intake. There was positive history of asthma in the family. Physical examination revealed marked tachypnea with subcostal, intercostal retractions and decreased air entry over right lower lung field with bilateral wheeze. There was a hard mass palpable in the anterior region of chest overlying the 5th, 6th and 7th ribs on right side. Systemic examination was unremarkable except for the respiratory findings. Clinical possibilities kept were community acquired pneumonia with underlying collapse consolidation, pulmonary agenesis and malignant neoplasm arising from rib. As child was symptomatic since two months of age, causes of persistent pneumonia like congenital anomaly of airways, tuberculosis, cystic fibrosis, immunodeficiency was also kept. Chest X- ray revealed opacity of right lung with deformed 5th, 6th, 7th ribs raising the suspicion of a malignant lesion [Table/Fig-1]. USG thorax showed 5 x 6 cm soft tissue mass in the parietal wall.
Chest X-ray right lung opacity with distortion of 5th, 6th 7th ribs
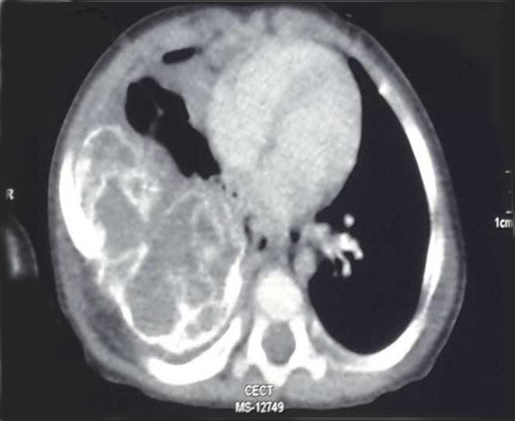
Child was managed with bronchodilators, antibiotics and oxygen inhalation. There was marked improvement in respiratory distress with these measures. CECT finding pointed towards a diagnosis of mesenchymal hamartoma of chest wall [Table/Fig-2]. As child showed marked response to bronchodilator therapy (salbutamol nebulization), a possibility of underlying hyperreactive airway disease was also kept. FNAC from the mass showed clusters of spindle cells admixed with richly vascular chondromyxoid stroma. Bone scan showed homogenous radiotracer uptake in right thoracic mass. A biopsy from chest wall showed fragments of cellular cartilage surrounded by spindle shaped mesenchymal cells. Paediatric surgery opinion was obtained. As the child’s respiratory distress settled, it was decided to keep him under close observation with periodic imaging. The child has been followed up for one year with two episodes of exacerbation of respiratory symptoms responding to medical measures and growth percentiles between 25th and 50th for the normal population.
CECT Chest-large chest wall based heterogeneous lesion with matrix calcification and remodeling of underlying ribs with multiple enhancing septations
Discussion
McLeod and Dahlin in 1979 gave the present accepted nomenclature of Mesenchymal hamartoma [1], Mesenchymoma, Infantile cartilaginous hamartoma [2] and infantile osteochondroma are other names used for this entity in the past.
Mesenchymal hamartomas are not true neoplasm, at times they have been classified as non-neoplastic development anomaly. It generally presents in neonates and infants [3], arising antenatally. Most of the times, a diagnosis on prenatal USG is possible. Origin is from ribs usually and may be multifocal [4]. It is almost always of congenital origin [5]. It has M:F ratio of 2:1. Chest wall deformity or mass and respiratory distress are usual presentation [6].
Recurrent respiratory symptoms with persistent radiological finding may raise the possibility of persistent pneumonia. At the same time if underlying respiratory symptoms are due to any other underlying condition, the respiratory symptoms may be wrongly attributed to mesenchymal hamartoma compressing the lung parenchyma.
Present case was a five-month-old infant with mesenchymal hamartoma of chest wall. He had respiratory symptoms which were explained by hyper reactive airway disease. We were able to manage it conservatively with a follow-up period of one year. The management of MHCW depends on respiratory symptoms. Surgery is preferred for children who are symptomatic secondary to compression by mass. Cameron D et al., in their case series of three patient reported conservative management of 2 patients with one of the patient requiring surgery [7]. Pawel BR et al., in their case report described a partially resected MHCW which had a benign course on further follow up [8]. Freeburn et al., reported a case of spontaneous regression of infantile MHCW by age of 11 years [9]. Their case also had respiratory symptoms attributed to asthma like in our case MHCW.
Mesenchymal hamartoma are well-circumscribed lesions arising from the central portions of ribs, associated with erosion of adjacent ribs at gross examination [10]. Radiographic appearance of well circumscribed mass with involvement of multiple ribs is diagnostic of MHCW in an infant.
CT scan helps to delineate site of origin, tumour density, effect on lung parenchyma and adjacent structures [11]. CT best demonstrates matrix mineralization, whereas MRI best demonstrates haemorrhagic cystic lesion [6].
Definitive diagnosis is by histopathology examination [4]. Microscopically, the lesion is composed of cartilage, bone and spindle proliferation. Cystic spaces suggest diagnosis of an aneurysmal bone cyst. Spindle cells are arranged in loose fashion. Cartilage is in form of plates maturing into trabecular bone, simulating the appearance of epiphyseal plates.
Other differentials for such mass lesions of chest are fibrous dysplasia and haemangiomas arising from ribs. Langerhans cell histiocytosis, Ewing sarcoma or PNET with large soft tissue mass and involvement of ribs (destruction, sclerosis) is a close differential. But these can be differentiated on basis of rib origin, presence of secondary aneurysmal bone cyst component with characteristic radiological finding. Because of morbidity associated with surgery, conservative management can be tried with surgical resection in symptomatic patient at presentation or follow up [7]. Management is guided by clinical presentation with surgery being curative. Surgery is indicated if compression by the mass causes pulmonary or cardiac compromise. Conservative management by close follow up and periodic imaging is advocated as spontaneous regression can occur and large residual chest wall defect after en bloc resection can frequently result in a scoliosis. Surgery may also be complicated by large amount of blood loss due to haemorrhagic elements. Recent reports continue to support attempted total resection. Long term data on conservative management outcomes are lacking.
Conclusion
MHCW with its clinical presentation and radiological features may be alarming and may lead to suspicion of malignant lesion unless clinician is aware of this entity. With better understanding of natural history of this benign condition, a trend towards conservative management especially in asymptomatic cases is likely. There is need for data on long term follow up on cases managed conservatively. Malignant transformation in primary mass or after resection is rare.
[1]. Eskelinen M, Veli-Matti K, Vainio J, Mesenchymoma of the chest wall in childrenAnn Thorac Surg 1991 52:291-93. [Google Scholar]
[2]. Balci P, Obuz F, Gore O, Aneurysmal bone cyst secondary to infantile cartilaginous Hamartoma of ribPaediatr Radiol 1997 27:767-69. [Google Scholar]
[3]. Kim JY, Jung WH, Yoon CS, Mesenchymal Hamartoma of the chest wall in infancy: radiologic and pathologic correlationYonsei Med J 2000 41(5):615-22. [Google Scholar]
[4]. Brar MK, Cubberley DA, Baty BJ, Branch DW, Chest wall Hamartoma in a fetusJ Ultrasound Med 1998 7:217-220.PMID 328506 [Google Scholar]
[5]. Rose NC, Coleman BG, Wallace D, Prenatal diagnosis of chest wall Hamartoma and sternal cleftUltrasound Obstet Gynecol 1996 7:453-58. [Google Scholar]
[6]. Groom KR, Murphey MD, Howard LM, Mesenchymal Hamartoma of the chest wall: radiologic manifestations with emphasis on cross-sectional imaging and histopathology comparisonRadiology 2002 222(1):205-11.doi:10.1148/radiol.2221010522 [Google Scholar]
[7]. Cameron D, Ong TH, Borzi P, Conservative management of mesenchymal hamartomas of the chest wallJ Paediatr Surg 2001 36(9):1346-49.PubMed PMID: 11528603 [Google Scholar]
[8]. Pawel BR, Crombleholme TM, Mesenchymal hamartoma of the chest wallPaediatr Surg Int 2006 22(4):398-400.Epub 2005 Dec 6. PubMed PMID: 16331523 [Google Scholar]
[9]. Freeburn AM, McAloon J, Infantile chest hamartoma—case outcome aged 11Arch Dis Child 2001 85:244-25. [Google Scholar]
[10]. McCarthy EF, Dorfman HD, Vascular and cartilaginous Hamartoma of the ribs in infancy with secondary aneurysmal bone cyst formationAm J Surg Pathol 1980 4:247 [Google Scholar]
[11]. Psaila J, Carachi R, Raine PAM, Patrick WJA, Thoracic mesenchymoma of infancyJ Paediatr Surg 1996 31:726-68. [Google Scholar]