Takayasu Arteritis with Bilateral Renal Artery Stenosis and Left Subclavian Artery Stenosis in Pregnancy
Sharma Nalini1, Singh Ahanthem Santa2
1 Assistant Professor, Department of Obstetrics and Gynaecology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India.
2 Professor and Head of Department, Department of Obstetrics and Gynaecology, North Eastern Indira Gandhi Regional Institute of Health and Medical SciencesShillong, Meghalaya, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nalini Sharma, Assistant Professor, Department of Obstetrics and Gynaecology, B 1 D, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences Shillong, Meghalaya-793018, India.
E-mail: Nalinisharma100@rediffmail.com
Takayasu arteritis (TA) is a rare, systemic, chronic inflammatory, progressive, idiopathic disease of aorta and its main branches. It causes narrowing, occlusion and aneurysm of arteries. It affects mainly young females in about 80-90% of cases (young female arteritis). TA has adverse effect on pregnancy in the form of abortion, superimposed preeclampsia, IUGR (Intrauterine growth restriction), IUFD (intrauterine fetal death), abruption and CCF (congestive cardiac failure). Careful assessment, treatment of TA complication, regular antenatal followup and multidisciplinary approach involving obstetrician, cardiologist, rheumatologist and anaesthetist improve maternal and fetal outcome. We described here a case of pregnancy with TA with bilateral renal artery stenosis and left subclavian artery stenosis.
Pulseless disease, young women arteritis, pregnancy outcome
Case Report
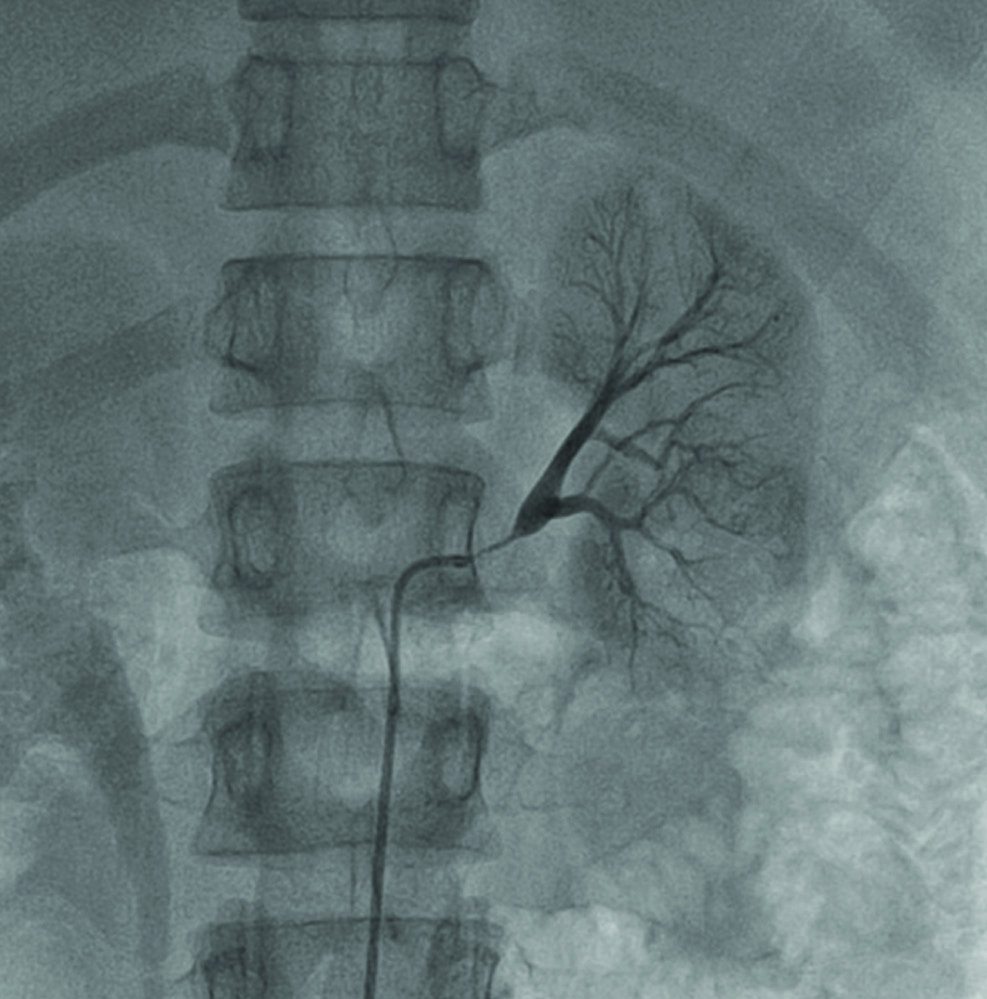
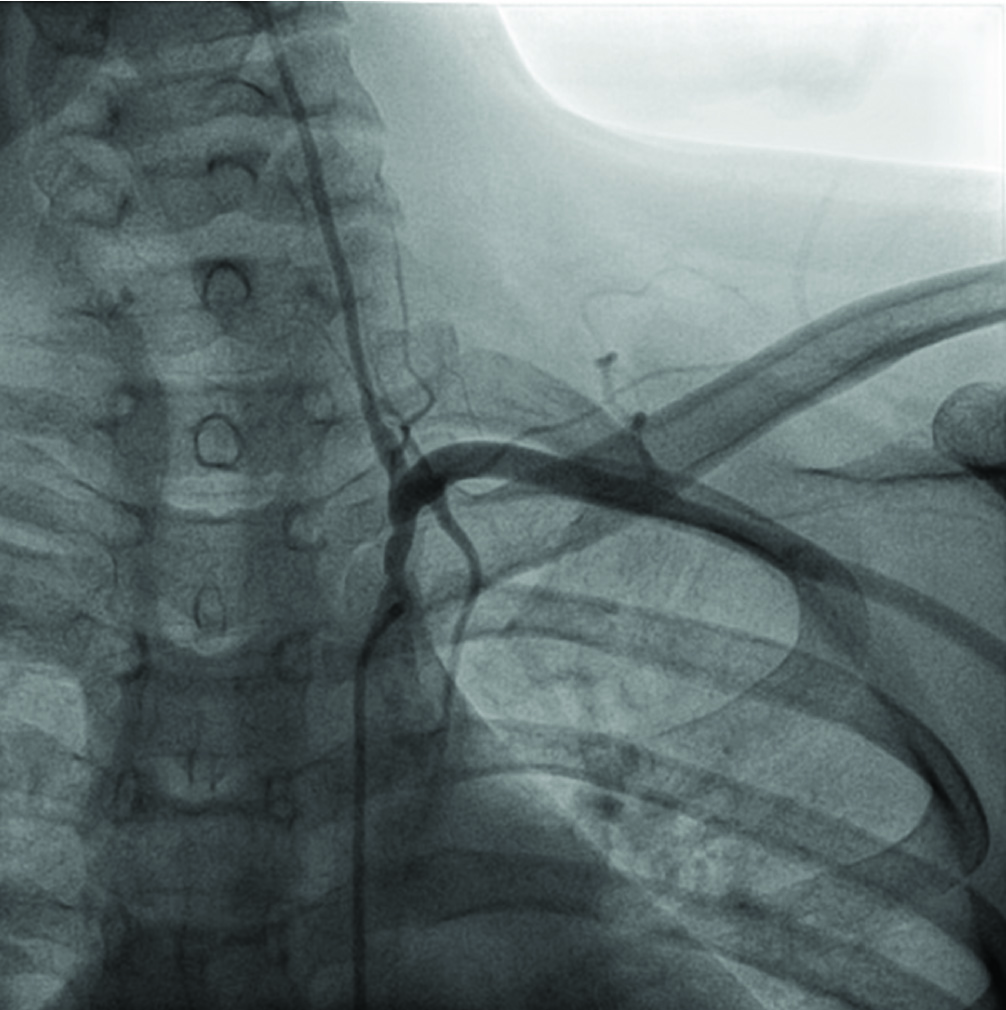
We observed 21-year-old, Mongol origin presented to Gynae OPD at 6 weeks of pregnancy with TA and severe hypertension. One year back when she was evaluated for pain in abdomen she diagnosed as a case of abdominal kochs and hypertension. On further evaluation for hypertension she diagnosed a case of Takayasu arteritis with bilateral renal artery stenosis (90-95%) with left subclavian stenosis (85%) [Table/Fig-1,2]. Left subclavian artery stenting and bilateral percutaneous transluminal angioplasty of renal arteries done [Table/Fig-3,4]. She put on three antihypertensive amlodipine, methyldopa, enalapril and ecospirin, antitubercular drugs. During pregnancy she was in remission, enalapril replaced with labetalol. Her routine investigations including renal function test, fundus and echo were within normal limits. But she was admitted four times for uncontrolled hypertension during antenatal period. To monitor fetal growth monthly obstetric ultrasound and umblical artery Doppler was done. She developed intrauterine growth restriction. There was no superimposed preeclampsia. Strict maternal and fetal surveillance done. Surfactant induction initiated. Elective LSCS done at 37 completed weeks in lieu of IUGR, as well as cardiologist’s recommendation to prevent volume overload and CHF in second stage. Epidural anaesthesia given, 2.4 kg baby delivered with Apgar >9. Patient discharged well on three antihyertensive with advice of regular followup especially with cardiologist.
Anterio-posterior view showing 90% stenosis of left renal artery
Anterio-posterior view showing 80% osteal-proximal stenosis of left subclavian artery
Anterio-posterior view showing post angioplasty with stenting of left subclavian artery
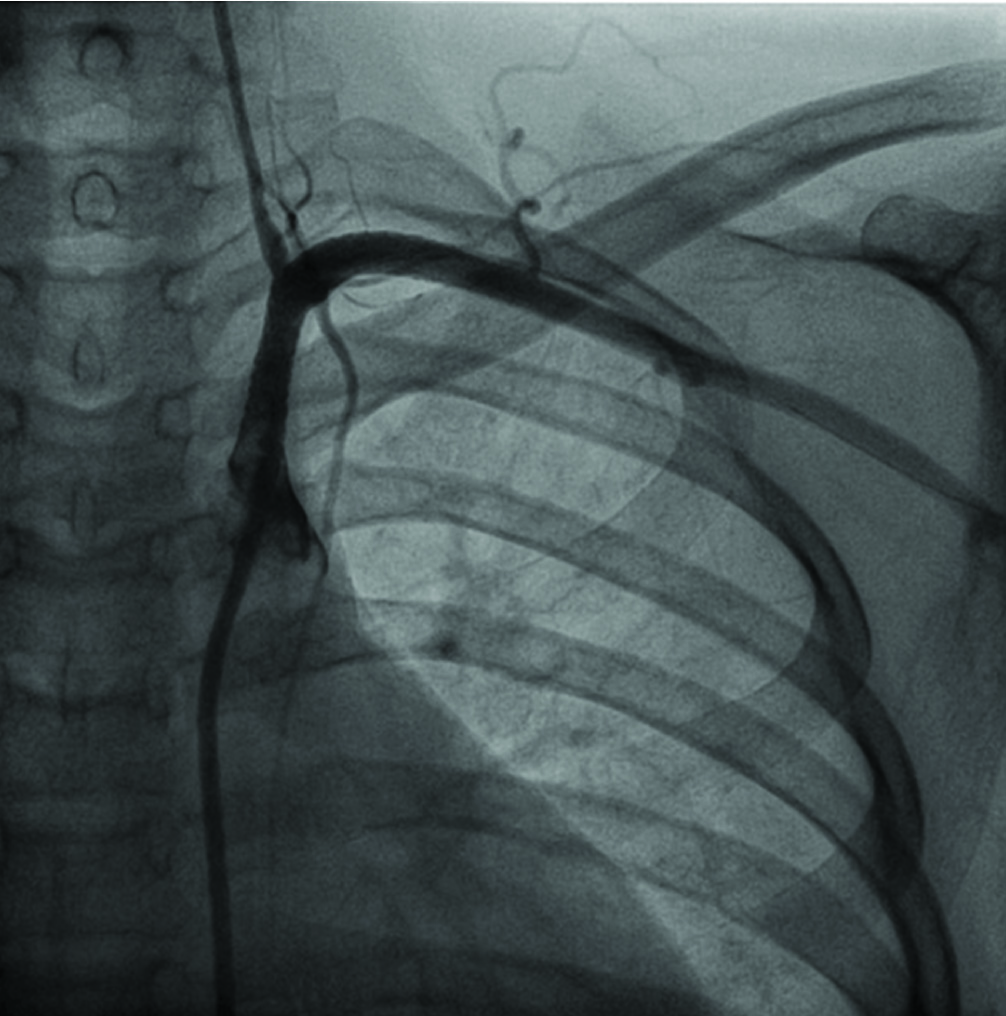
Anterio-posterior view showing stent deployment in both right and left renal artery, flow restored

Discussion
Takayasu arteritis (TA) is a rare, systemic, chronic inflammatory, progressive, idiopathic disease of aorta and its main branches affects mostly carotid, subclavian, pulmonary, iliac and renal arteries [1,2]. It causes narrowing, occlusion and aneurysm of arteries. It affects mainly young females in about 80-90% of cases (young female arteritis). It is common in Asia and oriental countries. World wide annual incidence of disease is 1.2-2.6 cases/million [2]. Clinical presentation is highly varied and depends on affected artery, from limb claudication, numbness, vertigo, visual changes, angina, and seizures. The distinguishing clinical sign are diminished or absent pulse (80-90%), differences in blood pressure, carotid, subclavian or aortic bruit (80-95%), retinopathy and hypertension [2]. It is also known as “pulseless disease” because pulse may not palpable at times due to occlusion of artery. Blood pressure may not be recordable in upper limb or disparity of blood pressure [2]. In this patient BP discrepancy was 20 mm of Hg, more in right arm. Few patients may lead to aortic insufficiency, congestive cardiac failure, hypertensive encephalopathy and stroke. Diagnosis is based on symptoms, signs, inflammatory marker and angiography of aorta and its branches. Treatment includes corticosteroids, anti-inflammatory and immunosuppression like azathioprine and methotrexate if corticosteroids fails.
Available data suggests that disease does not worsen or improve with pregnancy [1]. But TA has adverse effect on pregnancy in the form of abortion, superimposed preeclampsia, IUGR, IUFD, abruption and CCF [3–5]. Aetiology of TA is still unknown. It may be autoimmune or genetic in origin or infective particularly Mycobacterium tuberculosis because tuberculosis is endemic in areas with high prevalence of TA [6]. This patient had history of abdominal kochs. Disease progression typically occurs in various stages from acute inflammatory arteritis to lymphocytic infiltration, intimal thickening, elastic tissue destruction, fibrosis and patchy luminal narrowing of arteries. Depends on presence or absence of four major complications such as hypertension, retinopathy, aneurysm and aortic insufficiency, it can be classified into four stages [7]. In stage 1, None of these complications were present. Stage 2a, patients had only one of these complication. Stage 2b, patients had one of these complications but in the severe form. Stage 3, when more than one complication was present. The patient presented here was in Stage 2b. She had uncontrolled hypertension. Cause of hypertension might be renal ischemia due to narrowing of renal arteries. She had bilateral renal arteries stenosis (90-95%). Hypertension may be due to decreased elasticity and narrowing of aorta and its branches and abnormal function of carotid and aortic sinus baroreceptor [8,9]. Patient of TA with bilateral renal arteries stenosis usually have difficulty in controlling blood pressure just like in this patient. Although this patient did not develop superimposed preeclampsia. Pregnancy with TA complicated by IUGR [4,5]. Aetiology of IUGR may be impaired placental blood flow. Incidence of IUGR is high when bilateral renal involvement is present [1]. These patients should have regular maternal and fetal surveillance. Monthly obstetrics USG and umblical artery Doppler is must to monitor fetal growth and early diagnosis of IUGR. Pregnancy with TA is a high risk pregnancy. Patient advised to conceive after controlling of blood pressure as normal BP at the beginning of prenatal care associated with better outcome [10]. Vaginal delivery could be indicated in group I and IIa. Epidural anaesthesia has been used to provide stable haemodynamics and pain relief during labour and delivery. Second stage of labour to be cut short by instrumental delivery. For LSCS also, choice of anaesthesia is be epidural anaesthesia because regional anaesthesia is associated with sympathetic blockade and subsequent drop in BP specially harmful in a patient with compromised regional circulation due to stenosed arteries [1]. Epidural anaesthesia is associated with gradual onset of sympathetic block and decrease in BP. Epidural block ensures complete pain relief which helps in smooth control of BP in the intraoperative and postoperative period. In this case pregnancy outcome was good, same finding was also described by Hauenstein in which 83.9% newborns were healthy [4]. After delivery, maternal peripheral vascular resistance increases, it may lead to pulmonary oedema, cardiac decompensation and stroke mainly first two day after delivery, therefore these patient require special care in puerperium.
Conclusion
TA is an inexplicable inflammatory arteritis with potential involvement of multiple large arteries and varied disease presentation. If a young women present with hypertension, TA should consider in differential diagnosis. Careful assessment, treatment of TA complication, regular antenatal followup and multidisciplinary approach involving obstetrician, cardiologist, rheumatologist and anaesthetist improve maternal and fetal outcome.
[1]. Ishiwaka K, Matsumura S, Occlusive thrombopathy (Takayasu’s disease) and pregnancy. clinical course and management of 33 pregnancies and deliveriesAm J Cardiol 1982 50(6):1293-300. [Google Scholar]
[2]. Langford Carol A, Fauci Anthony S, Harrisons Principle of internal medicine 2008 17th ednNew YorkMcGraw-Hill Medical [Google Scholar]
[3]. Cunningham FG, William JW, Williams Obstetrics 2009 23rd ednNew YorkMcGraw-Hill Medical [Google Scholar]
[4]. Hauenstein E, Frank H, Bauer JS, Takayasu arteritis in pregnancy: review of literature and discussionJ Perinat Med 2009 38(1):55-62. [Google Scholar]
[5]. Mandal D, Mandal S, Dattary C, Takayasu arteritis in pregnancy: an analysis from eastern IndiaArch Gynecol Obstet 2011 285(3):567-71. [Google Scholar]
[6]. Subramanyan R, Joy J, Balakrishnan KG, Natural history of aortoarteritis (Takayasu’s disease)Circulation 1989 80:429-37. [Google Scholar]
[7]. Ishiwaka K, Natural history and classification of occlusive thrombopathy (Takayasu’s disease)Circulation 1978 57(1):27-35. [Google Scholar]
[8]. Sharma BK, Sagar S, Singh AP, Takayasu arterits in IndiaHeart vessel 1992 7(supp):37-43. [Google Scholar]
[9]. Jain D, Rojha M, Aggarwal M, Kumar D, Indian origin Takayasu’s arteritis: A case report with a brief review of clinical managementAnaesth Pain & Intensive Care 2012 16(2):191-93. [Google Scholar]
[10]. Hidka N, Yamanka Y, Fukushima K, Clinical manifestation of pregnancy in patients with takayasu arteritis: Experience from a single tertiary centerArch Gynecol Obstet 2011 285(2):377-85. [Google Scholar]