An Unusual Presacral Cyst in An Infant
Pragati Aditya Sathe1, Ratnaprabha Kundlikrao Ghodke2, Vageriya Natasha Laxmilal3, Bhuvaneshwari Mahendra Kandalkar4, Parelkar Sandesh Vinod5
1 Associate Professor, Department of Pathology, Seth G. S. Medical College and KEM Hospital, Mumbai, India.
2 Assistant Professor, Department of Pathology, Seth G. S. Medical College and KEM Hospital, Mumbai, India.
3 Assistant Professor, Department of Pediatric Surgery, Seth G. S. Medical College and KEM Hospital, Mumbai, India.
4 Professor, Department of Pathology, Seth G. S. Medical College and KEM Hospital, Mumbai, India.
5 Professor, Department of Pediatric Surgery, Seth G. S. Medical College and KEM Hospital, Mumbai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pragati Aditya Sathe, A/7, Jeevan Sudha Society, C.D. Barfiwala Road, Andheri West, Mumbai 400058, India.
E-mail: pragativk@yahoo.com
The neurenteric cyst is a rare developmental lesion arising as a result of persistence of the neurenteric canal. It usually presents in the second and third decade. Lesions occurring in children are rare. Majority of the cases presented with signs of spinal cord involvement. This is a rare case of neurenteric cyst in an infant who presented with a presacral mass. A nine-month-old female had an antenatally diagnosed sacrococcygeal lesion. Radiology suggested a diagnosis of sacrococcygeal teratoma. Histology was typical of a neurenteric cyst. We report this case to create awareness about this rare cystic lesion and inclusion of this entity in the differential diagnosis of cystic masses in children at this location.
Neurenteric, Sacrococcygeal lesion, Spinal cord
Case Report
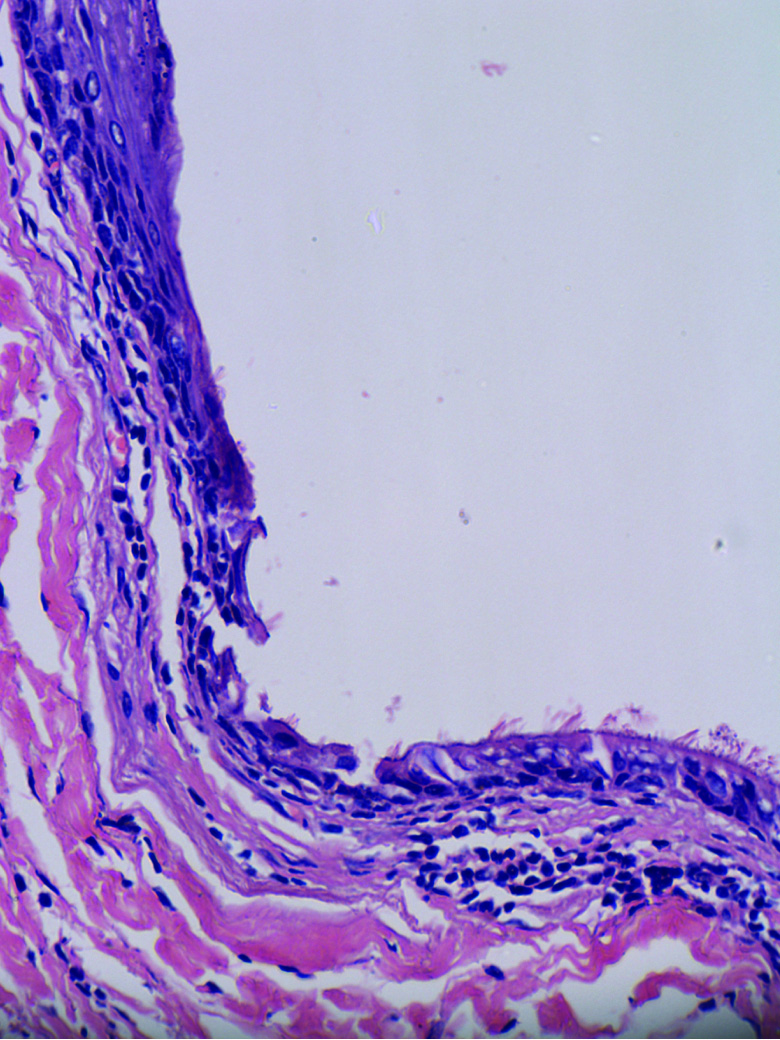
A nine-month-old female child, first by birth order, born of a non-consanguineous marriage, by lower segment caesarean section, had an antenatally diagnosed presacral mass. The patient presented to our hospital for the management of this mass. There was no significant family history. The patient did not have any symptoms of neurological involvement like weakness, radicular pain, sphincter disturbances or paresthesia. Magnetic resonance imaging of the pelvis showed a multicystic presacral mass not communicating with the sacral foramen [Table/Fig-1a]. The radiologic impression was a Type IV sacrococcygeal teratoma. The haematologic parameters, renal function tests and serum levels of alpha fetoprotein were within normal limits. The patient underwent surgical excision of the cyst through open laparotomy along with coccygectomy. Intraoperatively, a cystic swelling measuring 6x5 cm and containing clear fluid was excised from the presacral area. The cyst was sent for histopathologic examination. On gross examination, a unilocular ellipsoidal cyst measuring 6x3x1.5 cm was seen with smooth inner surface and a wall thickness of 0.5 cm. No solid areas were appreciated [Table/Fig-1b]. Histopathologic examination showed the wall of the cyst to be composed of thin fibrocollagenous tissue along with mature neuroglial tissue [Table/Fig-1c,d]. It was lined by pseudostratified columnar ciliated epithelium with foci of squamous metaplasia [Table/Fig-2]. The cyst did not show any other mature or immature structures. A diagnosis of neurenteric cyst was given. The patient was discharged after an uneventful postoperative period. On follow-up, one year later, the patient is doing well without any neurological deficit.
a) MRI pelvis showing the cyst in presacral space
b) Cyst measuring 6x3x1.5 centimeters with smooth inner aspect and without solid areas.
c) The cyst wall focally lined by metaplastic squamous epithelium with mature neuroglial tissue in the wall (H&E x 100)
d) Pseudostratified columnar ciliated mucin containing epithelium lining majority of the cyst wall (H&E x 400)

Pseudostratified columnar epithelium undergoing metaplasia to squamous epithelium thus favouring a diagnosis of neurenteric cyst (H&E x400)
Discussion
Neurenteric cysts were earlier described as teratomatous cysts or intestinomas till Holcomb and Matson coined the term neurenteric cyst in 1954 [1]. According to the review of literature on neurenteric cysts by Santos De Oliveira et al., less than 150 cases have been reported till date in paediatric population (<18-year-old) and about 29 cases have been reported in children less than one-year-old [1–3].
Majority cysts present as solitary lesions located ventrally in intradural extramedullary compartment [2]. Uncommon locations include cranium, skull base, cerebello-pontine angle, cavernous sinus, brainstem and optic nerve [1]. For paediatric population, the mean age at presentation is 6.4 years [1,2].
They result from abnormal separation of the neural tube and the endodermis during the 3rd week of gestation, leading to the persistence of endodermal elements in the spinal canal. Theories put forth for the formation of neurenteric cysts suggest that they could occur due to abnormal endodermal-ectodermal adhesion with subsequent splitting of the notochord. Splitting of the notochord could be the primary event. Persistence of the neurenteric canal or formation of an accessory neurenteric canal, over distension of the neural tube or a teratomatous origin from primordial germ cells are the other theories that have been put forth for its development [3].
The patients can present with myelopathic or radicular symptoms depending on the location of the cyst [1,4]. However, our patient presented with a presacral mass and did not have any neurological complaints.
Various anomalies of gastrointestinal tract, renal defects, cardiac malformations and cutaneous changes have been associated with neurenteric cyst in addition to the commoner bony vertebral abnormalities. Conditions like spinal dysraphism, scoliosis, spina bifida, split cord malformation and Kippel-Fiel syndrome may also be associated with neurenteric cyst [2]. Isolated spinal neurenteric cysts without associated bone or soft tissue malformations are rare just as also observed in our patient [4].
On Magnetic resonance imaging, it can be resemble a teratoma as also seen in our case [5]. Plain radiograph of the vertebral column is always indicated given the high incidence of associated bony anomalies.
As per the histological classification of these cysts described by Wilkins and Odom, three subtypes exist [6]. Type A cysts contain either columnar or cuboidal cells with ciliated and non ciliated component a top a basal membrane. Type B cysts include all features of Type A as well as additional tissue that can include bone, cartilage, lymphatic tissue, fat or glandular components. Type C cysts are identified by Type A features in association with ependymal or glial tissue. There appears to be no correlation of these subtypes with outcome or management [2]. The present patient had a Type C neurenteric cyst.
The differential diagnoses in this location include cystic lesions that show mature neuroglial tissue in the wall namely meningomyelocele, teratoma and a glioependymal cyst. Presence of a well defined epithelial lining differentiates it from a meningomyelocele. Type B neurenteric cysts can closely resemble a teratoma. Again, the continuous presence of an epithelium reminiscent of gastrointestinal or respiratory epithelium lining the cyst and absence of other components favours a diagnosis of neurenteric cyst over a teratoma. A glioependymal cyst has an ependymal lining and absence of goblet cells within the lining epithelium.
Total resection of the cyst instead of simple aspiration is curative. However, recurrence related to incomplete resection has been reported in one third cases [1,2,7].
Conclusion
Awareness of this entity is essential for clinicians, radiologists and pathologists to achieve an accurate diagnosis and differentiate it from the commoner teratoma. This uncommon lesion has to be included in the differential diagnoses of presacral masses in children.
[1]. de Oliveira RS, Cinalli G, Roujeau T, Sainte-Rose C, Pierre-Kahn A, Zerah M, Neurenteric cysts in children:16 consecutive cases and review of the literatureJ Neurosurg 2005 103:512-23. [Google Scholar]
[2]. Savage JJ, Casey JN, McNeill IT, Sherman JH, Neurenteric cysts of the spineJ Craniovertebr Junction Spine 2010 1:58-63. [Google Scholar]
[3]. LeDoux MS, Faye-Petersen OM, Aronin PA, Vaid YN, Pitts RM, Lumbosacral neurenteric cyst in an infant. Case reportJ Neurosurg 1993 78:821-25. [Google Scholar]
[4]. Satyarthee GD, Mahapatra AK, Presacral neurenteric cyst in an infantPaediatr Neurosurg 2003 39:222-24. [Google Scholar]
[5]. Muzumdar D, Bhatt Y, Sheth J, Intramedullary cervical neurenteric cyst mimicking an abscessPaediatr Neurosurg 2008 44:55-61. [Google Scholar]
[6]. Wilkins RH, Odom GL, Spinal Intradural Cysts. In: Vinkin PJ, Bruyn GW, editorsTumors of the spine and spinal cord, Part II. Handbook of Clinical Neurology 1976 Vol. 20North HollandAmsterdam:55-102. [Google Scholar]
[7]. Kapoor K, Jajoo M, Dabas V, Manchanda V, Neurenteric cyst in a neonate:a rare congenital thoracic cystJ Neonatol 2011 25:109-110. [Google Scholar]