Vertical root fractures in teeth present with challenges not only with diagnosis but also with management. The prognosis in such teeth is generally questionable with extraction of the tooth being the most common treatment option. However, conservative treatment options such as reconstruction of the fractured fragments with adhesive resin followed by intentional replantation have been recently suggested. There are only a few case reports that describe management of complete vertical root fracture by reconstruction of fragments. The present case report describes successful management of an unusual complete vertical root fracture of a maxillary right central incisor in a 23-year-old male by reconstructing the fragments with a dual cure resin followed by intentional replantation. At the three year follow up, the tooth was asymptomatic, radiographically sound with probing depth and mobility within normal physiological limits.
Adhesive resin, Reattachment, Splinting, Root Fracture
Case Report
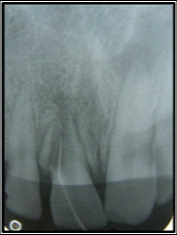
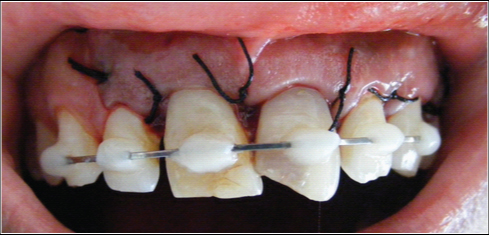
A 23-year-old male was referred to the Department of Conservative Dentistry and Endodontics complaining of occasional pain on biting since one year in his upper right front tooth. He gave a history of fall from a bicycle two years back where he fractured his maxillary central incisors but did not undergo any treatment for the same. His medical history and extraoral examination were non contributory. Intraoral examination revealed enamel and dentin fracture involving the incisal edge in tooth 11, 21 along with discoloration of crown in both the teeth. Soft tissue examination showed the presence of sinus tract in the attached gingiva in relation to tooth 11 [Table/Fig-1]. Periodontal probing revealed deep narrow isolated pockets on both facial and palatal aspect of tooth 11 while other teeth showed a probing depth of non-pathologic value of 2-3 mm. Pulp sensibility tests showed negative response in teeth 11, 21, 22. Radiographic evaluation was done by digital intraoral periapical (IOPA) radiograph [Table/Fig-2], which clearly revealed a complete vertical root fracture in tooth 11. There was wide separation of fragments with the fragment lying in contact with tooth 12. Guttapercha point was inserted into the sinus tract and another digital IOPA radiograph [Table/Fig-3] was taken which showed the guttapercha point tracing along the fracture line that extended from below the alveolar crest till the root apex. A periapical radiolucency of approximately 1 cm in diameter was seen in relation to tooth 21, 22. However, no fracture lines were observed in these teeth.
Preoperative Intraoral view showing sinus tract,

Preoperative IOPA radiograph,

IOPA radiograph with guttapercha tracing the sinus tract,
Patient was explained about the treatment plan for the involved teeth which included root canal treatment in teeth 21, 22 and extraction of tooth 11 followed by replacement with implant or a fixed or removable prosthesis. However, patient was not convinced for extraction of tooth 11 and wanted to save the tooth. Hence, it was decided to reconstruct the fractured fragments following surgical extraction of tooth 11 followed by immediate intentional replantation while non surgical endodontic therapy was planned for tooth 21, 22. The limitations of the procedure were explained to the patient and a written consent was obtained.
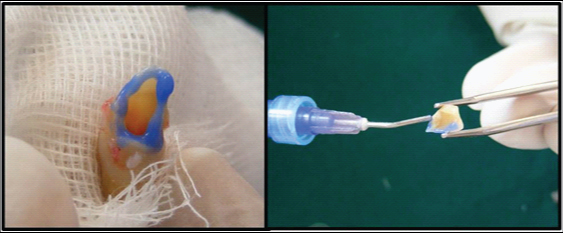
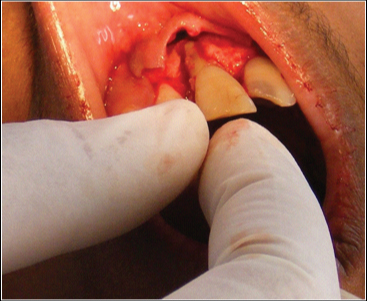
Lignocaine with 1:100000 epinephrine was administered as buccal infiltration and nasopalatine nerve block. A full thickness mucoperiosteal flap was elevated on the labial aspect extending from distal side of maxillary left canine to the distal aspect of maxillary right lateral incisor [Table/Fig-4]. Tooth 11 was extracted as atraumatically as possible and the two fractured fragments were also recovered [Table/Fig-5]. Granulation tissue was carefully removed from the tooth and the fragments while holding the tooth in gauze moistened with isotonic saline and propolis solution (Dentosafe, MedicePharma, Iserlohn, Germany).
Full thickness mucoperiosteal flap elevation

Tooth and root fragments extracted

The alveolar socket was also carefully curetted to remove any granulation tissue and irrigated with isotonic saline [Table/Fig-6]. The extracted tooth was inspected and confirmed of no extra fracture. The fractured fragments and the tooth were etched at the fracture margins [Table/Fig-7] with 37% phosphoric acid (Ultra-etch, Ultradent, South Jordan) for 15 seconds, and then washed and air dried. Bonding agent (Adper Single Bond Plus, 3M ESPE, St. Paul, MN, USA) was brushed over the etched fragments and light cured for 20 seconds followed by reattachment of a fragment with a dual cure resin cement (RelyX ARC 3M ESPE, St. Paul, MN, USA). The resin cement was light cured for 20 seconds.
Freshly extracted socket,

Etching of tooth and fragment margins
Retrograde obturation of the root canal was done extraorally [Table/Fig-8] using flowable composite resin (Tetric N Flow, Ivoclar Vivadent, Liechtenstein) reinforced with glass fibre (Ribbond, Inc., Seattle, Washington USA). Following this, the smallest fragment was also reattached, thereby completely reconstructing the whole tooth [Table/Fig-9,10].
Retrograde obturation using flowable composite resin reinforced with glass fibers
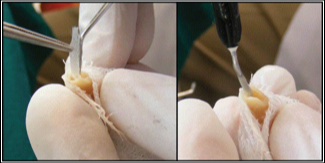
Tooth reconstructed (palatal view),

Tooth reconstructed (labial view)

The root surfaces were treated with tetracycline solution for 30 seconds and then replanted in the alveolar socket in its original position [Table/Fig-11]. Semi-rigid splinting was done using a 21-gauge stainless steel orthodontic wire for 10 days [Table/Fig-12] and a postoperative IOPA radiograph was taken [Table/Fig-13]. The complete procedure took 20 minutes of extraoral time.
Tooth reimplanted in socket
Postoperative intraoral view after splinting,
Immediate postoperative IOPA radiograph

Postoperative instructions were given which included soft diet for one week and careful brushing after every meal. Doxycycline 100mg BID was prescribed for seven days.
The splint was removed after 10 days. There were no signs of periapical infection and the gingiva had healed. Aesthetic management of tooth 11, 21 were denied by the patient. A regular six monthly follow up was done. After three years, there was successful healing of tooth 11 with probing depth and mobility within normal physiological limits. No radiographic signs of resorption were observed [Table/Fig-14].
Follow up IOPA radiograph after three years

Discussion
Vertical root fractures are most commonly associated with endodontically treated teeth; their presence in a non treated tooth is a rare presentation [1,2]. There is no single clinical feature that indicates its presence; hence diagnosis of vertical root fractures requires more of a predictive than a definitive identification. A cumulative assessment of clinical signs and symptoms and the radiographic features may help reach a definitive diagnosis. The prognosis of the root with vertical root fractures is poor and hence, extraction of the tooth followed by implant placement has been the most suggested treatment option. The recent literature provides cases where successful attempts have been made to conservatively manage incomplete and complete vertical root fractures using MTA, CEM, and reconstruction with adhesive resin followed by intentional replantation [3–6].
In the present case, extraction of tooth 11 and replacement by implant, bridge or denture was discussed with the patient. However, patient was reluctant for extraction and could not afford implant cost, hence an alternative treatment plan was established which included reconstruction of fragments with a dual cure resin cement and immediate replantation. The use of adhesive resin and intentional replantation has been reported in literature for complete and incomplete vertical root fractures. Hayashi et al., Arikan et al., reported successful treatment in vertically fractured incisors with this method [7,8], however failure was observed when the same method was used to treat vertically fractured posterior teeth. The possible reasons could be less occlusal forces and better maintenance of gingival health in anterior teeth. Similar cases have been reported in the literature for management of vertical root fractures which have been summarized in a table [Table/Fig-15].
List of case studies that reported successful management of vertical root fractures
| Authors | Tooth number | Treatment given | Recall period and observation | Evaluation |
|---|
| Ozturk M and Unal GC [3] | 11 | Reconstructed with a self-etching dual-cured adhesive resin cement and intentionally replanted in conjunction with a bio-absorbable barrier membrane. | 4 years | The tooth was asymptomatic, and attachment gain and bone regeneration were observed, no ankylosis was detected clinically or radiographically. |
| Moradi Majd N et al., [4] | 21 | Tooth was extracted, fracture line was shallow prepared and treated with adhesive resin cement, a retrograde cavity was produced and filled with calcium-enriched mixture (CEM) cement, and tooth was replanted. | 12 months | The tooth was asymptomatic. The size of periapical radiolucency was noticeably reduced and there was no clinical sign of ankylosis |
| Unver S et al., [5] | 14 | Fracture was repaired with 4-META/MMA-TBB resin cement and intentional replantation was done | 3 years | Tooth was asymptomatic, radiographically sound, reduced periodontal pockets and vertical bone loss |
| Hadrossek PH and Dammaschke T [6] | 11 | Silicon key prior to intentional extraction, fracture line on extracted tooth prepared and filled with Biodentine followed by replantation using silicon key for correct reposition | 2 years | No pathological findings |
| Hayashi M et al., [7] | 20 teeth with vertical root fracture | Teeth were extracted intentionally and reconstructed with 4-META/MMA-TBB dentin-bonded resin and were replanted into the original sockets. | 4 months to 45 months | The replanted teeth were evaluated by clinical criteria and radiographic examination. The longevity was calculated as 83.3% at 12 months and 36.3% at 24 months. |
| Arikan F et al., [8] | 11 | Fracture was repaired with dual-cure resin cement and intentional replantation was done | 18 months | Clinically and radiographically successful healing |
| Dogan MC et al., [9] | 21 | Tooth was extracted and fragment reattached with dual cure resin cement, the pulp chamber was also filled with the cement followed by intentional replantation | 3 years | No evidence of periapical infection, no signs of root resorption and gingival pocket development |
Ozturk and Unal managed a case of vertical root fracture of a maxillary right central incisor where the fractured tooth was reconstructed with self-etching dual-cured adhesive resin cement and was intentionally replanted in conjunction with a bio-absorbable barrier membrane [3]. A four year follow up was reported which revealed a radiographically and clinically healing outcome. In another recent case by Dogan et al., successful outcome was reported at a three year follow up when a fractured fragment was reconstructed using dual resin cement and replanted [9].
The present case presented with complete vertical root fracture extending from the apex to the coronal part. The presence of sinus tract in attached gingiva rather than in apical region and the presence of deep narrow isolated periodontal pockets both facially and palatally helped us predict a vertical root fracture which was confirmed radiographically that showed wide separation of fragments with the fragment lying next to tooth 12. A full thickness mucoperiosteal flap was raised rather than a more conservative flap to enable us to determine the extent of fracture since radiograph confirmed the separation of fragments. An atraumatic extraction was done and a dual cure resin was used so that extraoral working time could be reduced. Various studies have stated that to preserve the vitality of periodontal ligament and to increase the long term replantation success, extraoral time should be reduced [10,11]. In the present case, the extraoral time was 20 minutes. Moreover, careful handling of fragments during the bonding procedure was ensured by holding them carefully in gauze moistened with isotonic saline and propolis solution which also prevented their dehydration [12]. Propolis solution in lower concentrations has been shown to reduce apoptosis of the periodontium cells and increase their metabolic activity and proliferation [13].
Retrograde obturation was done using fiber reinforced composite not only to reinforce the fragments [14] with the tooth but also to avoid wedging forces that arise due to lateral and vertical compaction during conventional obturation with gutta percha and sealer [15]. Fibers are silanized electrical glass fibers and are impregnated with polymer by the manufacturer. It has a cross-link leno weave which reinforces multi-directionally, transferring forces throughout the fiber network without transferring stress back into the resin. Moreover, it is a biocompatible, translucent material which is highly bondable to composite resin. As there is chemical fusion of the internal walls of the preparation to the materials placed within its confines, “cross-root” reinforcement occurs. This enables enhancement in root strength with a conservative approach.
The root surface was modified with a 30 second application of tetracycline solution before replantation to prevent ankylosis. Various other solutions have been stated in the literature such as citric acid, EDTA, Hanks balanced salt solution that prevent ankylosis after replantation by making the root surface more conducive to cellular adhesion and growth [16]. The tooth was repositioned in a pressure less manner and a semi-rigid splint was used for stabilization to allow for physiological movement of tooth.
A regular six monthly follow up was done which showed reduction in pocket depth and the patient was completely asymptomatic. The percussion tone was also same as that of adjacent and opposing healthy tooth that excluded the presence of ankylosis. The most common complication of a replanted tooth is ankylosis [17,18] and is usually diagnosed within the first two years after replantation [19]. In the present case, a three year follow up revealed successful healing of tooth 11 with probing depth and mobility within normal physiological limits without any signs of ankylosis. But, in rare cases, ankylosis can be observed between 5 to 10 years after replantation [19]. Hence, a further long term follow up is necessary to evaluate the definitive prognosis of such treatment technique for vertical root fractures.
Conclusion
The prognosis of teeth with complete vertical root fracture is usually questionable with extraction being the most common treatment option. However, conservative treatment options such as reconstruction of the fractured fragments with adhesive resin followed by intentional replantation should be considered as described in the present case.
[1]. Yang SF, Rivera EM, Walton RE, Vertical root fracture in non endodontically treated teethJ Endod 1995 21(6):337-39. [Google Scholar]
[2]. Chan CP, Tseng SC, Lin CP, Huang CC, Tsai TP, Chen CC, Vertical root fracture in nonendodontically treated teeth – a clinical report of 64 cases in Chinese patientsJ Endod 1998 24(10):678-81. [Google Scholar]
[3]. Ozturk M, Unal GC, A successful treatment of vertical root fracture: a case report and 4-year follow-upDent Traumatol 2008 24(5):e56-60. [Google Scholar]
[4]. Moradi Majd N, Akhtari F, Araghi S, Homayouni H, Treatment of a vertical root fracture using dual-curing resin cement: a case reportCase Rep Dent 2012 :985215 [Google Scholar]
[5]. Unver S, Onay EO, Ungor M, Intentional re-plantation of a vertically fractured tooth repaired with an adhesive resinInt Endod J 2011 44(11):1069-78. [Google Scholar]
[6]. Hadrossek PH, Dammaschke T, New treatment option for an incomplete vertical root fracture–a preliminary case reportHead Face Med 2014 10:9 [Google Scholar]
[7]. Hayashi M, Kinomoto Y, Miura M, Sato I, Takeshige F, Ebisu S, Short-term evaluation of intentional replantation of vertically fractured roots reconstructed with dentin-bonded resinJ Endod 2002 28(2):120-24. [Google Scholar]
[8]. Arikan F, Franko M, Gurkan A, Replantation of a vertically fractured maxillary central incisor after repair with adhesive resinInt Endod J 2008 41(2):173-79. [Google Scholar]
[9]. Dogan MC, Akgun EO, Yoldas HO, Adhesive tooth fragment reattachment with intentional replantation: 36-month follow-upDental Traumatol 2013 29(3):238-42. [Google Scholar]
[10]. Andersson L, Andreasen JO, Day P, Heithersay G, Trope M, Diangelis AJ, International Association of dental traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teethDent Traumatol 2012 28(2):88-96. [Google Scholar]
[11]. Andreasen JO, Hjorting-Hansen E, Replantation of teeth. II. Histological study of 22 replanted anterior teeth in humansActa Odontol Scand 1966 24(3):287-306. [Google Scholar]
[12]. Parolia A, Thomas MS, Kundabala M, Mohan M, Propolis and its potential uses in oral healthInt J Med Med Sci 2010 2(7):210-15. [Google Scholar]
[13]. Wieckiewicz W, Miernik M, Wieckiewicz M, Morawiec T, Does propolis help to maintain oral health?Evid Based Complement Alternat Med 2013 :351062 [Google Scholar]
[14]. Ayna B, Celenk S, Atakul F, Uysal E, Three-year clinical evaluation of endodontically treated anterior teeth restored with a polyethylene fibre-reinforced compositeAust Dent J 2009 54(2):136-40. [Google Scholar]
[15]. Sedgley CM, Messer HH, Are endodontically treated teeth more brittle?J Endod 1992 18(7):332-35. [Google Scholar]
[16]. Zaman KU, Sugaya T, Hongo O, Kato H, A study of attached and oriented human periodontal ligament cells to periodontally diseased cementum and dentin after demineralizing with neutral and low pH etching solutionJ Periodontol 2000 71(7):1094-99. [Google Scholar]
[17]. Hammarstrom L, Blomlof L, Lindskog S, Dynamics of dentoalveolar ankylosis and associated root resorptionEndod Dent Traumatol 1989 5(4):163-75. [Google Scholar]
[18]. Andreasen JO, Analysis of pathogenesis and topography of replacement root resorption (ankylosis) after replantation of mature permanent incisors in monkeysSwed Dent J 1980 4(6):231-40. [Google Scholar]
[19]. Andreasen JO, Borum MK, Jacobsen HL, Andreasen FM, Replantation of 400 avulsed permanent incisors. 4. Factors related to periodontal ligament healingEndod Dent Traumatol 1995 11(2):76-89. [Google Scholar]