Perigraft Seroma Presenting as Discharging Sinus and Spontaneous Exteriorization of Vascular Graft – A Rare Entity Following Vascular Repair with PTFE Graft
Annu Babu1, Manish Kumar Pandey2, Amit Gupta3, Piyush Ranjan4, Maneesh Singhal5
1 Senior Resident, Department of Surgical Disciplines, AIIMS, New Delhi, India.
2 Senior Specialist Surgeon, Department of Surgery, CCL Hospital, Gandhinagar, Ranchi, Jharkhand, India.
3 Associate Professor, Department of Surgical Disciplines, AIIMS, New Delhi, India.
4 Assistant Professor, Department of Surgical Disciplines, AIIMS, New Delhi, India.
5 Associate Professor, Department of Surgical Disciplines, Aiims, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Maneesh Singhal, Room no. 304, JPN Apex Trauma Center, AIIMS, New Delhi-110029, India. E-mail : drmaneesh@gmail.com
Perigraft seroma presenting as discharging sinus and spontaneous exteriorization of vascular graft are rare complication of vascular injury repair with polytetrafluoroethylene (PTFE) grafts. We hereby report a case of young boy who presented with discharging sinuses and vascular graft coming out from one of the sinuses following vascular repair of femoral artery with PTFE graft after a follow-up of six months but the limb was salvaged. On evaluation PTFE graft was found to be thrombosed and collaterals were formed for distal perfusion. Because of persistent discharging sinuses, PTFE graft was removed and femoral artery was ligated proximal and distal to the graft. This case highlights an unusual complication of PTFE grafts that is commonly used in vascular surgery and also highlights the fact that these graft buy time for gradual collaterals formation for distal perfusion and hence when thrombosed and complicated can be safely removed.
Femoral Artery repair, Spontaneous expulsion, Traumatic vascular injury, Vascular graft
Case Report
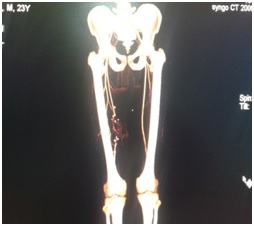
A 23-year-old male presented to Emergency Department of JPN Apex Trauma Centre, AIIMS, New Delhi, India, with history of gunshot injury to his right thigh. He presented within six hours after the injury. Patient was evaluated as per the Advanced Trauma Life Support (ATLS) protocol. He had an entry wound of size 2cm X 2cm on lateral aspect of right mid thigh and 5cmx 4cm exit wound on medial aspect of right mid right thigh. The distal pulsations in right lower limb were absent. He had no other injury. Patient was taken for urgent exploration in operating room. On exploration there was loss of 6 cm of femoral artery segment in mid right thigh region with surrounding devitalized muscle and other tissue. There was no nerve and bony injury. Thorough debridement of wound was done. The injured 6 cm segment of right femoral artery was excised out and repair was done using contralateral reverse saphenous vein interposition graft. Postoperatively distal pulsation was present in injured limb. Patient was heparanized intraoperatively and put on heparin infusion postoperatively. Two days later distal pulsation was absent in right lower limb and it was not showing oxygen saturation. Doppler study of limb showed thrombosed saphenous vein graft. Patient was taken to operating room for re-exploration. Thrombosed venous graft was removed and polytetraflouroethylene (PTFE) graft was used in place for repair. Heparin infusion continued for five days postoperatively. Warfarin 4 mg once daily started with three days overlapping with Heparin. Patient was discharged subsequently after successful re-vascularization and appropriate wound cover. Warfarin continued for three months postoperatively. INR was kept between 2 and 3. He was readmitted six months later with multiple discharging sinuses on right thigh. Small amount of serous fluid was coming out of those sinuses continuously causing a lot of discomfort to the patient. Small portion of graft was also seen coming out through one of the sinuses/spontaneous exteriorization [Table/Fig-1]. Arterial Doppler showed thrombotic occlusion of the PTFE graft. CT sinogram and CT angiography was done. CT angiography showed the thrombosis of graft with distal reformation of superficial femoral artery [Table/Fig-2]. Sinogram showed perigraft collection. There was no symptoms of claudication, rest pain, paraesthesia. Patient was taken up for exploration. Removal of PTFE graft done with proximal and distal ligation of femoral artery. Wound was covered by a split thickness skin graft. Two years follow up did not show any discharge or features of distal ischaemia. Patient is being followed up for development of claudication.
Spontaneous exteriorization of PTFE graft with discharging sinuses

CT angiography showing the thrombosis of graft with distal reformation of SFA
Discussion
Vascular trauma to extremity vessels is common now days because of increase in gunshot injuries, assaults and road traffic injuries. In a study done at a Medical centre in North India blunt trauma accounted for 84% of the vascular injuries with extremities involved in 88% [1]. The brachial artery followed by femoral artery is commonly involved. Repair without graft interposition was done in 74% and autogenous vein grafts were used in 23% of cases. Six percent of patient in which initial repair done by surgery later ended in amputation due to inadequate functional recovery [1]. On clinical examination hard signs of vascular injury are the following: observed pulsatile bleeding, arterial thrill by manual palpation, bruit over or near the artery by auscultation, Sign of distal ischaemia and visible expanding haematoma. Apart from hard signs other signs like Neurological deficit, delayed capillary refill and any bony abnormality should also increase the suspicion of extremity vascular injury and hence need for emergent arteriography or surgical exploration and repair [2]. In most cases of traumatic vascular injury, repair is done by end to end anastomosis. In cases where there is long segment loss of artery, autologous venous graft is preferred choice for repair. PTFE graft is only used when suitable autologous venous graft cannot be used. Currently, for vessels of 5 mm or less in diameter, the use of a saphenous vein graft is the only practical option [3]. Using synthetic graft gives an obvious advantage of completing the vascular repair with better speed. When vascular injury is associated with other injury or there are other complex injury in the same limb, speed of repair is of utmost importance to salvage the limb by doing speedy repair and thereby achieving early distal perfusion. Time is of essence in cases of vascular repair. There are two important technical considerations in using PTFE graft. One is choosing the appropriate size of graft and the other is giving adequate protection to the graft i.e., tissue cover. In young patient and in patient with hypotension the caliber of artery is small. By keeping in mind that the native artery dilates after perfusion, the diameter of the graft taken for interposition should be greater than that of the injured vessel seen intraoperatively. The PTFE graft is made of expanded teflon arranged as nodules connected by thin fibrils. It is an inert material causing minimal surrounding inflammation. Its inner surface has got strong electronegative charge. These features make this graft relatively resistant to thrombosis. It has high early patency rate when compared with saphenous venous graft. Venous graft has later patency rate [4].
Main complication following PTFE graft repair are thrombosis and infection. Twelve-month primary patency for femoral above-knee popliteal artery bypass with PTFE was 95%. Anastomotic intimal hyperplasia is a proliferative non atherosclerotic form of intimal thickening and is a major cause of anastomotic stenosis and bypass graft failure [5–7]. Late graft failure can occur at any time after 30 days. Failures occurring up to 18 months after operation are generally attributed to Neo-intimal hyperplasia involving the graft or one anastomosis, usually the distal one [8,9]. Perigraft seroma presenting as discharging sinus and spontaneous exteriorization of PTFE graft are rare complication. The causes of increased graft permeability are not clear whether this is because of surrounding tissue inflammation or not. It was thought that perigraft serous collection was due to seeping out of the serous component of blood after removal of coiled rings on graft surface. It was later disputed as the serous leak did not coincide with the position of the ring. The use of intraoperative betadine was also thought as a possible cause of increased graft permeability. Seroma around PTFE graft, particularly in extra anatomic site is very bothersome and at times it requires graft removal [10,11]. Any discharging sinus nearby a vascular repair should be taken as some abscess cavity as these grafts are prone for infections. The graft should be looked for patency [12].
Conclusion
Perigraft seroma formation with discharging sinus and spontaneous exteriorization of vascular graft are rare complications of PTFE grafts. All vascular surgeons should be cognizant of this potential complication of PTFE grafts. Postoperatively the patient should be kept under strict follow up to look for these complications.
Consent: Written and informed consent of the patient was obtained for the publication of the case report.
[1]. Menakuru SR, Behera A, Jindal R, Kaman L, Doley R, Venkatesan R, Extremity vascular trauma in civilian population: a seven-year review from North IndiaInjury 2005 36(3):400-06. [Google Scholar]
[2]. H Scott Bjerke, Rowe VL. Extremity vascular trauma treatment and management [internet]. [updated 2013 oct 29; cited 2015 may 18]. Available from http://emedicine.medscape.com/article/462752-treatment [Google Scholar]
[3]. Feliciano DV, Mattox KL, Graham JM, Bitondo CG, Five-year experience with PTFE grafts in vascular woundsJ Trauma 1985 25(1):71-82. [Google Scholar]
[4]. Hobson RW, Lynch TG, Jamil Z, Karanfilian RG, Lee BC, Padberg FT, Results of revascularization and amputation in severe lower extremity ischemia: a five-year clinical experienceJ Vasc Surg 1985 2(1):174-85. [Google Scholar]
[5]. Mills JL, Fujitani RM, Taylor SM, The characteristics and anatomic distribution of lesions that cause reversed vein graft failure: a five-year prospective studyJ Vase Surg 1993 17:195-206. [Google Scholar]
[6]. Garratt KN, Edwards WD, Kaufmann UP, Vlietstra RE, Holmes DR, Differential histopathology of primary atherosclerotic and restenotic lesions in coronary arteries and saphenous vein bypass grafts: analysis of tissue obtained from 73 patients by directional atherectomyJ Am Coll Cardiol 1991 17(2):442-48. [Google Scholar]
[7]. Thatte HS, Khuri SF, The coronary artery bypass conduit: I. Intraoperative endothelial injury and its implication on graft patencyAnn Thorac Surg 2001 72(6):S2245-52. [Google Scholar]
[8]. Reidy MA, Fingerle J, Lindner V, Factors controlling the development of arterial lesions after injuryCirculation 1992 86(6 Suppl):III43-46. [Google Scholar]
[9]. Veith FJ, Gupta SK, Ascer E, Rivers SP, Wengerter KR, Improved strategies for secondary operations on infrainguinal arteriesAnn Vasc Surg 1990 4(1):85-93. [Google Scholar]
[10]. McKay R, Securing of security: the polytetrafluoroethylene leakCardiol Young 1995 5:6 [Google Scholar]
[11]. Eid A, Lyass S, Acute perigraft seroma simulating anastomotic bleeding of a PTFE graft applied as an arteriovenous shunt for hemodialysisAnn Vasc Surg 1996 10(3):290-91. [Google Scholar]
[12]. Thevendran G, Lord R, Sarraf KM, Serous leak, a rare complication of polytetrafluoroethylene grafts: a case reportCases Journal 2009 2:195 [Google Scholar]