Isolated Langerhans Histiocytosis in Thyroid: Thyroidectomy or Chemotherapy?
Anoop Attakkil1, Vandana Thorawade2, Mohan Jagade3, Rajesh Kar4, Kartik Parelkar5
1 Junior Resident, Department of E.N.T & Head and Neck Surgery, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
2 Assistant Professor and Head of The Unit, Department of E.N.T & Head and Neck Surgery, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
3 Professor and Head of The Department, Department of E.N.T & Head and Neck Surgery, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
4 Junior Resident, Department of E.N.T & Head and Neck Surgery, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
5 Junior Resident, Department of E.N.T & Head and Neck Surgery, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anoop Attakkil, Room No 26, First Floor, ST George Hospital Hostel, Near Cst Station, Mumbai-400001, India. E-mail : fasttrack2317@gmail.com
Langerhans cell histiocytosis (LCH) is a rare disorder of mononuclear phagocytic system whose clinical presentation varies from the localised involvement of a single bone to a widely disseminated disease. Langerhans cell histiocytosis rarely involves the thyroid gland and isolated involvement of thyroid is even rarer. We report a case of an eight-year-old male child diagnosed with Langerhans cell histiocytosis limited to thyroid gland with review of literature. Should thyroidectomy be done or proceed with chemotherapy? Our case report raises this question with a note on the role of 18 fluoro deoxy glucose positron emission tomography-computed tomography in the management of the same.
CD1a, 18 FDG PET CT, S-100, Thyroid swelling
Case Report
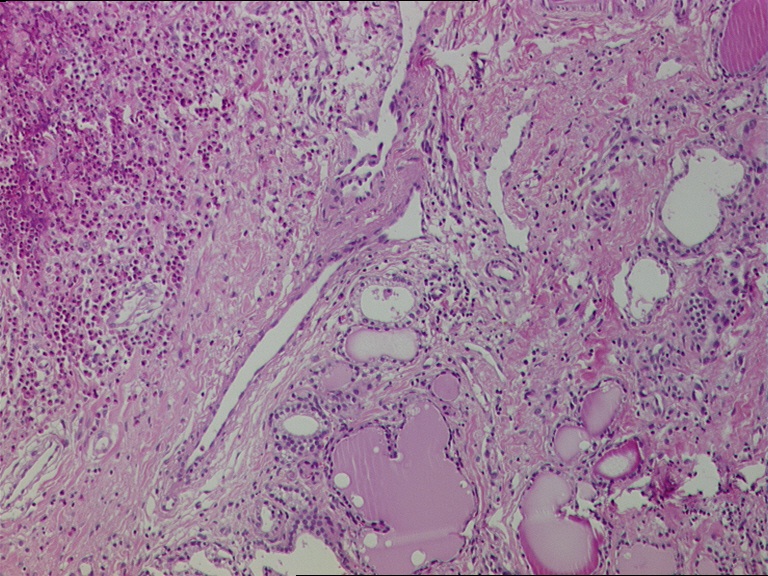
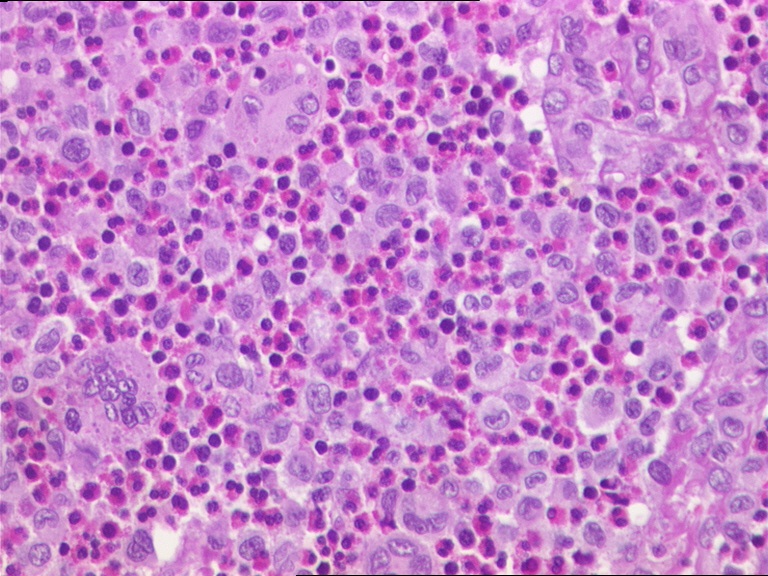
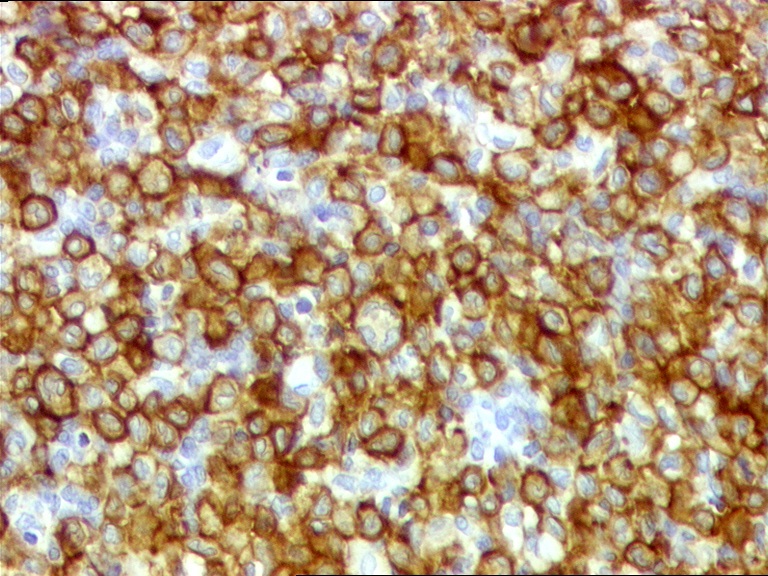
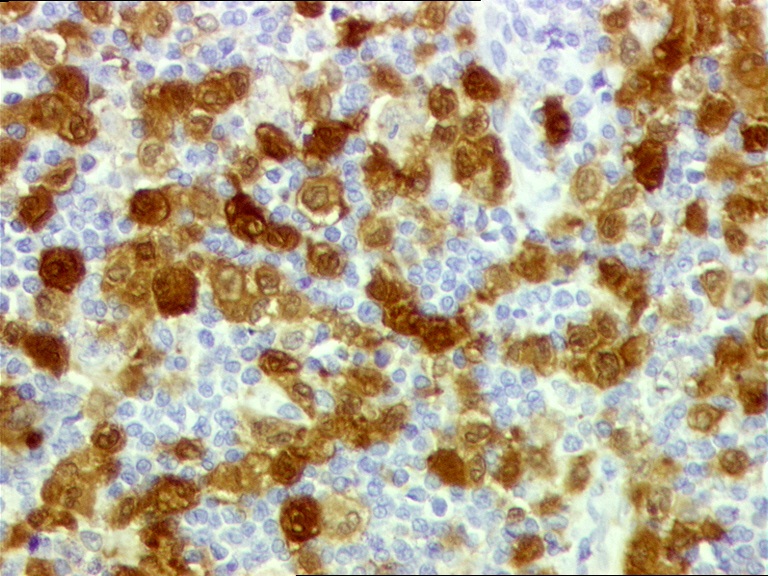
An eight-year-old male child with thyroid swelling of six months duration was referred to the Department of ENT & Head and neck surgery, Grant Govt. Medical College, Mumbai, as papillary carcinoma of thyroid was suspected on fine needle aspiration cytology (FNAC). On clinical examination, an anterior neck swelling of size 3x1cm was present, which was firm, non tender, moving with deglutition. There was no voice change or dysphagia. He had no history suggestive of hypo or hyperthyroidism and thyroid function tests were normal. Ultrasound examination of neck revealed enlarged lobes of thyroid bilaterallly showing multiple well defined hypo echoic lesion within. Few enlarged necrotic cervical lymph nodes were present bilaterally. An expert review of the FNAC slide was done which was inconclusive. Biopsy of thyroid gland was obtained through a horizontal incision over anterior part of the neck from the left lobe of thyroid. Histopathological examination revealed that the thyroid tissue is replaced in most areas by a diffuse infiltrate of mononuclear cells admixed with lymphocyte and eosinophils [Table/Fig-1]. The mononuclear cells showed bean shaped nucleus with nuclear grooves and moderate pale eosinophilic cytoplasm [Table/Fig-2]. Immunohistochemistry showed those cells expressed CD 1a [Table/Fig-3] and S-100 protein [Table/Fig-4] and were immune negative for CD30 and cytokeratin confirmatory for LCH.
Photomicrographs of a a low power image showing the thyroid tissue replaced by a diffuse infiltrate of mononuclear cells admixed with lymphocyte and eosinophills. (H&E staining -100 X)
The mononuclear cells shows bean shaped nucleus with nuclear grooves and moderate pale eosinophilic cytoplasm (H&E staining -400X)
Langerhans cells highlighted by CD1a immunostain, showing cytoplamic staining (-400X)
Langerhans cells highlighted by S-100protein immunostain (-400X)
Patient was further evaluated for systemic involvement for LCH. Clinical examination, biochemical and routine blood tests were normal. Antithyroid antibodies and antimicrosomal antibodies were within normal limits. In bone marrow examination, there was no evidence of myelofibrosis, increased histiocytosis or haemophagocytosis [Table/Fig-5].
The diagnostic evaluation done in the child for systemic evaluation
| S.No | Parametry | Normal |
|---|
| 1 | Total protein | 7.8gm/dl | 5.9-80gm/dL |
| 2 | Albumin | 4.8 gm/dl | 3.7-5.6gm/dL |
| 3 | Total Bilirubin | 0.9 mg/dL | 0.2-1.0 mg/dL |
| 4 | ALT (SGPT) | 17 IU/L | 5-35 IU/L |
| 5 | AST (SGOT | 15 IU/L | 5-40 IU/L |
| 6 | Alkaline phosphatase | 140 IU/L | 115–345 IU/L |
| 7 | INR | 1.12 | 1-1.4 |
| 8 | APTT | 35 s | 42–54 sec |
| 9 | PT | 14s | 11–15 sec |
| 10 | BUN | 12 mg/dl | 7–17 mg/dL |
| 11 | Creatinine | 0.6mg/dL | 0.3-0.9mg/dL |
| 12 | Na+/K+ | 141/ 4.2 mEq/l | Na + 135–148 mEq/L K+ 3.5–58 mEq/L |
| 13 | Erythrocyte Sedimentation Rate (ESR) | 15 mm/hr | 3-20 mm/hr |
| 14 | Ca | 9.2 mg/dL | 9-11 mg/dL |
| 15 | Haemoglobin | 14.4gm/dL | 11.0–133gm/dL |
| 16 | White blood cell | 5400/mm3 | 4500–10500/mm3 |
| 17 | Neutrophils | 65% | 50-70% |
| 18 | Lymphocytes | 28% | 20-40% |
| 19 | Monocytes | 5% | 2-8% |
| 20 | Eosinophils | 2% | 1-4% |
| 21 | Basophils | 0 | 0.5-1% |
| 22 | Platelet count | 3.5x106/mm3 | 1.94–364 X 106/mm3 |
| 23 | Free T3 | 120 ng/dL | 96–232 ng/dL |
| 24 | Free T4 | 1.1 ng/dl | 0.81–168 ng/dL |
| 25 | TSH | 1.8 mIU/L | 0.37–600 mIU/L |
| 26 | TBG | 18 mg/L | 15.0–292 mg/L |
| 27 | Thyroglobulin | 15 ug/L | 3-42 ug/L |
| 28 | Antithyoid Antibodies | <1.3IU/ml | <35 IU/ml |
| 29 | Bone marrow Evaluation | Within normal limits | |
| 30 | Abdominal ultrasound | No significant abnormality | |
| 31 | FNAC Thyroid | Inconclusive | |
| 32 | USG neck | Multiple well defined hypo echoic lesions in both lobes of thyroid gland with a few enlarged necrotic cervical lymph nodes | |
| 33 | Biopsy of Thyroid [Table/Fig-2,3 and 4] | LCH cells with CD 1a, S-100 Positivity | |
| 34 | Skeletal Survey | Within Normal Limits | |
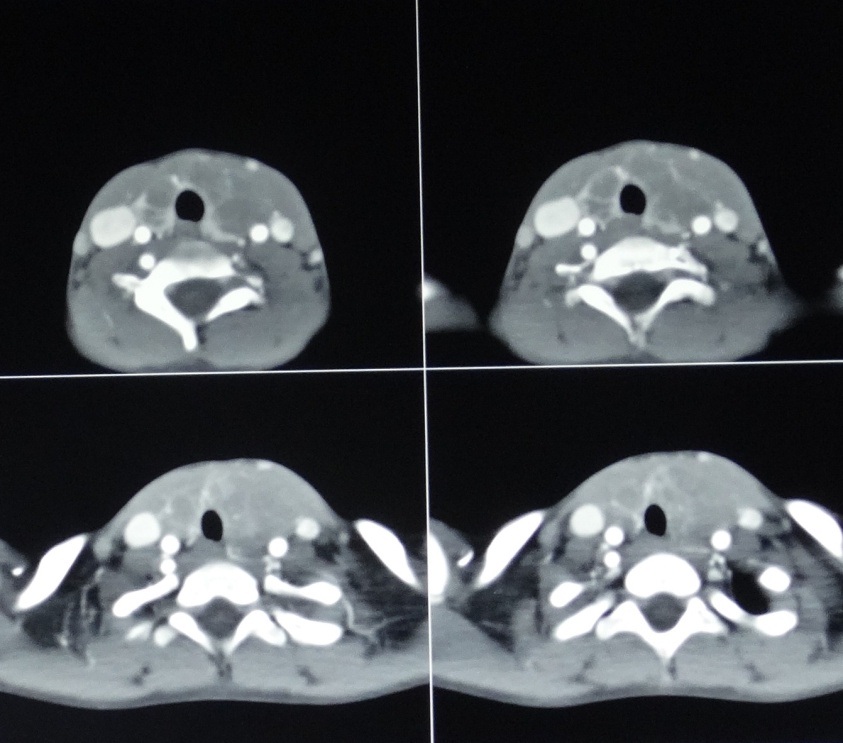
| 35 | Contrast-enhanced CT Neck [Table/Fig-6] | A diffusely enlarged thyroid gland with multiple lymph nodes on both side | |
| 36 | CT Brain, Chest & Abdomen | Within normal limits | |
| 37 | 18FDG PET CT scan whole body [Table/Fig-7] | Active disease in the multiple coalesced hypodense nodules involving both the lobes of the enlarged thyroid. Hyper metabolic bilateral level 2, 3 and 5 lymph nodes | |
Ultrasonography of abdomen with skeletal survey were done and found to be normal. An 18FDG PET CT scan whole body was done to detect the systemic involvement which showed active disease in the multiple coalesced hypodense nodules involving both the lobes of the enlarged thyroid [Table/Fig-6]. Hyper metabolic bilateral level 2, 3 and 5 lymph nodes were seen with no active disease elsewhere in the body.
CT Neck with contrast showing the enlarged thyroid with multiple cervical nodes
Patient was started on intravenous vinblastine (6mg/m2) with oral prednisolone once a week for six weeks. A repeated 18FDG-PET CT scan showed significant reduction in significant decrease in size and metabolic activity of the multiple coalesced hypodense nodules in both lobes of thyroid. Patient was continued on injection vinblastine once every three weekly till one year. His thyroid function was within normal limits throughout the treatment. The thyroid swelling gradually reduced over the course of the treatment and was undetectable at the end of the same. An 18FDG-PET CT done after one year showed absence of any significant disease in thyroid or elsewhere in the body. He tolerated chemotherapy well and is on regular follow up for last one year.
Discussion
Langerhans cell histiocytosis (LCH) is a neoplastic proliferation of Langerhans cells, with expression of CD1a, S-100 protein and the presence of Birbeck granules by ultrastructural examination [1,2]. The annual incidence has been estimated to be 4 per million and there seems to be a slight predominance of cases in males [3]. The median age at diagnosis for all disease variants is 2 to 3 years [3]. LCH can present along a continuum of illness, ranging from indolent to explosive disease [3]. More frequently affected are the bone (80%), the skin (33%), and the pituitary (25%) followed by the liver, spleen, the hematopoietic system and the lungs (15% each). Finally, the lymph nodes (5-10%) and the central nervous system excluding the pituitary (2-4%) are the other possible localization sites of the disease.
Current literature documents 75 cases of LCH involving the thyroid gland where only 23 cases reported the isolated thyroid involvement in English literature [3]. The thyroid involvement of LCH is more reported in adults than children (47 adult vs 18 paediatric cases) with slight female predilection (1.4:1). LCH cases involving the thyroid gland present with diffuse (39 /66 cases) or nodular thyroid (17/66) enlargement [3]. These cases were euthyroid (40.9%) or hypothyroid (19.7%) with less incidence of subclinical hypothyroidism or hyperthyroidisim (10.6% vs. 1.5%, respectively) [3].
In a case of thyromegaly, ultrasonography and FNAC needs to be done as a part of preliminary evaluation. In the thyroid, LCH had been mistaken for poorly differentiated carcinoma on histology [4] or lymphocytic thyroiditis or papillary carcinoma on fine-needle aspiration as in our case [5]. They have been diagnosed as LCH retrospectively, following haemithyroidectomy or total thyroidectomy, either diagnostic or curative, for other suspected clinical entities like medullary carcinoma or adenoma [3,6]. In present case FNAC was inconclusive, so the core biopsy was obtained that surgery can be reserved after obtaining the definite pathological diagnosis, considering the age of the child.
The diagnosis of LCH is confirmed on the detection of Langerhans cell whose nuclei are folded or grooved resembling a coffee bean or lobulated and indented akin to those described in our patient. There may be eosinophils, lymphocytes, neutrophils and plasma cells around these cells some times in large number. The definitive diagnosis requires positive staining of the lesional cells with CD1a and S-100 protein on immunohistochemistry [7].
Systemic involvement is evaluated based on blood counts, total protein, Albumin, Bilirubin, ALT, AST, Alkaline phosphatase, BUN-blood urea nitrogen, Creatinine, electrolytes, ESR, abdominal ultrasound, coagulation studies, bone marrow biopsy, chest radiograph and skeletal radiograph survey. In our case, LCH was limited to thyroid gland only which was confirmed by PET scan. Phillips et al., proposed that if a patient has only a single site of disease by plain films and no suspicion of a vertebral lesion PET scans are an excellent screening modality which provide improved sensitivity for locating active or reparative LCH lesions [8]. In the present case, after six cycles of chemotherapy PET scan was done that showed significant decrease in size and metabolic activity of the multiple coalesced hypodense nodules in both lobes of thyroid and draining nodes. The decrease of FDG uptake when treatment is effective, makes 18FDG PET CT scan the imaging of choice to assess the treatment when compared to other radiographic modalities, especially in soft tissue involvement [8].
Should it be thyroidectomy or chemotherapy? The review of literature may suggest resection of LCH by subtotal, near total, or total thyroidectomy is the treatment of choice for localized LCH to the thyroid [6]. 42.4% of the reported cases received surgery for thyroid involvement, 30.3% received surgery and adjuvant chemo-radiotherapy, and 18% received chemo-radiotherapy only [3]. Moreover, it is evident that in most of the cases where surgery was suggested, surgery had been done prior to diagnosis and those patients were followed up.
Definitive management in a case where a diagnosis was attained preserving the thyroid gland is still a controversy owing to the lack of prospective randomised studies [9]. One case report proposed thyroidectomy as the treatment but did not rationalise the role of chemotherapy [10]. In the present case expert opinion from the Histiocyte Society was sought for and was advised to proceed with chemotherapy with vinblastine and prednisolone. Thyroid swelling started reducing during the treatment and PET scan done after the complete course showed nil significant active disease within the gland and absence of any new lesions. Only direct RT to the neck would permanently damage the thyroid function. It is possible that the LCH infiltration might nevertheless damage the thyroid gland, but if the thyroid function is normal before the treatment, there is still a chance to preserve the gland function. He remained euthyroid during and after the course of chemotherapy with no adverse effects. Owing to the rarity and lack of prospective randomised studies, there are limitations in the available clinical data in providing a definitive management protocol.
Conclusion
LCH with solitary involvement of thyroid gland is one of the rarest presentations. The present report signifies the role of chemotherapy and organ preservation in a case of primary LCH thyroid when compared to thyroidectomy. Only a prospective randomized trial can fill the void in the available clinical data that will answer this question and establish the treatment protocols in LCH limited to thyroid.
[1]. Henry K, Langerhans cell histiocytosis. In: Barnes L., Eveson J.W., Reichart P., Sidransky D.(Eds)World Health Organization Classification of Tumours. Pathology and Genetics of Head and Neck Tumours 2005 LyonIARC Press:358 [Google Scholar]
[2]. Nicholson Stacy H, Langerhans Cell Histiocytosis. In: Greer JP, Rodgers GM, Foerster J, etalWintrobe’s Clinical Hematology 2004 11th editionPhiladelphia, USALippincott Williams & Wilkins:3681-97. [Google Scholar]
[3]. Patten DK, Wani Z, Tolley N, Solitary Langerhans Histiocytosis of the Thyroid Gland: A Case Report and Literature ReviewHead and Neck Pathol 2012 6:279-89. [Google Scholar]
[4]. Coode PE, Shaikh MU, Histiocytosis X of the thyroid masquerading as thyroid carcinomaHum Pathol 1988 19:239-41. [Google Scholar]
[5]. Kitahama S, Iitaka M, Shimizu T, Serizawa N, Fukasawa N, Miura S, Thyroid involvement by malignant histiocytosis of Langerhans cell typeClin Endocrinol 1996 45:357-63. [Google Scholar]
[6]. Vilallonga R, Ciudin A, Fort JM, Isolated Langerhans cell histiocytosis of the thyroid in an adult female: one-year followupInt J Endocrinol 2011 2011:898302doi:10.1155/2011/898302 [Google Scholar]
[7]. Yap WM, Langerhans cell histiocytosis involving the thyroid and parathyroid glandsMod Pathol 2001 14:111-15. [Google Scholar]
[8]. Phillips M, Allen C, Gerson P, McClain K, Comparison of FDG-PET scans toconventional radiography and bone scans in management of Langerhans cell histiocytosisPediatric blood & cancer 2009 52(1):97-101. [Google Scholar]
[9]. Kevin L, Langerhans cell histiocytosis of the thyroid glandAmerican Journal of Otolaryngology 2008 29(3):201-04.doi: 10.1016/j.amjoto.2007.05.004 [Google Scholar]
[10]. Vilallonga R, Ciudin A, Fort JM, Isolated Langerhans Cell Histiocytosis of the Thyroid in an Adult Female: One-Year Follow upInternational Journal of Endocrinology 2011 2011:8983024 pages, 2011. doi:10.1155/2011/898302 [Google Scholar]