Cardiovascular disease is the number one killer disease worldwide as well as in India [1]. According to a WHO survey, in India 24.8% people die annually due to various cardiovascular diseases, among which coronary artery disease (CAD) being the leading cause [2]. Atherosclerosis is thought to play a key role in the pathogenesis of CAD [3]. The offspring of patients with CAD are at increased risk for atherosclerosis. The reported risk in first degree relatives ranges from 1.5-7% [4]. Recent research suggests that asymptomatic subjects with zero coronary artery calcium score and a positive family history of CAD are at increased risk for cardiovascular events compared with those without a family history of CAD [5]. Atherosclerosis starts very early in life, slowly progressing over decades before manifesting clinically. The anatomic lesions of atherosclerosis begin in some children as early as infancy, especially those with a positive family history of CAD [6].
Increased common carotid arteries intima-media thickness (CIMT) is related to generalized atherosclerosis of all vascular beds especially the coronaries and is associated with increased risk of future myocardial infarction and stroke [7]. Several studies in middle-aged and elderly adults with family history of CAD reveal structural and functional changes in their arterial wall assessed by non-invasive methods like CIMT and brachial artery reactivity, whereas similar studies are lacking in the younger age group [8,9]. CIMT measurement is increasingly used as a surrogate marker for subclinical atherosclerosis because of its ability to predict future clinical cardiovascular endpoints [10]. CIMT measurements can be easily done using B mode ultrasonography. This high resolution, non-invasive technique is one of the best methods to detect early atherosclerotic changes since it is precise, reproducible, and rapidly applicable and demonstrates the arterial wall structure better than any other similar technique [11]. We undertook the present study to investigate whether structural vascular changes related to atherosclerosis are detectable by non-invasive method like CIMT in healthy young adults with family history of CAD.
Materials and Methods
Study population & design
After obtaining the institutional ethical clearance an observational, case-control study was conducted in the Department of Physiology in conjunction with the Department of Internal Medicine and Radiology at SRM Medical College, Hospital and Research Centre, kattankulathur, from August 2014 till May 2015 for a period of 10 months. The study was conducted in accordance with the ethical guidelines for biomedical research on human subjects by Central Ethics Committee on Human Research (CECHR) and those as contained in the “Declaration of Helsinky”.
We included 50 healthy young adults of both sexes (M=35 & F=15) between the ages of 18-25 years with family history of CAD as cases and 50 age and sex matched (M=35 & F=15) subjects without family history of CAD served as controls. Both cases and controls were given an explanatory note, explaining the purpose of the study and the right to deny participation following which due consent on the patient consent form was obtained from each patient prior to inducting them in the study. Subjects with smoking history, alcohol intake, coronary artery anomaly, obesity, who are already being treated for CAD/diabetes and/ anaemia were excluded from the study. Those agreeing for the study underwent high resolution B-mode ultrasonographic evaluation of common carotid artery intima–media thickness. Lipid profile, resting blood pressure and anthropometric measurements were measured.
Cardiovascular disease risk assessment
Cardiovascular disease risk assessment was made in the Internal medicine OPD of SRM Medical College, Hospital and Research Centre, kattankulathur according to standardized protocols. All subjects underwent a detailed clinical examination and were administered a standard questionnaire to obtain information about smoking status, history of diabetes, hypertension and family history of CAD. Family history of CAD was defined as mother or father having a myocardial infarction, percutaneous coronary angioplasty, coronary artery bypass surgery, angina pectoris or unexplained death at any age (males < 55 years and females < 65 years). Anthropometric measurements like height and weight were measured with indoor clothes and without shoes [12]. Blood pressure was measured in accordance with the British hypertension society guidelines [13]. It was measured as a mean of three readings taken at 2 minutes interval using a periodically calibrated mercury sphygmomanometer.
Biochemical Investigation
Lipid profile
Fasting blood sample were drawn for measurement of serum total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C) and very low-density lipoprotein (VLDL-C) cholesterol using standardized commercially available SIEMENS kit [14]. Serum LDL-C and VLDL-C were calculated from the estimated values of TC, TG and HDL-C, using Frieldwald’s equation [15].
CIMT measurement
High resolution ultrasound of the right and left carotid arteries was performed in all subjects using PHILIPS HD 7 ultrasound machine with L12-3 broadband linear probe. A single qualified radiologist who was unaware of the subjects status performed all the studies to avoid inter-observer variations. The measurements were made with the patient lying in supine position with neck extended and turned to the opposite side. Optimal B-mode settings of gain, depth, focal zone placement and compression were individually adjusted for each vessel to enhance arterial wall structures and image quality. First, bilateral cervical carotid arteries were screened in cross section to see the luminal patency and for the presence of plaques in the longest extension possible from the base of the neck to the carotid bulb and bifurcation. Then longitudinal images were obtained and the distance between the far two echogenic lines representing the intima media thickness (IMT) of the arterial wall of the distal common carotid artery (CCA) was measured within 1 cm proximal to the carotid bulb. The maximal IMT at this site in the right and left CCAs was measured by manual technique using electronic calipers [16]. The lumen diameter between the near and far wall intima media interfaces was imaged at this site on both sides. The reproducibility of the measurement was assessed by repeating the scan in 20 subjects after a period of 1 week by another radiologist. The mean absolute difference in intima–media thickness on two occasions was 0.03±0.04 mm (coefficient of variation, 2.8%).
Statistical Analysis
Data were compiled in MS excel Office 2010 and analysis was performed in SPSS version 22. Values were expressed as mean±SD. Comparisons between participants with a family history of CAD and controls were made using unpaired Student t-test. Odds ratio with 95% confidence interval for a family history of CAD was calculated by conditional logistic regression analysis. Pearson correlation was used to study the relationship between the variables. P-value of <0.05 was considered to be significant.
Results
The clinical and biochemical characteristics of the cases and controls are given in [Table/Fig-1]. They were similar with regards to age, sex, BMI, pulse rate, systolic and diastolic blood pressure. Participants in both groups had comparable dietary habits. Cases had significantly higher levels of TG, TC and VLDL-C compared to controls. There was no significant difference in the serum concentration of HDL-C and LDL-C.
Clinical and biochemical characters of study participants
| Parameters | Control (N = 50) | Case (N = 50) | p-value |
|---|
| Age(Yrs) | 23.2 ± 4.6 | 22.7 ± 4.8 | 0.61 |
| Height(Cms) | 162.4 ± 11.4 | 165.5 ± 9.6 | 0.14 |
| Weight(Kg) | 60.6 ± 9.2 | 64.6 ± 13.8 | 0.09 |
| BMI(kg/m2) | 23 ± 2.9 | 23.4 ± 3.8 | 0.55 |
| SBP(mmHg) | 109.8 ± 14.6 | 109.5 ± 12 | 0.92 |
| DBP(mmHg) | 72.4 ± 9.6 | 74.2 ± 9.3 | 0.34 |
| PP(mmHg) | 37.4 ± 10.5 | 35.3 ± 8.2 | 0.27 |
| MAP(mmHg) | 84.8 ± 10.4 | 86 ± 9.6 | 0.58 |
| PR(min) | 79.4 ± 9.6 | 79.3 ± 10.9 | 0.99 |
| LIPID PROFILE |
| TGL(mg/dl) | 109.5 ± 43.1 | 164.7 ± 89.1 | <0.001* |
| TC(mg/dl) | 119.7 ± 22.8 | 161.5 ± 48.3 | <0.001* |
| LDL(mg/dl) | 80.8 ± 27.1 | 96.0 ± 51.6 | 0.07 |
| HDL(mg/dl) | 36.8 ± 10.4 | 33 ± 12.2 | 0.1 |
| VLDL(mg/dl) | 19.8 ± 6.5 | 30.2 ± 12.2 | <0.001* |
BMI- Body mass index, SBP- Systolic blood pressure, DBP- Diastolic blood pressure, PP- Pulse pressure, MAP- Mean arterial pressure, PR- Pulse rate, TGL- Triglycerides, TC- Total cholesterol, LDL- Low density lipoprotein, HDL- High density lipoprotein, *p<0.001- significant
The results of ultrasonographic studies are summarized in [Table/Fig-2]. Participants with a family history of CAD had greater intima–media thickness of the common carotid artery compared to controls (Values for combined sides, 0.57±0.08 mmvs. 0.46±0.05 mm; p<0.001).
Ultrasound findings of study participants
| Parameters | Control (N = 50) | Case (N = 50) | p-value |
|---|
| Right side |
| CIMT(mm) | 0.447±0.054 | 0.581±0.089 | <0.001* |
| Lumen diameter (Cms) | 0.559±0.033 | 0.561±0.034 | 0.77 |
| Left side |
| CIMT(mm) | 0.468±0.054 | 0.570±0.091 | <0.001* |
| Lumen diameter (Cms) | 0.564±0.033 | 0.565±0.033 | 0.82 |
| Average of both sides |
| CIMT(mm) | 0.457 ± 0.050 | 0.576 ± 0.084 | <0.001* |
| Lumen diameter (Cms) | 0.561±0.025 | 0.563±0.024 | 0.79 |
CIMT- Carotid artery intima media thickness, *p<0.001- significant
Pearson correlation was used to study the relationship between the study variables. In [Table/Fig-3] the correlation is illustrated by a scatter plot showing the association between CIMT and triglyceride in cases and [Table/Fig-4] shows the association between CIMT and triglyceride in controls. Triglycerides and CIMT were the variables that entered the multivariate logistic regression. Triglycerides turned out to be insignificant at the end of logistic regression. Carotid intima–media thickness was seen to be independently associated with family history of CAD (odds ratio= 5.36 with 95% confidence interval of 1.84 – 10.53, p=0.003).
Scatter plot showing the association between CIMT and triglycerides in cases

Scatter plot showing the association between CIMT and triglycerides in controls

Discussion
In the present study, we found a significantly higher CIMT compared to controls [Table/Fig-5]. To the best of our knowledge this is the first study demonstrating an increased CIMT in apparently healthy, young individuals with no cardiovascular disease risk other than a family history of CAD. There are very few studies assessing subclinical atherosclerosis in younger age group, as most of them are targeted towards symptomatic population like the middle aged and elderly. Our findings are consistent with similar studies where a family history of premature myocardial infarction is associated with increased CIMT and an unfavourable lipid profile [17,18].
Comparison of CIMT between cases and controls

Genetic factor plays a key role in the progression of atherosclerosis [19]. Its occurrence is exacerbated in the presence of risk factors. In a study by Otaki et al., it is seen that compared with other CAD risk factors a positive family history in young subjects is the strongest clinical predictor of future myocardial infarction [20]. Of late, it is being increasingly recognized that most early cardiovascular events occur in subjects with a positive family history of cardiovascular disease [21]. Offsprings of parents with CAD are at high risk of premature atherosclerosis. Researchers have proved that children of parents with CAD have significantly higher levels of total serum cholesterol and triglycerides and decreased levels of high density lipoprotein and increased low density lipoprotein compared to controls [22]. Mendes et al., noted that dyslipidaemia is more prevalent in children and adolescents with family history of CAD and they responded to dietary intervention [23]. Similar to these studies and suggesting the role of hereditary factors, our subjects also exhibited significantly higher levels of TG, TC and VLDL-C [Table/Fig-1] all pointing towards an adverse lipid profile. Recent evidences have highlighted the role of hypertriglyceridemia in the pathogenesis of CAD. Hypertriglyceridemia is associated with increased VLDL production and decreased clearance. It decreases clearance by reducing the activity of lipoprotein lipase, hepatic TG lipase and novel receptors such as GPI anchored HDL-binding protein 1 (GPIHBP1) [24]. Also, various triglyceride rich lipoproteins (TRLs) including VLDL and VLDL remnants are seen to stimulate atherogenesis independently of LDL [25]. TRLs causes enhanced recruitment and attachment of monocytes through the action of endothelial derived inflammatory proteins such as tumor necrosis factor-α (TNF-α), interleukin (IL)-1β, monocyte chemotactic protein-1, intercellular adhesion molecule-1, and matrix metalloproteinase-3 [26]. It also causes direct vascular cytotoxicity through lipolytic by products [27]. Further it is seen that TRLs suppress the protective effect of HDL by blocking sterol efflux from monocytes and macrophages[28]. Thus triglycerides promote atherogenesis by increased expression of adhesion molecules leading to increase in intima thickness which is thought to be an early sign of atherosclerosis [29]. This explains the direct association between carotid intima media thickness and triglyceride observed by us [Table/Fig-3].
The association between hyperlipidemia and CAD has been studied vastly [30,31]. The arterial wall abnormalities [Table/Fig-5&6] seen in our subjects could be precipitated by the dyslipidemia occurring them. It is postulated that there is increased availability of vasoconstricting factors and reduced nitric oxide levels in offsprings with family history of CAD. This leads to atherosclerotic changes like smooth muscle proliferation along with lipoproteins and macrophage deposition in the arterial wall [32]. The increased CIMT observed by us indicates that young arteries of subjects with genetic predisposition are more susceptible to the atherogenic effect of raised lipids. It is worthy to note that there was no difference in the lumen diameter of both cases and controls [Table/Fig-2]. This represents the initial stages of vascular remodeling in response to atherosclerosis. Though initially thought to be beneficial this compensatory process is limited as the arteries lose their elasticity over time [33]. Thus it is clear that structural change in the arterial wall starts occurring at a very young age in subjects with a familial predisposition to CAD. These early morphological changes in the arterial wall can be easily assessed by high resolution B mode scan of the carotid arteries intima-media thickness. This non-invasive, easily available and rapid technique considered one of best methods in detection of early stages of atherosclerosis will help us in identifying such population at risk [34]. As these are the individuals who will benefit the most from primary prevention strategies like life style modification and dietary invention.
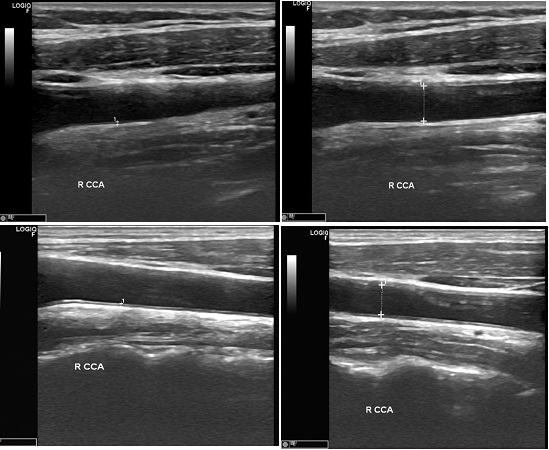
Measurement of CIMT
Panel (A1) Shows thickness and (A2) Shows the lumen diameter in family history negative subjects
Panel (B1) Shows increased thickness and (B2) Shows the lumen diameter in family history positive subjects
CIMT- carotid intima-media thickness, RCCA- Right common carotid artery
Limitations
Our study has few limitations. First, family history was obtained from direct patient query. Though parents of cases were patients who are being treated for CAD in our hospital, health status of the control subject’s parents were entirely based on their self-report. Second, our study is observational in nature, hence the role of unmeasured confounders in the association between family history of CAD and CIMT cannot be ruled out. Finally due to financial constraints we were not able to measure other cardiovascular risk factors like tissue plasminogen activator, serum fibrinogen and apolipoproteins.
Conclusion
Our study shows that structural abnormalities of the arterial wall occur at a very early age in young adults with family history of CAD. CIMT measurement is a non-invasive and highly reproducible technique that can easily quanjpgy the presence of subclinical atherosclerosis in these subjects.
BMI- Body mass index, SBP- Systolic blood pressure, DBP- Diastolic blood pressure, PP- Pulse pressure, MAP- Mean arterial pressure, PR- Pulse rate, TGL- Triglycerides, TC- Total cholesterol, LDL- Low density lipoprotein, HDL- High density lipoprotein, *p<0.001- significant
CIMT- Carotid artery intima media thickness, *p<0.001- significant