Serous Microcystic Adenocarcinoma of Pancreas Infiltrating Into Spleen: A Case Report
Valarmathi Kadhirvel1, Sathyalakshmi Ramu2, Nidhi Mishra3, Mary Lilly Susai Adaikalam4, Ramya Venkatesan5
1 Professor, Department of Pathology, Medical College, Dr.M.G.R. Medical University Government Stanley, Chennai, Tamil Nadu, India.
2 Assistant Professor, Department of Pathology, Medical College, Dr.M.G.R. Medical University Government Stanley, Chennai, Tamil Nadu, India.
3 Post Graduate, Department of Pathology, Medical College, Dr.M.G.R. Medical University Government Stanley, Chennai, Tamil Nadu, India.
4 Professor, Department of Pathology, Medical College, Dr.M.G.R. Medical University Government Stanley, Chennai, Tamil Nadu, India.
5 Post Graduate, Department of Pathology, Medical College, Dr.M.G.R. Medical University Government Stanley, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K. Valarmathi, Old No 8/5, New No 36/5,4th Cross Street, Trustpuram, Kodambakkam, Chennai-24, India. E-mail : valarmathimd@gmail.com
Cystic tumours of pancreas account for 5-10% of all pancreatic neoplasms and serous tumours represent 1% among those tumours. Most of the serous tumours are benign and very rarely they infiltrate adjacent organs like liver and spleen. Herewith we present a rare case report of serous cystadenocarcinoma of pancreas in a 65-year-old woman. The tumour involved the body and tail of pancreas and contiguously invaded the spleen. The histopathology of tumour was similar to serous cystadenoma with mild nuclear hyperchromasia and atypia. The spleen showed tumour infiltration as microcysts diffusely infitrating the red pulp.
Ductal cytokeratins, malignant cystic pancreatic neoplasms, serum amylase
Case Report
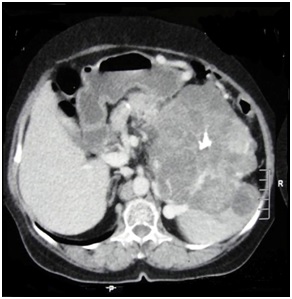
A 65-year-old female presented to the Department of Surgical Gastroenterology with complaints of pain in the epigastrium and in the left hypochondrium for a period of 6 months, increasing in intensity for 1 month with pain radiating to the back. General and systemic examinations were unremarkable. On ultrasound abdomen, there was a cystic tumour in the body of pancreas. Serum amylase level was 250 U/L. After initial symptomatic treatment, CT scan abdomen was done, which showed a heterogeneously enhancing left sided abdominal mass involving body and tail of pancreas along with spleen, the origin of mass could not be made out [Table/Fig-1]. A provisional diagnosis of solid pseudo papillary tumour of pancreas was given [Table/Fig-2].
CT scan showing a large heterogenous mass involving body, tail of pancreas and spleen
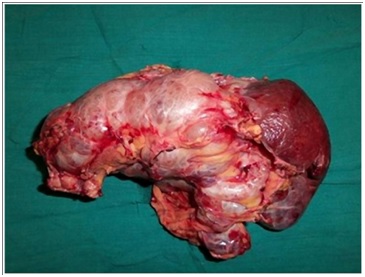
Gross- External appearance of distal pancreatectomy with splenectomy
Distal pancreatectomy with splenectomy was done and specimen was sent for histopathological examination.
The resected specimen of pancreas measured 14x13x10 cm and spleen measured 12x12x5 cm. External surface of pancreas was lobulated and cut surface showed multiple cystic spaces of variable sizes filled with serous fluid with a stellate scar. The external surface of spleen was also nodular and it was adherent to the pancreatic mass. The cut surface of the spleen was entirely replaced by grey white spongy areas [Table/Fig-3a,b].
Gross- Cut surface showing tumor infiltrating spleen
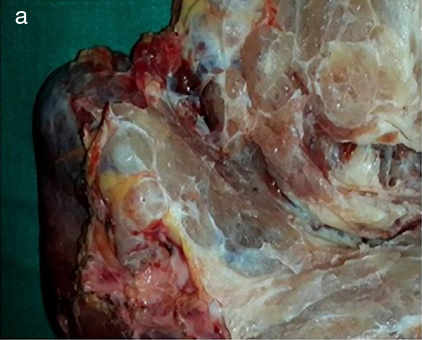
Cut surface of spleen showing tumor infiltration as multiple microcystic spaces of varying sizes

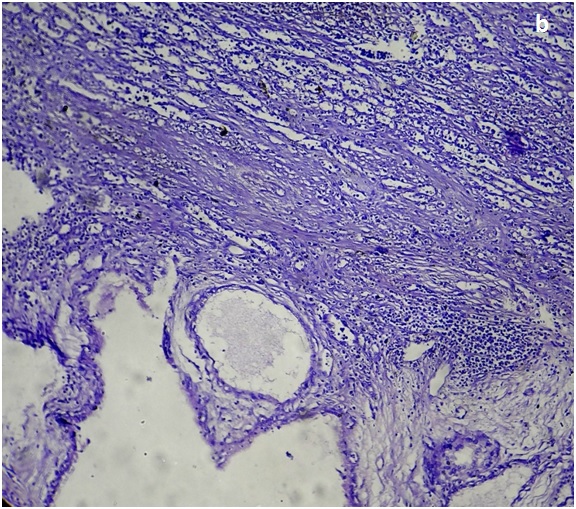
Histopathological examination showed a neoplasm composed of multiple cystic spaces lined by a single layer of cuboidal cells with clear cytoplasm and well-defined cytoplasmic border with small round hyperchromatic nuclei. Focal areas showed hyalinization. The tumour is seen infiltrating the spleen [Table/Fig-4a,b].
H&E (10x) – Multiple cystic spaces of variable size lined by cuboidal cells
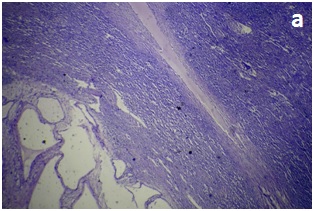
H&E (10x) –Tumour infitrating into spleen
The tumour is diagnosed as serous cystadenocarcinoma infiltrating into the spleen.
Discussion
Cystic pancreatic tumours can be primary or secondary due to cystic change. The neoplasms with secondary changes should be differentiated from tumours with a cystic configuration (i.e., cystadenomas and cystadenocarcinomas). Majority of these cystic tumours are of benign nature and present as cystadenoma and 1% of cases present as malignant cystic neoplasms [1,2].
In 1978 Compagno and Oertel classified cystic neoplasm of pancreas into two different types based on their biological behaviour. First type is serous cystadenoma. Second type is mucinous cystadenoma [3]. Recent Classification of pancreatic neoplasms is based on WHO nomenclature.
Mucinous cystic tumours of the pancreas are common in perimenopausal women and are characterized by the formation of large multilocular or unilocular cysts lined by tall, mucin-producing cells, often forming papillae. Most are found in the body and tail rather than in the head. The underlying stroma is often very cellular resembling ovarian stroma. Extensive sampling of the tumour is done to rule out malignancy [4].
The four variants of serous adenomas are macrocystic serous cystic neoplasm, solid serous neoplasm, Von Hippel-Lindau (VHL) associated serous cystic neoplasm and mixed serous-neuroendocrine neoplasm [5]. The term serous cystadenoma refers to the most frequent microcystic type [6].
Microcystic cystadenoma, also known as glycogen-rich or serous cystadenoma presents grossly as a large multiloculated mass. The cut surface shows honey comb appearance with central scar and the individual cystic cavities are small and filled with a clear serous fluid. Microscopically, they are composed of multiple small cysts lined by small, flat or cuboidal cells with abundant PAS (periodic Schiff) positive glycogen [6].
Malignant cystic pancreatic tumours are very rare, accounting for about 1% of all pancreatic malignancies. Cystic pancreatic neoplasms comprise 1-2% of pancreatic lesions and most of these lesions are cystadenomas [5]. The first case of a pancreatic serous cystadenocarcinoma was reported by George et al., in 1989 [7]. Serous cystadenocarcinoma is considered malignant when tumour invades surrounding tissues and organs or when distant metastasis is present [6]. According to the literature most cases of serous cystadenocarcinoma show synchronous or metachronous liver metastasis, invasion into the spleen, stomach, lymphnode infiltration, lung, adrenals, peritoneal and colonic mesentry metastasis [8–10]. So far 26 cases of serous cystadenocarcinoma have been reported in the literature [5].
The immuno profile is characterized by positivity for the ductal cytokeratins 7, 8, 18, and 19; inhibin; Glut1; MUC6; MUC1; and neuron-specific enolase and negativity for CEA [11].
Serous cystadenocarcinomas cannot be distinguished from its benign counterpart solely on the basis of histological parameters and clinically may be difficult [12], except for local invasion and distant metastasis. Therefore thorough careful gross and microscopic examination is mandatory.
Conclusion
The prevalence of serous cystadenocarcinoma is very rare. Differentiation between serous microcystic adenoma and serous cystadenocarcinoma is very difficult both histologically and clinically but is very important to know the diagnosis for treating the patient. Hence extensive sampling of the tissue has to be done along with immunohistochemical markers to confirm the diagnosis.
[1]. Siech M, Tripp K, Schmidt-Rohlfing B, Mattfeldt T, Widmaier U, Gansauge F, Cystic tumours of the pancreas: diagnostic accuracy, pathologic observations and surgical consequencesLangenbecks Arch Surg 1998 383:56-61. [Google Scholar]
[2]. Horvath K, Charbot JA, An aggressive resectional approach to cystic neoplasms of the pancreasAm J Surg 1999 178:262-74. [Google Scholar]
[3]. Compagno J, Oertel JE, Microcystic adenomas of the pancreas (glycogen-rich cystadenomas): a clinicopathologic study of 34 casesAm J Clin Pathol 1978 69:289-98. [Google Scholar]
[4]. Volkan Adsay N, Cystic lesions of the pancreasMod Pathol 2007 20(Suppl 1):S71-93. [Google Scholar]
[5]. Bramis K, Petrou A, Papalambros A, Manzelli A, Mantonakis E, Brennan N, Serous cystadenocarcinoma of the pancreas: report of a case and management reflectionsWorld J Surg Oncol 2012 10:51 [Google Scholar]
[6]. Bosman FT, Carneiro F, Hruban RH, Theise ND, WHO classification of tumours of the digestive systemVolume 34th editionIARC WHO Classification of Tumours; No3 [Google Scholar]
[7]. George DH, Murphy F, Michalski R, Ulmer BG, Serous cystadenocarcinoma of the pancreas: A new entity?Am J Surg 1989 13:61-66. [Google Scholar]
[8]. Wu CM, Fischerman EK, Hruban RK, Serous cystic neoplasm involving the pancreas and liver: A unususal clinical entityAbdom Imaging 1999 24:75-77. [Google Scholar]
[9]. Kimura W, Makuutchi M, Operative indications for cystic lesions of the pancreas with malignant potential: Our experienceHepatogastroenterology 1999 46:483-91. [Google Scholar]
[10]. Abe H, Kubota K, Mori M, Mingawa M, Noise T, Kimura W, Serous cystadenoma of the pancreas with invasive growth: Benign or malignant?Am J Gastroentrol 1989 93:1963-66. [Google Scholar]
[11]. Mohr VH, Vortmeyer AO, Zhuang Z, Histopathology and molecular genetics of multiple cysts and microcystic (serous) adenomas of pancreas in VHL patientsAm J P Pathol 2000 157:1615-21. [Google Scholar]
[12]. King JC, Ng TT, White SC, Cortina G, Reber HA, Hines OJ, Pancreatic serous cystadenocarcinoma: a case report and review of the literatureJ Gastrointest Surg 2009 13:1864-68. [Google Scholar]