Virilizing Ovarian Steroid Cell Tumor: A Rare Case
Aishwarya Bettegowda1, Nagarathnamma Rangaiah2, Nagendra Prasad3, Savitha Channaveeregowda4
1 Post-Graduate, Department of Obstetrics and Gynaecology, Rajarajeswari Medical College, Bangalore, Karnataka, India.
2 Professor & HoD, Department of Obstetrics and Gynaecology, Rajarajeswari Medical College, Bangalore, Karnataka, India.
3 Associate Professor, Department of Obstetrics and Gynaecology, Rajarajeswari Medical College, Bangalore, Karnataka, India.
4 Assistant Professor, Department of Obstetrics and Gynaecology, Rajarajeswari Medical College, Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aishwarya Bettegowda, No.11. Malarasi,18th Cross, 26th Main, Annaiahreddy Layout, Sarakkikere, Annaiahreddy Layout, JP Nagar 6th Phase, Bangalore-560078, India.
E-mail: aishwarya.bgowda@gmail.com
Ovarian steroid cell tumours are fewer than 5 percent of sex-cord stromal tumours and 0.1% of all ovarian tumours. The average age at diagnosis is the mid-20s, but patients can present at virtually any age. We present a case of 38-year-old multipara with history of secondary amenorrhea, clinical signs & symptoms of virilization developed over the past 5 years. With elevated (115ng/dL) serum testosterone level and radiological findings of a left adnexal solid mass; the patient was suspected to have a virilizing tumour of left ovary. Laparoscopic left salpingo-oophorectomy was performed. Histopathology revealed tumour cells in small nests with vacuolated to eosinophilic cytoplasm with nuclear atypia completely replacing the ovarian tissue suggestive of steroid cell tumour (NOS) of ovary. The patient was discharged and advised for follow up with serum testosterone levels after 3 weeks.
Serum testosterone, Sex-cord stromal tumours, Virilizing tumour
Case Report
A 38-year-old moderately built multiparous woman, a mother of 3 children, with her last child birth 10 years back, delivered vaginally without any complications, not tubectomised, who had attained menarche at 14 years of age presented with complaints of amenorrhea for 5 years and in the last two years associated with an increase in the facial and body hair but with frontal balding. The patient’s sister had similar complaints of increased facial and body hair.
She had low-pitched, deepened female voice, a male pattern alopecia, temporal recession of hairline, obvious facial hair, grade 2 acne and a BMI of 24.8 [Table/Fig-1]. Her breasts were normal and she had severe hirsutism affecting the chest, anterior abdominal wall, and thighs with a Ferriman Gallwey scoring of 26/36. On per-abdomen examination there were no palpable masses. On per speculum & per vaginal examination her cervix was mildly hypertrophied, uterus was anteverted, normal size, mobile, with left forniceal fullness, non-tender.
Picture shows male pattern alopecia with temporal recession of hairline

The complete blood picture, renal and liver parameters were within normal limits and relevant tumour markers were found to be normal. The Serum testosterone level was 115 ng/dl (normal: < 60 ng/dl).
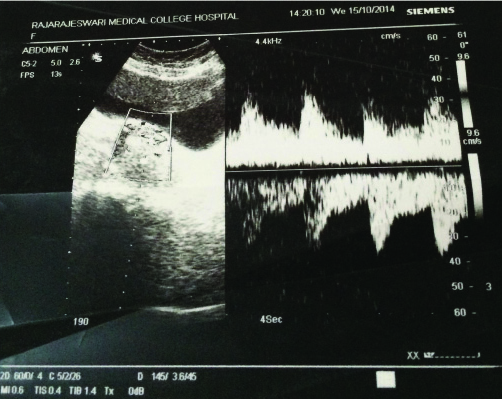
Ultrasound abdomen showed an enlarged left ovary with echogenic solid mass approx. 5.3 x 3 x 5 cm with increased vascularity [Table/Fig-2]. Virilization of ovarian tumour was suspected. MRI reported left adnexal solid mass arising from the left ovary adjacent to the fundus of the uterus and urinary bladder with F/S/O Ovarian Dermoid.
USG showing echogenic solid mass with increased vascularity
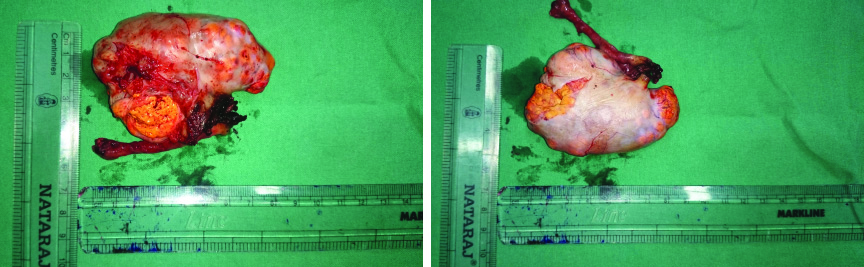
Laparoscopic left salphingo-oopherectomy under GA was performed. On gross examination the uterus, right ovary and B/L tubes appeared unremarkable. Left ovarian tumour of 8.0 x 5.0 x 3.0 cm, with a bosselated yellowish surface with intact capsule was seen [Table/Fig-3,4]. The cut section appeared yellowish, lobulated with tiny cysts in periphery.
Gross specimen showing enlarged left ovary with left fallopian tube with bosselated surface with intact capsule
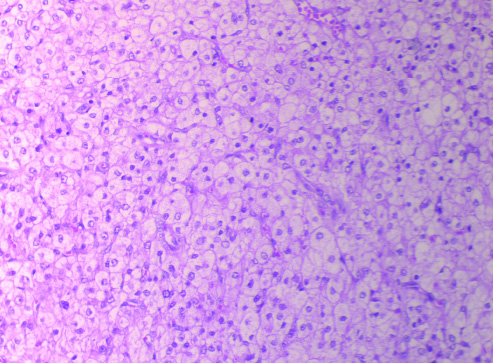
The histopathological examination on microscopy showed a thin rim of ovary with tumour completely replacing the ovarian tissue and cells that were arranged in small nests, thin cords and columns and showed scanty stroma. Tumour cells had distinct cell borders and abundant amount of vacuolated to eosinophilic cytoplasm and mild nuclear atypia with no necrosis [Table/Fig-5]. All the above features led to the impression of a Steroid Cell Tumour (Not Otherwise Specified) of left ovary & on Immunohistochemistry tumour cells were Positive for Calretinin and Inhibin.
HPE on microscopy showing tumour cells in small nests with vacuolated to eosinophilic cytoplasm
The patient was discharged on postoperative day 8 with no complications. Postoperatively a decline in the serum total testosterone levels was noted after a 3-week interval. Patient has been advised regular follow up with the department of OBG and with the department of Dermatology for the treatment of Hirsutism.
Discussion
Ovarian steroid cell tumours are rare functioning sex cord-stromal tumours. These tumours are composed entirely or predominantly of cells that resemble steroid hormone secreting cells and are categorized according to histologic composition of these cells [1]. Ovarian Steroid Cell tumor can be sub-classified into Stromal luteoma, leydig cell tumours and steroid cell tumours not otherwise specified Sex-cord stromal tumours [1,2].
Steroid cell tumours account for 0.1% of all ovarian tumours and the subtype not otherwise specified (NOS) are the most common subtype within this group [3] and typically present in younger reproductive aged women and are associated with androgen excess [1]. In the above reported case, she was in her late reproductive age group (38 years), with elevate testosterone levels.
Virilization or hirsutism is encountered with 3/4th of leydig cell tumours, with half of steroid cell tumours (NOS) and with 12% of stromal tumours [2]. Hayes and Scully reported 63 cases of subtype, not otherwise specified [4]. It was associated with androgenic changes in approximately one half of patients. In case of Virilism; it has to be investigated systematically to determine if high testosterone levels are of an adrenal or ovarian origin. In our case DHEA was found to be within normal limits and in addition Radiological imaging established that cause of virilization was an ovarian aetiology.
Stromal luteoma are clinically benign tumours that by definition lie within the ovarian stroma. They are usually seen in the postmenopausal women. Estrogenic effects are more common but occasionally have androgenic manifestations. Leydig cell tumours are also benign and typically seen in postmenopausal women and secrete testosterone; hence androgenic effects and are distinguished microscopically by crystals of Reinke within the cytoplasm. Steroid cell tumours (NOS) on microscopy are usually composed of vacuolated or eosinophilic cytoplasm replacing the ovarian tissue which may sometime be mistaken for a large stromal luteoma that have grown to reach the ovarian surface or Leydig cell tumour in which Reinke crystals cannot be identified [1]. Hence for the accurate diagnosis along with Microscopy immunohistochemical markers such as Inhibin and Calretinin are useful.
In a series of 63 cases from Massachusetts General Hospital [5], 94% of the tumours were found to be unilateral and 28.6% were malignant. In our case Tumour makers within normal limit and with no ascites or significant lymph nodes and with a unilateral ovarian tumour suggestive of benign origin
The mainstay of treatment for patients with an ovarian Sexcord stromal tumour is surgical resection with staging laparotomy or laparoscopy. In the above case it was staged T1N0M0 and the diagnosis of Virilizing Steroid cell tumour of Left ovary was made by Histo-pathological Examination and Immunohistochemistry.
Conclusion
Virilizing tumours are a rare entity. Androgenicity has to be investigated systematically by to establish if it’s of adrenal or ovarian origin. Ovarian steroid cell tumour is a histological diagnosis and the definitive diagnosis of the subtypes requires immunohistochemistry. The definitive modality of treatment is surgical excision & follow-up with serum testosterone levels and usually does not require any radiotherapy or chemotherapy.
[1]. Schorge Schaffer Halvorson Hoffman Bradshaw Cunningham Williams Gynaecology 2008 2nd edMcGraw-Hill Companies:750 [Google Scholar]
[2]. Jonathan S. Berek, Berek & Novak’s Gynaecology 2012 15th edLippincott Williams & Wilkins Publishers:1098:1406 [Google Scholar]
[3]. Young RH, Scully RE, Steroid cell tumours of the ovaryIn Obstetric & Gynecological Pathology. Edited by Fox H, Wells M 2003 SpainChurchill Livingstone:845-56. [Google Scholar]
[4]. Hayes MC, Scully RE, Ovarian steroid cell tumours (not otherwise specified): a clinic pathological analysis of 63 casesAm J Surg Pathol 1987 11:835-45. [Google Scholar]
[5]. Scully RE, Young RH, Clement PB, Steroid cell tumoursIn Tumours of the Ovary, Mal-developed Gonads, Fallopian Tube, and Broad Ligament 1996 Washington, DCArmed Forces Institute of Pathology:227-38. [Google Scholar]