Thyroiditis is defined as a disorder that involves inflammation of the thyroid gland. Thyroiditis is mainly divided into two broad categories: painless and painful. Among the category of painful types of thyroiditis is subacute (de Quervain’s thyroiditis) which is the most common cause of acute painful thyroiditis [1]. The patients usually present to the otorhinologists with complaints of neck pain, swelling and odynophagia. On examination, there is tenderness at the region of thyroid gland. Although the exact aetiology is unknown, is thought to be a viral inflammatory disorder [2]. The disorder is usually self-limiting over months with a triphasic course of hyperthyroidism followed by hypothyroidism and ending with euthyroidism.
Subacute thyroiditis has been treated with either nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids for years. The response to steroids is often more dramatic and quicker than the response to NSAIDs, but steroids are well known for their side effects over NSAIDs. As subacute thyroiditis is a self-limiting condition, high dose of steroids might be irrelevant to some people. The usual initial dose is 1 mg/kg of prednisolone per day and tapered over six weeks although the basis for this dose has not been established yet by prospective studies [3].
The current study was carried out to study if prednisolone in lower initial dose (20 mg/day tapered over four weeks) is effective in patients with acute painful thyroiditis. Thyroid tenderness and Erythrocyte Sedimentation Rate (ESR) were taken as the guidelines to either continue or discontinue the drug. The patients were followed up carefully and data were analysed.
Materials and Methods
This study was a prospective, cross sectional, observational study carried out in the Department of ENT, Manipal Teaching Hospital, Pokhara, Nepal from 1st August 2012 to 31st March 2015. All the patients with acute anterior neck pain of less than or equal to seven days duration were included in the study. Diagnosis was made in the clinical grounds according to history of anterior neck pain, tenderness thyroid region, tender and swollen thyroid gland, ultrasound of the neck showing increased vascularity of the thyroid gland and raised Erythrocyte Sedimentation Rate (ESR).
Patients with clinical signs suggestive of subacute thyroiditis and ESR of more than 30 mm/h were finally included in the treatment group.
Patients in whom there was contraindication to the use of prednisolone (severe gastritis, Diabetes, hypertension) were excluded from the study.
The patients were administered prednisolone in a starting dose of 20 mg/day (10 mg twice daily) tapered over four weeks. The dose was 10 mg twice daily for 2 weeks and 10 mg once daily day for next 2 weeks. They were also co- prescribed with pantoprazole 40 mg twice daily for 2 weeks to lessen the gastric irritation caused by prednisolone. A performa was made, initial findings of severity of pain and tenderness and ESR were noted, and patients were closely observed for 4 weeks. ESR was repeated in 2 weeks and at 4 weeks. Patients were supposed to be cured if the patient was pain free without thyroid tenderness and ESR of less than 20 mm/hour. Patients were asked to follow up immediately if neck pain recurred within six months post treatment or after that also. All the data were carefully collected and analysed and the results were interpreted.
Results
One hundred and fifty cases of acute painful thyroiditis were included in our study. Twenty-eight patients did not complete the follow up of at least four weeks duration. Therefore, final analysis was made amongst the 122 patients who came for regular follow up of at least 4 weeks.
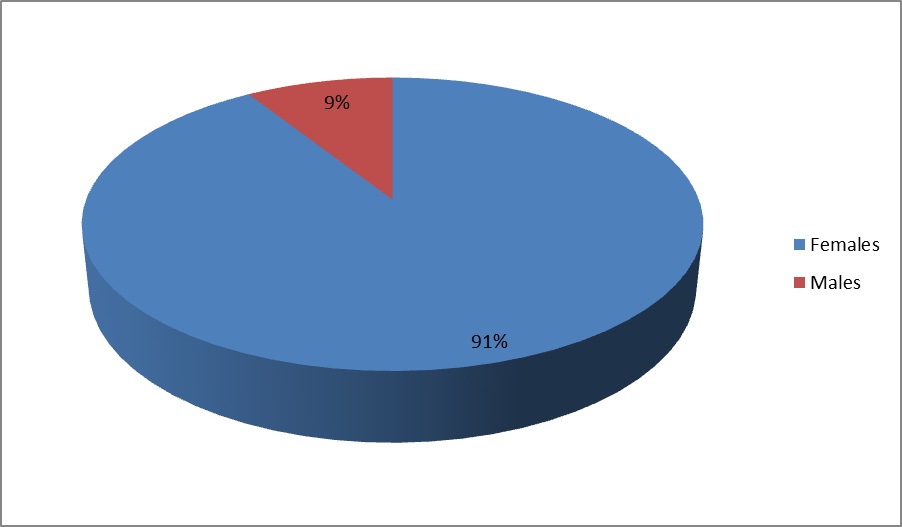
Ages of the patients ranged from 19 years to 69 years with the mean age of 36.58 years. Sixty percent of patients were in the age range of 25-39 years [Table/Fig-1]. Females accounted for 111 patients (91%) and males accounted for 11 in number (9%). Female to Male ratio was 10:1 [Table/Fig-2]. Mean ESR was 57.03 at the time of presentation and 29.63 at two weeks after treatment. The mean ESR was 17.03 mm per hour at 4 weeks after continuation of the drug. ESR was less than or equal to 30 in 74 patients at 2 weeks (60%) and in 117 patients (96%) at 4 weeks after treatment.
Age range of patients under study
| Age Range | No. of cases | Percentage |
|---|
| 15-24 | 12 | 9.8 |
| 25-39 | 73 | 59.8 |
| 40-54 | 31 | 25.4 |
| 55-69 | 6 | 5.0 |
| Total | 122 | 100 |
Pie chart showing Female to male ratio (10:1)
All the patients reported with severe pain in the anterior neck at the time of presentation. The thyroid gland was diffusely tender in 40 patients, on the left side in 49 patients and on the right side in 33 patients. Pain was completely relieved in 115 patients (94%) at 2 weeks after starting the treatment and it was better than previous in seven patients. None of the patients reported worsening of the symptoms after starting the treatment. At the end of four weeks, only two patients had persisting neck pain, which was of low intensity.
The degree of pain and mean ESR at the start of treatment and at two weeks was extremely statistically significant (p<0.0001) according to two tailed p-value for Fisher’s exact test [Table/Fig-3].
Relation between Pain and Mean ESR at the start of treatment and at 2 weeks
| Start of treatment | At 2 weeks of treatment | p-value |
|---|
| Pain | 122 | 7 | p<0.001 |
| Mean ESR | 57 | 29 |
Thyroid Stimulating Hormone (TSH) level was performed at the time of presentation and at four weeks (after completion of steroids). TSH was normal in 91 patients (74.5%) at the time of presentation and low in 31 patients (25.5%). At the end of therapy, it came to normal in 115 patients (94.2%) and was still low in seven patients (5.8%). Antithyroid treatment was started for these seven patients.
Facial swelling was the most common side effect of steroid use. It was present in 114 (93.5%) patients during the course of therapy but no other side effects related to steroid use like diabetes, severe gastritis and hypertension were recorded in our study.
Recurrence occurred in nine patients within six months of completion of therapy. Three patients had recurrence within two months, two patients in third month, three patients in fourth month and one patient in sixth month. Three patients had recurrence after 6 months and therefore 10 mg of prednisolone was continued for them again for next 6 weeks. All of them were controlled by 10 mg of prednisolone.
Discussion
Subacute thyroiditis is an inflammatory disease of thyroid gland. Recent literatures suggest that even viruses like mumps, measles, influenza, adenovirus, infectious mononucleosis, coxsackie virus, EB virus are associated with thyroiditis [4–7]. Ninety-four of our patients (77%) could remember an attack of upper respiratory tract infection before the onset of thyroiditis, which is suggestive of a viral prodrome. This result is similar to a study carried out by Qari FA et al., [8]. In their study, 78% of patients had a viral prodrome.
The disease more often affects females than males. Male to female ratio is widely varied in different studies. This ratio reported in different studies ranges from 1:2 to 1:7 [9–11]. Male to female ratio in our study is 1:10.
Subacute thyroiditis is the most common cause of thyroid pain. The most prominent feature is gradual or sudden onset of pain in the region of the thyroid gland. Our main criterion to define the patients was painful thyroid swelling and that was present in all of our patients. Painful enlargement of the thyroid gland may persist for weeks or months. Symptoms of hyperthyroidism may be present early in the disease and can occur in upto 60% of patients [11]. Later, symptoms of hypothyroidism such as fatigue, constipation, or cold intolerance may occur. Eventually, thyroid gland function returns to normal. However, in our study, only 25% of patients presented with features of hyperthyroidism in the initial presentation.
The hallmark of painful subacute thyroiditis is a markedly elevated erythrocyte sedimentation rate. Erythrocyte sedimentation rate (ESR) is usually higher than 50 mm/h in the initial phase in up to 70% of patients [10,12]. A normal or slightly elevated ESR makes the diagnosis of de Quervain’s thyroiditis relatively unlikely [13]. Mean ESR of all our patients at the time of presentation was 57.03 mm/h, which decreased to 29.63 mm/h at two weeks and 17 mm/h after 4 weeks of treatment. One hundred and fifteen patients were completely pain free at 2 weeks of treatment. As the degree of pain and mean ESR at the start of treatment and at two weeks was extremely statistically significant (p<0.0001) according to two tailed p-value for Fisher’s exact test, we came to the hypothesis that patients with higher ESR have much pain in comparison with those with less ESR which could be due to more inflammation.
There is no definitive treatment of painful subacute thyroiditis. An effective treatment is that which will ameliorate the symptoms and allow the disease to run its spontaneous course in an asymptomatic manner. Nonsteroidal anti-inflammatory drugs have been used in patients with mild or moderate forms of the disorder. In more severe forms of the condition, oral glucocorticoids in various pharmacological dosages have been reported to cause rapid relief of pain and fever within 24-48 hours [12]. Prednisolone is the most commonly used glucocorticoid in treatment of subacute thyroiditis. However, there have been no reports regarding the optimal dose of prednisolone for treatment of subacute thyroiditis. Usual dose of prednisolone in adults is 1 mg/Kg/day or 60 mg/day. Depending on the clinical response and erythrocyte sedimentation rate, steroids are gradually tapered after 1 to 2 weeks and stopped after 4 to 6 weeks. Volpe R initiated prednisolone in dosage of 40 mg daily, with a gradual reduction in dosage over 6 weeks [3]. In a study of 160 patients with subacute granulomatous thyroiditis seen at the Mayo Clinic by Fatourechi V et al., high-dose steroids rapidly and dramatically decreased the pain and thyroid swelling, but the natural course of thyrotoxicosis of 4-6 weeks duration was not altered [14]. Therefore, the glucocorticoid treatment was continued for 4-6 weeks.
However, few studies have been undertaken with low dose of prednisolone over prolonged time to minimize the side effects of high dose steroids. Nishihara et al., performed a study of similar kind [11]. They carried out a study in 219 subjects by using 15 mg/day of prednisolone as the initial dosage and tapered it by 5 mg every 2 weeks (n=219). The number of patients whose thyroiditis improved within 6 weeks was 113 (51.6%). However, 20% of patients needed longer than 8 weeks to recover from the inflammation. The longest duration was for 40 weeks. In our study, 4 patients (3.2%) had pain even at the end of four weeks and they were continued with prednisolone 20 mg again for next 4 weeks.
Recurrences occur in around 5% - 20% of patients [11,14,15]. Our study showed the recurrence of 7.3 % (n=9). Out of them, 3 patients had recurrence at 2 months, 2 patients at 3 months, 3 patients at 4 months and 1 patient at fifth month. They were all dealt with in the same way as the initial attack and prednisolone treatment was useful for them.
In our study, oral prednisolone at a dose of 20 mg tapered over 4 weeks for treatment of subacute thyroiditis was enough to achieve rapid response of pain relief in 94% of patients within 2 weeks and reduce ESR to normal level in 96% at 4 weeks. There was also significant lower rate of recurrence in comparison to other studies.
Conclusion
As per the result of the study, we recommend that 20 mg of prednisolone daily tapered over 4 weeks is an adequate treatment of subacute thyroiditis. However, dose can be drastically tapered after 2 weeks.