Postoperative pain causes deleterious effects such as alterations in haemodynamic parameters, behavioural and neuroendocrine stress response. Such hormonal and biochemical changes are reflected in rise in blood glucose, cortisol, insulin catecholamines and growth hormone concentrations [1,2]. These responses occur not only in adults but in children as well and modulation of these may favourably influence the ultimate outcome. Drugs such as morphine, ketamine and bupivacaine have been demonstrated to blunt these responses to certain degree by some workers [3–6], as well as in studies done at our institute [7]. A search of literature however, reveals that no comparative study between fentanyl and clonidine for attenuation of these responses when used as caudal adjuvants in children. Since, the choice of techniques and agents used in the perioperative period may influence such responses, a comparison between them is highly desirable. Caudal block is a commonly used simple and safe technique. The quality and duration of analgesia can be improved with use of adjuvants such as ketamine, morphine, fentanyl, midazolam, and clonidine [7]. Clonidine, is a popular adjuvant [8,9] although the optimum dose of clonidine with bupivacaine remains uncertain. It produces analgesia without causing significant respiratory depression, bradycardia or sedation in dosages of 1-2 μg/kg normally used in paediatric patients.
Sevoflurane is preferred inhalational agent for induction of anaesthesia in paediatric patients however, it is associated with non-purposeful restlessness and agitated behaviour commonly termed as emergence agitation. The exact reason behind such a change is unknown and unrelieved pain remains one of the postulated causes [11]. Hence, effective postoperative pain management such as by caudal block with local anaesthetic with or without adjuvants (fentanyl, clonidine) for infraumbilical surgeries may prevent emergence agitation.
Though many workers have established the role of these agents, there is paucity of literature comparing the benefits/efficacy of caudal fentanyl vs. clonidine to blunt the neuroendocrine stress responses, postoperative pain and emergence agitation caused by sevoflurane anaesthesia in a consistent surgical population. Thus, this study was designed with the aim to assess and compare the efficacy of fentanyl vs. clonidine for analgesia, neuroendocrine stress responses and incidence and duration of emergence agitation.
Materials and Methods
After obtaining approval from the ethical committee, the procedure of the study including detailed method of pain assessment, assessment of emergence agitation and blood sampling for stress response measurement was explained to the parents/guardians as well as to the children (who could understand). Informed consent was obtained from the parents of the children included in the study.
Sixty children were included in this prospective, controlled randomized and double blind study which was conducted from April 2009-10. Children having contraindication to caudal block, history of pre-existing neurological or spinal disease, known endocrine or neurological abnormalities or conditions likely to alter stress hormones such as preexisting pain and hypovolaemia were excluded from the study. Randomization was performed en block in a 1:1 ratio according to a computer generated randomization code using SPSS 17.0 (SPSS Inc., Chicago IL, USA) and delivered in sealed, opaque, sequentially numbered envelopes.
Three groups of 20 each, of ages 1-10 years undergoing elective lower abdominal surgeries belonging to ASA grade I and II were randomized to receive caudal block after induction of general anaesthesia as follows:
Bupivacaine 0.25% 1ml/kg + 0.9% normal saline (0.1 ml/kg) (Weight related volume) to ensure that volume of solution injected remains same in all the study groups
Bupivacaine 0.25% 1ml/kg + fentanyl 1μg/kg
Bupivacaine 0.25% 1ml/kg + clonidine 3μg/kg
The drug was prepared by one anaesthetist who gave unlabeled syringes to the anaesthetist performing the block who was blinded to the solution of bupivacaine and adjuvant, thus ensuring double blindness of the study.
To ensure double blind nature of study the drug was prepared by another anaesthetist who gave unlabeled syringes containing bupivacaine and adjuvant to anaesthetist performing the block. It was ensured that the upper limit of dose of Bupivacaine which is 2.5 mg/kg is not exceeded in any of the subjects.
Preoperative assessment was performed and children were fasted according to ASA standards. The children were premedicated with oral midazolam 0.5 mg/kg 30 minutes prior to induction. Inhalational induction was carried out with 6-8% sevoflurane in 100% oxygen using a face mask. An intravenous cannula (22/24 gauge) was then sited and an appropriately sized laryngeal mask airway was placed. The patients were allowed to breathe spontaneously. Anaesthesia was maintained with a mixture of 40% oxygen in nitrous oxide and sevoflurane at a MAC value of 1.5. Intravenous fluid (Ringer Lactate) was given according to Holliday and Segar formula. Caudal block was then performed and the study medication injected according to the group assigned as per the randomization code.
Standard monitoring was established and the parameters were monitored at the time of induction and every five minutes thereafter. At the end of surgery, the child was shifted to post anaesthesia care unit (PACU). One blinded observer recorded all the data in PACU.
To assess the neuroendocrine stress responses, samples were taken from a separate dedicated vein cannulated with a 22/20 gauge intravenous cannula. Approximately 5-6 ml of blood was drawn for measurement of blood glucose, serum cortisol and insulin levels. Blood glucose was measured by glucometer. Serum cortisol levels and serum insulin levels were measured by radioimmunoassay (through commercially available kits) just after induction as baseline value before giving caudal block (T0), 30 min after start of surgery (T30), 60 min after end of surgery (T60).
The modified VAS scale used in this study integrates the subjective assessment by the patient using standard 10 cm line and also observational assessment by using FLACC scale (for children ≤ 5 years) [12]. The scores were assessed by a single blinded observer at all-time intervals postoperatively. The nurses and parents were explained about the pain assessment. Rescue analgesia with paracetamol 20 mg/kg orally or by rectal suppository was given whenever VAS scores were≥ 4.
Assessment for emergence agitation was done at 0 min (arrival in PACU), 15 min, 30 min, 45 min, and 60 min. Emergence agitation was scored as follows: 1 = awake, calm, cooperative; 2 = crying, requires consoling; 3 = irritable/restless, screaming, inconsolable; 4 = combative, disoriented, thrashing. Children with an agitation score of 3 or 4 were classified as agitated.
The sedation in the postoperative period was assessed by a scoring system [13] as follows 1) asleep, arousable by verbal contact, 2) asleep, arousable by physical contact, 3) asleep, not arousable. All children were observed for complications like sedation, respiratory depression, nausea, vomiting, itching, urinary retention, motor weakness, hypotension, and bradycardia.
Statistical Analysis
Considering SD1 = 0.51 and SD2 = 0.72 in the bupivacaine and clonidine groups, to study a difference of 0.65 units in mean values of VAS score at 90% power and alpha value of 5%, a sample size of 20 cases in each group was required. Data was analysed using SPSS version 17 computer software. Numerical variables are presented as mean and standard deviation (SD) and categorical variables as frequency (%). Analysis of variance (ANOVA) for repeated measures was used for analysing the collected data. Tukey’s HSD test was applied as post hoc test whenever applicable. P-value of ≤ 0.05 was taken as significant. The power of one-way ANOVA was found to be 1.00 for detecting the difference in the average time to first analgesic administration.
Results
The children in all the groups were comparable for age and weight, duration and types of surgery [Table/Fig-1].
| Group | I | II | III |
|---|
| Age (years) (mean ± SD) | 5.70 ± 3.19 | 5.75 ± 2.26 | 4.55 ± 2.91 |
| Weight (kgs) (mean ± SD) | 16.60 ± 5.73 | 15.80 ± 5.89 | 14.65 ± 6.07 |
| Surgical duration (mean ± SD) | 43.54 ± 9.43 | 41.40 ± 6.50 | 39.7 ± 7.92 |
| Type of surgeries Herniotomy | 15 | 16 | 17 |
| Circumcision | 4 | 2 | 2 |
| Hypospadiasis | 1 | 2 | 1 |
| Males/ Females | 19/1 | 17/3 | 18/2 |
The VAS score was analysed at 0, 0.5, 1, 2, 4, 6, and 24 hours. As the earliest rescue analgesia was given at ≤ 4 hours (in 12 out of 20 subjects in bupivacaine alone group), statistical comparison between the Groups could be done only upto 4 hours. The mean VAS score in Group I varied between 0.20 ± 0.41 at 0 minutes (i.e. arrival at PACU) to 1.80 ± 0.41 at 2 hours postoperatively. The mean VAS score in Group II ranged between 0.00 ± 0.00 in immediate postoperative period to 1.25 ± 0.44 at 2 hours postoperatively. The same in Group III varied from 0.00 ± 0.00 at 0 minutes to 0.60 ± 0.60 at 2 hours postoperatively. The VAS score among patients in group II and III was significantly less as compared to those in Group I at 4 hour postoperatively. There was, however, no significant difference between group II and group III at these time intervals.
The VAS score at 6 hours was significantly less in Group III as compared to Group II [Table/Fig-2].
Mean VAS scores in all groups at various time intervals
| Postop Time (hrs) | Group I | Group II | Group III |
|---|
| 0 | 0.20 ± 0.41 | 0.00 ± 0.00 | 0.00 ± 0.00 |
| 0.5 | 0.65 ± 0.49 | 0.15 ± 0.36* | 0.00 ± 0.00** |
| 1 | 1.20 ± 0.52 | 0.65 ± 0.59* | 0.30 ± 0.47** |
| 2 | 1.80 ± 0.41 | 1.25 ± 0.44* | 0.60 ± 0.60**,*** |
| 4# | 3.50 | 1.85* | 1.05**, |
| 6# | NA | 2.50 | 1.60*** |
* Significant difference between Group I & II (p-value ≤ 0.05);
** Significant difference between Group I & III (p-value ≤ 0.05);
*** Significant difference between Group II & III (p-value ≤ 0.05);
# Mean VAS score of the remaining patients who had not received rescue analgesia by that time
NA- not applicable as all patients had received rescue analgesia by that time
The proportion of children with adequate surgical analgesia was 40% in Group I and 100% in Group II and III at 4 hours postoperatively. This proportion further fell to 0% and 40% in group I and group II respectively but remained at 100% in group III up-to 6 hours postoperatively.
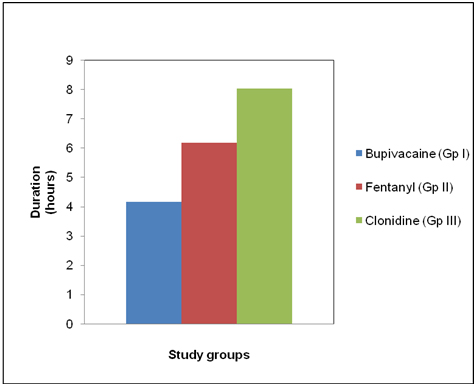
The mean time for requirement of rescue analgesia in group I was 4.15 ± 0.54 hours, 6.18 ± 0.57 hours in Group II and 8.03 ± 0.94 hours in group III [Table/Fig-3]. The difference was statistically significant among the three groups, the earliest need for rescue analgesia being in group I.
The patients in Group III were significantly more sedated than the ones in Group I and II, till two hours postoperatively [Table/Fig-4]. Beyond this time, the sedation scores were not significantly different amongst the three groups All the children in the study groups were wide awake and alert (i.e. sedation score = 0) by 4 hours postoperatively.
Sedation score in all 3 groups at various time intervals
| Postop Time (hrs) | Group I | Group II | Group III |
|---|
| 0 | 1.40 ± 0.5 | 1.70 ± 0.47 | 2.25 ± 0.55**,*** |
| 0.5 | 0.70 ± 0.66 | 1.20 ± 0.52* | 1.80 ± 0.41**,*** |
| 1 | 0.10 ± 0.31 | 0.60 ± 0.50* | 1.10 ± 0.31**,*** |
| 2 | 0.05 ± 0.22 | 0.05 ± 0.22 | 0.70 ± 0.47**,*** |
| 4 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 |
*Significant difference between group I & II(P-value ≤ 0.05);
** Significant difference between group I & II(P-value ≤ 0.05);
*** Significant difference between group II & III(P-value ≤ 0.05)
The EA scores were significantly less in group III as compared to group I at 0 minute and 15 minutes postoperatively. However, there was no significant difference between group III and group II at these times. The EA score at and beyond 30 minutes was comparable among all the groups [Table/Fig-5].
Emergence agitation score in all 3 groups at various time intervals
| Postop Time (min) | Group I | Group II | Group III |
|---|
| 0 | 2.10 ± 0.64 | 1.65 ± 0.59* | 1.35 ± 0.59** |
| 15 | 1.75 ± 0.55 | 1.45 ± 0.51 | 1.35 ± 0.49** |
| 30 | 1.25 ± 0.44 | 1.20 ± 0.41 | 1.10 ± 0.31 |
| 45 | 1.00 ± 0.00 | 1.00 ± 0.00 | 1.00 ± 0.00 |
| 60 | 1.00 ± 0.00 | 1.00 ± 0.00 | 1.00 ± 0.00 |
* Significant difference between group I & II (P-value ≤ 0.05);
** Significant difference between group I & III (P-value ≤ 0.05)
NESR was assessed by measurement of blood glucose, serum cortisol and serum insulin at T0 (baseline), T30 (30 min after surgical incision) and T60 (60 min postoperatively) [Table/Fig-6].
Stress response parameters in all three groups at various time intervals (mean ± sd)
| TIME | Blood glucose (mg/dl) | Serum cortisol (μg/dl) | Serum insulin (μIU/ml) |
|---|
| Group I | Group II | Group III | Group I | Group II | Group III | Group I | Group II | Group III |
|---|
| T 0 | 84.85 ± 7.07 | 84.80 ± 8.60 | 84.75 ± 5.57 | 17.14 ± 12.88 | 16.06 ± 8.96 | 16.54 ± 12.97 | 3.35 ± 3.42 | 2.93 ± 2.36 | 2.89 ± 3.30 |
| T 30 | 92.40 ± 7.97 | 91.50 ± 7.33 | 88.85 ± 5.11 | 15.77 ± 9.13 | 16.42 ± 12.35 | 16.00 ± 13.37 | 6.45 ± 5.93 | 6.45 ± 5.27 | 6.43 ± 7.56 |
| T 60 | 97.35 ± 20.98 | 99.00 ± 9.38 | 94.90 ± 6.00 | 25.98 ± 10.48 | 23.05 ± 15.19 | 15.25 ± 13.20 | 5.12 ± 5.81 | 4.62 ± 5.71 | 4.08 ± 5.33 |
Baseline values of indices were comparable within all the groups. Blood glucose values increased significantly intragroups at T30 and T60, but the increase was not significant intergroups. All the groups showed a significant rise in serum insulin level from baseline to T30. The rise from T0 toT30 was followed by a fall in serum insulin level at T60 in all the three groups. Although the values were lowest in group III at both T30 and T60, this difference was not statistically significant between the groups.
At T30 the level of serum cortisol was not significantly different within or between the three groups. At T60, there was a significant rise in serum cortisol levels from baseline values (T0) in group I and II (bupivacaine and fentanyl group). However, patients in Group III (clonidine group), had a fall in serum cortisol levels from baseline to T60. This difference was, not significant when compared with the other two groups. The trends indicate a nearly constant level of serum cortisol in Group III as against the rising trend in Group I and II. The haemodynamic parameters remained within normal values throughout the study period and these values were comparable in all the three groups. None of the patients had side effects like respiratory depression, PONV, itching, urinary retention or motor weakness.
Discussion
Single shot caudal block provides effective postoperative analgesia. The duration of block can be prolongation use of adjuvant like opioids (fentanyl [10]) and more recently α2-agonist (clonidine). Clonidine in the dosage of 1-2 μg/kg provides prolongation of analgesia but for a limited period. Dose of 5 μg/kg can cause undesirable motor blockade. A dose of 3 μg/kg [11] has been used in a few studies but not adequately investigated for analgesia, neuroendocrine stress response and emergence agitation. Hence, this study was planned with this dose to study these parameters and also to establish the safety of this dose. So, in the present study we used fentanyl and clonidine in the dosage 1 μg/kg and 3 μg/kg respectively.
We used the already well established methods to measure pain i.e. modified VAS scale [12,13] and serum cortisol, blood glucose and serum insulin levels to assess NESR.
Our results indicate that caudal administration of either clonidine or fentanyl, provides good pain relief with very low VAS scores in the immediate postoperative period. But the quality as well as duration of analgesia was best with clonidine followed by fentanyl as compared to only bupivacaine. With bupivacaine alone, VAS scores remained low up to 4 hours postoperatively with most patients receiving rescue analgesia after 4.15 hours. This finding is in agreement to previous studies using similar dosages [6]. The addition of fentanyl to bupivacaine, resulted in significantly low (p<0.05) VAS scores as compared to bupivacaine till 4 hours postoperatively indicating a better and longer duration of analgesia. Rescue analgesia in this group was given at 6.18 hours. Similar findings were reported by Desai et al., [10] with caudal fentanyl.
With clonidine as adjuvant, the duration of adequate analgesia (VAS <3) was highest amongst the three groups and the mean time to rescue analgesia was 8.03±0.94 hours Our results are similar to the findings of a study conducted by Yildiz [9] and Akin et al., [14] who reported mean duration of analgesia as around 8 hours in children undergoing inguinal hernia repair under general anaesthesia using caudal clonidine. Their study design was however different from ours making comparison difficult. Wheeler et al., [15], however, failed to demonstrate any prolonged analgesic benefits of addition of clonidine 2 μg/kg to bupivacaine through caudal route over bupivacaine alone.
Attenuation of NESR by various techniques is a recent area of research interest [16,17], Although many drugs have been extensively reviewed to modulate NESR [16] we did not find any study which included caudal clonidine for the same. This was, therefore, the first study to evaluate the efficacy of caudal clonidine to blunt NESR.
We did not take blood samples preoperatively for hormonal levels because of the effects of preoperative and separation anxiety especially in older children.
Hepatic glycogenolysis, gluconeogenesis and insulin resistance at cellular level per peratively alters normal regulation of glucose homeostasis hence hyperglycemia and increase in insulin levels are inevitable. In present study too, a rise in blood glucose and insulin levels were found to occur in all the study groups although the values were within normal range for that age. Earlier studies comparing caudal block with GA alone group have reported a reduction in the NESR in caudal group, although accompanied with an increase in blood glucose [17,18]. Although we did not have a control group comprising only GA group (without any caudal block), the fact that all blood glucose values were within normal range indicates blunting of NESR in all the groups. This beneficial effect was found to be maximum with clonidine.
Although there was no statistically significant difference between the 3 groups, the modest fall in the serum cortisol values postoperatively in clonidine group as against a rise in fentanyl and bupivacaine groups signify a near equal NESR in the fentanyl and only bupivacaine group. These results are parallel with the findings of Gaitini et al., [18] who showed that there was no beneficial effect of using small doses of fentanyl (1 microgram*kg-1) and bupivacaine 0.25% for caudal epidural-analgesia, compared with bupivacaine 0.25% alone, based on pain scores and catecholamine levels in patients undergoing inguinal herniorrhaphy.
Murat et al., [19] demonstrated that epidural anaesthesia as compared to GA alone reduces the cortisol response in the first 24 hours after lower abdominal or peripheral surgery. This is in agreement with our study where cortisol levels remained at lower values in the postoperative period. Thus, the decrease in stress response to surgery observed after epidural anaesthesia is mainly related to complete blockade of afferent neurogenic impulses from the surgical site. Novak [20] et al., compared intravenous and epidural clonidine, 4 μg/kg for modulation of NESR following thoracic surgeries in adult patients. They suggested that epidural clonidine significantly reduces the stress response. The patient and the study profile of this study however differed from ours and these differences in the study design make comparisons with our study difficult. We did not find any study evaluating the role of caudal clonidine on modulation of the surgical stress response in children. Our findings, however, clearly indicate a modulation of NESR with caudal clonidine.
Emergence agitation following sevoflurane is a common problem in the postoperative period. A number of studies have been found that used clonidine fentanyl and midazolam administered intravenously. However, there is a paucity of literature analysing the effect of caudally administered fentanyl or clonidine on emergence agitation [21].
M Block et al., [11] studied clonidine in a dose of 3 μg/kg by both intravenous and caudal routes and had concluded that clonidine was effective in this dose to prevent emergence agitation independent of the route used. Hence, we decided to study the efficacy of this dose on emergence agitation in our study, also. In a study conducted by Aouad et al., [22] the effect of preoperative caudal analgesia on the incidence and severity of EA was compared to children receiving intravenous fentanyl without a caudal block. Caudal group revealed a significantly low incidence of emergence agitation and pain scores as compared to i.v. fentanyl (1 μg/kg). These results match with our findings stating a decreased agitation following caudal block. A meta-analysis conducted by Dahmani et al., [23] and one by Chengmi Z [24] found that propofol, ketamine, fentanyl, midazolam and clonidine (i.v., intranasal, oral), had a prophylactic effect in preventing EA. In our study, addition of clonidine and fentanyl to caudal bupivacaine both showed a fall in the intensity of emergence agitation, but the children in clonidine group were more calmer compared to the fentanyl group .
In our study, we did not observe any clinically significant side effects. Patients in clonidine group were significantly calmer/ more sedated than those in fentanyl or bupivacaine group. This degree of sedation was not clinically significant enough to refute the utility of clonidine in this dose (i.e.3 μg/kg). Safety profile of still higher doses of clonidine, however, needs to be evaluated.
Limitations
It is difficult to distinguish between sedation and analgesia in the age group included in the study. Since patients were asleep provided they were comfortable (pain free), and they were awake if they were in pain/ required analgesia.
There may be discordance between self reporting and behavioural pain measures in children 3-7 yrs of age after surgery.
The power of the study was calculated for analgesia and a larger study could highlight the difference in stress response. This study can thus be used as a pilot study to indicate a difference in stress response by use of adjutants in caudal block.
This study has a low sample size hence some linitatations could have occurred.
Conclusion
Thus, we can conclude that clonidine in a dose of 3 g/kg as an adjuvant to bupivacaine is better than fentanyl 1 μg/kg for analgesia, blunting of stress response and prevention of emergence agitation. This may reduce patient’s stay in the PACU and facilitate early discharge hence reduce costs.
* Significant difference between Group I & II (p-value ≤ 0.05);
** Significant difference between Group I & III (p-value ≤ 0.05);
*** Significant difference between Group II & III (p-value ≤ 0.05);
# Mean VAS score of the remaining patients who had not received rescue analgesia by that time
NA- not applicable as all patients had received rescue analgesia by that time
*Significant difference between group I & II(P-value ≤ 0.05);
** Significant difference between group I & II(P-value ≤ 0.05);
*** Significant difference between group II & III(P-value ≤ 0.05)
* Significant difference between group I & II (P-value ≤ 0.05);
** Significant difference between group I & III (P-value ≤ 0.05)