The thumb contributes to about 40% of the hand functions. Hence loss of thumb results in significant loss of hand function [1]. The thumb is a vital contributor to the complex mechanism of prehension. Except in the cases with unsuitably amputed thumb, replantation is indicated in all cases [2]. Pollicization, toe to thumb transfer and osteoplastic thumb reconstruction, including free tissue transfer, are the most reported reconstructive procedures after traumatic amputation at the proximal and middle third of the thumb [3].
Osteoplastic reconstruction of the thumb is indicated in amputation at or around metacarpophalangeal level in patients who cannot, or will not, have a toe transfer [4]. In this study we have discussed two techniques of osteoplastic reconstruction; distally based radial forearm osteocutaneous flap and groin flap with iliac crest free bone graft.
Materials and Methods
This study was conducted from August 2012 to December 2014 in the Department of Plastic Surgery in Bangalore tertiary care centre. Total 104 patients with various levels of thumb tissue loss were examined in casualty. Out of these, 36 patients had injury at middle or proximal third of thumb. Replantation was done for 14 patients which was successful in 10 patients. Patients who were unsuitable for thumb replantation and with failed replant were given option of osteoplastic thumb reconstruction. Osteoplastic thumb reconstruction was done for 13 patients and they were included in the study. In thumb amputations with first web space injury and associated injury in forearm, chronic smokers, doubtful Allen’s test; groin flap was preferred over radial forearm flap. Data was collected in terms of age, sex, occupation, handedness and mode of injury, level of thumb amputation, surrounding injury, other co-morbidities and surgical procedure. Postoperative results were assessed in terms of range of motion, hand grip, functional recovery, donor site morbidity and patient satisfaction. Details of the patients are mentioned in [Table/Fig-1].
Patient information for the study
| S. No | Side of hand | Age | Sex | Mode of injury | Level of amputation | Surgery performed |
|---|
| 1 | Right | 48 | Male | Firecracker | At MCP joint | Groin flap + iliac bone graft |
| 2 | Left | 30 | Male | Machine cut injury | Base of proximal phalanx | Groin flap + Iliac bone graft |
| 3 | Right | 27 | Male | Machine cut injury | Base of proximal phalanx | Groin flap + iliac bone graft |
| 4 | Left | 15 | Male | Machine crush injury | Base of proximal phalanx | Groin flap + iliac crest bone graft |
| 5 | Right | 28 | Male | Road traffic accident | Base of proximal phalanx | Groin flap + iliac crest bone graft |
| 6 | Left | 40 | Male | Construction site crush injury | At mid proximal phalanx | Groin flap + iliac crest bone graft |
| 7 | Right | 35 | Male | Machine cut injury | At Head of 1st Metacarpal | Radial forearm osteocutaneous flap |
| 8 | Left | 42 | Male | Road traffic accident | At MCP joint | Radial forearm osteocutaneous flap |
| 9 | Right | 30 | Male | Stone crush injury | At base of proximal phalanx | Radial forearm osteocutaneous flap |
| 10 | Left | 34 | Male | Machine cut injury | At MCP joint level | Radial forearm osteocutaneous flap |
| 11 | Left | 28 | Male | Road traffic accident | At MCP joint | Radial forearm osteocutaneous flap |
| 12 | Right | 32 | Male | Assault | Mid proximal phalanx | Radial forearm osteocutaneous flap |
| 13 | Left | 32 | Male | Stone fall crush injury | At MCP joint level | Radial forearm osteocutaneous flap |
Surgical Procedure
Groin Flap with Iliac Bone Graft [4]
Groin flap is an axial pattern flap based on superficial circumflex iliac artery which runs 2 cm below and parallel to inguinal ligament. According to the defect size [Table/Fig-2], flap was marked and elevated from lateral to medial side, superficial to deep fascia. After crossing lateral border of Sartorius deep fascia was incised and elevated with the flap. Tubing of flap was done. Iliac crest tricortical bone graft was harvested with oscillating saw. Bone graft was fixed to the remaining stump of thumb with screws and plate [Table/Fig-3]. Then groin flap inset was given around the flap [Table/Fig-4]. Donor site was either closed primarily or skin-grafted. In second stage, flap was divided after 3 weeks and final inset was done [Table/Fig-5].
Groin flap with iliac bone graft – amputed thumb

Groin flap with iliac bone graft – bone graft

Groin flap with iliac bone graft – wrapped around flap

Groin flap with iliac bone graft – divided flap

Radial Forearm Distally Based Osteocutaneous Flap [4]
Adequecy of distal circulation based on ulnar artery was checked by Allen’s test. Flap marking was done considering pivot point mid-way between distal end of thumb defect and proximal end of radial forearm flap [Table/Fig-6,7]. On radial side, flap was elevated upto ulnar edge of bracioradialis. On ulnar side, flap was elevated upto radial edge of flexor carpi radialis. Radius periosteum was exposed and around 6 cm of radius anterior cortical graft was included in flap. Before diving proximal end of radial artery, clamp was applied to check for flap and digital circulation. Radial artery was divided proximally and flap was transposed distally to the thumb [Table/Fig-8]. Donor site was skin-grafted. Bone was fixed to the thumb stump with plate and screws. Flat inset was given around the bone graft. Final outcome is shown in [Table/Fig-9].
Radial Forearm Distally Based Osteocutaneous Flap – amputed thumb

Radial Forearm Distally Based Osteocutaneous Flap
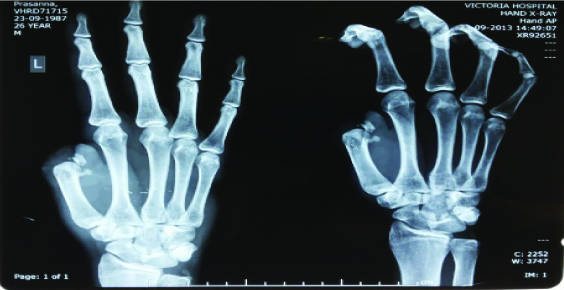
Radial Forearm Distally Based Osteocutaneous Flap – dissection

Radial Forearm Distally Based Osteocutaneous Flap – postoperative

Postoperative Rehabilitation
Regular physiotherapy and splintage was done to get the optimum movement from a reconstructed thumb. The reconstructed thumb and donor forearm are protected with a short-arm thumb Spica cast for 6 weeks. After that, range of motion and opposition exercises is initiated. Any heavy lifting and weight bearing is avoided for 4 more weeks. Training in activities of daily living and vocational training was arranged for most of the patients. Sensory retraining was started in patients in whom Littler flap was done.
Results
In our study majority patients were daily wage workers from construction sites. These patients were presented with crush injury of thumb with amputations and were not fit for replantation. Out of 13 patients 2 were post replant failure with clean cut injury around metacarpophalangeal joint. Site of injury was around first metacarpophalangeal joint for majority of patients. Out of 13 patients only 1 patient was left handed with opposite side thumb injury. Out of 13 patients 7 underwent distally based radial forearm osteocutaneous flap single stage thumb reconstruction. Two stage ipsilateral groin flap with iliac crest bone grafting was done for 6 patients. The average size of flap and graft were observed as mentioned in [Table/Fig-10]. Groin flap division and inset was done after average 26 days. Subsequently debulking of the flap was done for 6 patients, primarily for groin flap reconstruction, approximately 4 months postoperatively. Extensive rehabilitation program was scheduled postoperatively in every case.
| Procedure | Number of patients | Average size | Average Flap division and inset (Days) | Donor site morbidity |
|---|
| Flap (cm2) | Bone graft (cm) |
|---|
| Radial forearm distally Based osteocutaneous flap | 7 | 102 | 6 x1.5 | NA | 2 |
| Groin flap with iliac bone graft | 6 | 148 | 5 x 1.5 | 26 days | 1 |
All reconstructive thumbs were functionally acceptable. Cosmetically, donor site morbidity was an issue for 2 patients with radial forearm flap and 1 patient with groin flap. Suture line dehiscence and plate exposure required intervention in local anaesthesia in one patient with radial forearm flap [Table/Fig-11,12].
Radial Forearm Distally Based Osteocutaneous Flap - Delayed plate exposure

Radial Forearm Distally Based Osteocutaneous Flap - Delayed plate exposure X-Ray

The major drawback for both techniques was absence of sensitivity. Temperature, touch and pain sensation were absent immediately after reconstruction. On late follow up, patients were counselled for neurosensory Littler flap but only two patients opted for this procedure. All patients were followed up for minimum of 6 months and a maximum of 24 months.
Discussion
In a traumatic thumb loss replantation and reconstruction are the available methods. The choice of the method is guided by the level of thumb amputation. Physical examination and radiographs are used for determination of level of loss [4]. Osteoplastic reconstruction of the thumb is indicated in amputation at or around metacarpophalangeal level in patients who cannot, or will not, have a toe transfer [5]. Any of the microsurgical reconstruction with second-toe transfer, great toe transfer, or wraparound technique will give much better result, both functionally and cosmetically [6]. However, in many situations, patients might be reluctant to sacrifice a toe for reconstruction of the thumb. In countries where thong sandals are the main footwear, loss of second or great toe might be viewed as unacceptable deficit [7]. Cultural issues regarding loss of another digit or toe might also play a role in patient’s decision making. Osteoplastic reconstruction, although inferior in cosmetic outcome, does not require sacrifice of another finger or a toe and also does not need microsurgical expertise [8,9].
Both groin flap and radial forearm flap are reliable and versatile flaps. Requirement of multiple-stage surgery, poor sensation and absorption of bone graft were the main hindering factors with groin flap and iliac crest bone graft [10]. With this technique, donor site morbidity and scar was much acceptable to patients when compared with radial forearm flap. Radial forearm osteocutaneous flap was single stage technique with vascularized bone graft. Disadvantages of this flap were donor site graft loss and visible forearm scar. Though we have not seen any donor site fractures, it is a well-known complication of this technique. Both flaps were non sensate flap and needed Littler flap for regaining sensation at tip of reconstructed thumb. Partial flap loss can be disastrous as it lessens the width of flap, length of the thumb, bone graft exposure and loss of the bone graft [9]. Minimal requirement for optimal functional thumb can be achieved with osteoplastic reconstruction techniques as shown in [Table/Fig-13,14 and 15].
Optimal thumb functions – Pulp-to-pulp pinch

Optimal thumb functions – Tripod pinch to enable fine object manipulation
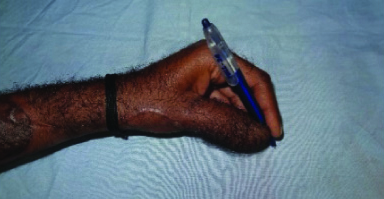
Optimal thumb functions – Hand-digital cylinder grasp for larger objects

Limitations of The Study
The sample size was limited due to access to the patients from a single tertiary care center and due to the time bound nature of the study. The study needs to continue over next few years to include additional patients from the other hospitals and tertiary care centres around the region to draw statistically significant conclusions.
Conclusion
While Toe-to-thumb transplantation is the gold standard, we observed that osteoplastic reconstruction is a very good alternative. If mobility at CMC joint is intact, good opposition and grasp can be achieved with osteoplastic techniques. Most of the patients were manual labourers, hence stability, length, position and strength were most important factors to be achieved. Most of the patient returned back to their previous occupations and were able to use their thumb for earning livelihood. We observed that osteoplastic reconstruction for thumb amputations around metacarpophalangeal joint, when planned meticulously, can result in satisfactory restoration of thumb function.