Background
Children with cerebral palsy, although having similar diagnosis, varies in their abilities & level of functioning within & across different environmental context e.g. home, school or community setting. Capacity (what a child can do in standardized, controlled environment) may or may not be the same as performance (what a child actually does do in her/her daily environment).
Materials and Methods
After getting approval from Institutional Ethic’s Committee (IEC), 63 children with cerebral palsy (4-16 year, mean 7.4 year with SD 0.39) of all clinical types, Gross Motor Functional Classification System (GMFCS) level I-V were examined for mobility using Gross Motor Functional Measure 88 (GMFM). Motor capacity was assessed in clinical setting by highest of 3 GMFM items attained, i.e., crawling (44), walks with support (68) & walks without support (70). Motor performance was measured by Functional Mobility Scale version 2.
Result
On analysis of motor capacity 42.85% children were walking without support, 15.87% were able to crawl & 26.98% were able walk with support in clinical setting. Spearman’s Correlation was done between GMFM item 70 with FMS 5 (home setting) to check correlation of capacity with performance & was found to be significantly correlated (r=0.586, p=0.04). All three GMFM items were correlated with FMS 5, 50, 500 & found positively correlated. For community setting (FMS 500), 52.38% children were lifted by parents & only 6.34% were using wheel chair mobility. A total of 21.87% patients were able to walk with or without support & still lifted by parents in school or community setting.
Conclusion
Change in capacity and performance of mobility exists mainly in school and community setting in studied population. Context should be given importance to prioritize rehabilitation process.
Community, ICF, Motor capacity
Introduction
India is developing country with total population of more than 100 crores. In India, the prevalence of disability is estimated at 35 million individuals, of whom 15 million are children [1].
The cerebral palsy (CP) have been described as “a group of non-progressive, but often changing, motor impairment syndromes secondary to lesions or anomalies of the brain arising in the early stages of development” [2]. CP is the commonest diagnosis of children who receive physical therapy services on regular basis at the institution where present study was conducted.
Mobility is important for the cognitive and psychosocial development of children [3,4]. Independent mobility is vital for activity & participation, reducing dependence on caregivers and the environment [3–5]. Children with significant mobility impairments who cannot crawl and walk independently are at risk for additional secondary, mobility-related delays [6].
The severity of limitation in gross motor functions among children with CP is highly variable. Children with cerebral palsy although having similar diagnosis, varies in their abilities & level of functioning within & across different environmental context e.g., home, school or community setting. According to International Classification of Functioning, Disability and Health [7], the environment is defined as the physical, social and attitudinal conditions that are present in an individual’s life.
In 2006, ICF-CY was developed to include developmental aspects of children & youth which were similar to adult ICF [8]. Capacity & performance are domains of ICF-CY. “Capacity” (what a child can do in standardized, controlled environment/what they can do at their best) may or may not be the same as “Performance” (what a child actually does do in her/her daily environment/the execution of that activity in the real world) [7,9,10].
Recent research has examined differences in mobility of children with CP across environmental settings [11–13]. There is scarcity of similar research in Indian population & result of foreign studies may not be applicable in Indian context. The socio economical differences, cultural differences & availability of assistive technology as well as Government funding vary between developed countries and developing countries as well as among different states of India.
So the aim of present research is to report whether any differences in mobility of children with CP exist across different environmental settings in Ahmedabad, Gujarat, India.
Present study is one of the objectives of a larger research project being conducted at our institution where analysis of various mobility issues in children with CP is being explored.
Research Question: Do capacity & performance of mobility differ in terms of environmental settings in children with CP?
Materials and Methods
Design: An Exploratory Study.
Participant inclusion criteria: Children with diagnosed cases of CP, all clinical types, all GMFCS level, age range 4-16 year
Exclusion criteria: Children with impaired mobility due to other Neuro Developmental Disability like Meningo Myelocele, Autism, Duchenne Muscular Dystrophy etc; children with CP aging< 4 years or > 16 years; CP with uncontrolled epilepsy & impaired cognition, patients who had gone through L/E surgery or botulinum toxin within 6 month of study entry.
Outcome Measures
Mobility (Activity & participation domain of ICF) – Capacity is measured as highest of 3 items from GMFM 88 under structured environment with routine orthosis & assistive devices (Item 44 – crawling, Item 68 – walk with support, Item 70 – walk without support) [14] GMFM is standardized test designed to measure change in GM function in CP [15].
Performance is measured with Functional Mobility Scale (version 2) which rate what the child actually does at this point in time & not what they can do or used to be able to do. Questions asked to parent (not direct observation) about usual mobility method e.g., How does your child move around for short distances in the house? (5m), in and between classes at school? (50 m), long distances such as at the shopping center? (500 m) FMS is reliable, valid & sensitive tool with substantial agreement between direct observation & parental report [16].
Difference in administration between these two outcome measure was not kept >1 week to avoid major change in mobility method.
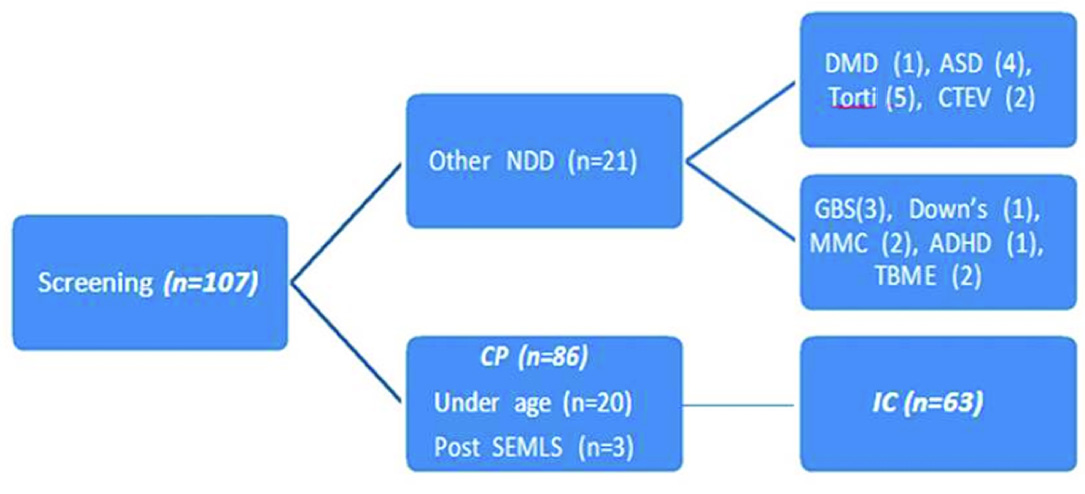
Procedure: After approval from IEC, screening of patients coming to paediatric rehabilitation center of SBB college of Physiotherapy from various OPDs of VSGH & Aastha paediatric rehabilitation center were done (n=107). Children were selected as per selection criteria & informed written consent was taken from parent or legal caregiver along with oral consent from child who is verbal. Capacity was measured using GMFM 88 by therapist under structured environment at clinical setting with routine orthosis & assistive device & Performance was measured using FMS where parents were questioned for functional mobility used by child for various distances (5 meter-home, 50 meter- school and 500 meters-community).
Flow chart of participant through study [Table/Fig-1]:
Flow chart of participants through study
Statistical Analysis
Statistical analysis was done using SPSS 16.0 version with level of significance kept at 5%. Correlation between GMFM item 44,68 and 70 (Motor capacity) with FMS 5,50 and 500 (motor performance) was done using Spearman’s correlation test.
Results
For analysis children were grouped as per their mobility levels. Group A- children unable to crawl (n=15), Group B- children capable of crawling (n=4), Group C- children capable of walking with support (n = 17), Group D- children capable of walking alone (n=27).
Children who step with wall support/furniture support/ adult are hand support/ walks using a walking aid were all categorized under walk with support for analysis [14]. Mean age of patients was 7.4 year SD 0.39 (range 4 to 16). Total male patients were 44 (69.8%) while female were 19 (30.15%). Demographic features of studied population was shown in [Table/Fig-2,3].
Clinical types of children with Cerebral Palsy
| Clinical type | | No | Percentage |
|---|
| Spastic | Diplegic | 21 | 33.33% |
| Quadriplegic | 14 | 22.22% |
| Triplegic | 5 | 7.93% |
| Hemiplegic | 10 | 15.87% |
| Dystonic | | 8 | 12.69% |
| Ataxic | | 4 | 6.34% |
| Athetoid | | 1 | 1.58% |
Locomotor Ability of studied Population as per GMGCS levels
| GMFCS levels | No. | Percentage |
|---|
| I | 19 | 30.15% |
| II | 8 | 12.7% |
| III | 10 | 15.8% |
| IV | 13 | 20.6% |
| V | 13 | 20.6% |
[Table/Fig-4] shows that n= 17 (26.98%) were able to walk with support (GMFM 68), were more positively correlated with home & school setting (r= 0.455, r= 0.575) as compared to community setting (r = 0.387).
Number of patients as per their gross motor capacity in different environmental settings (FMS 5, 50, 500)
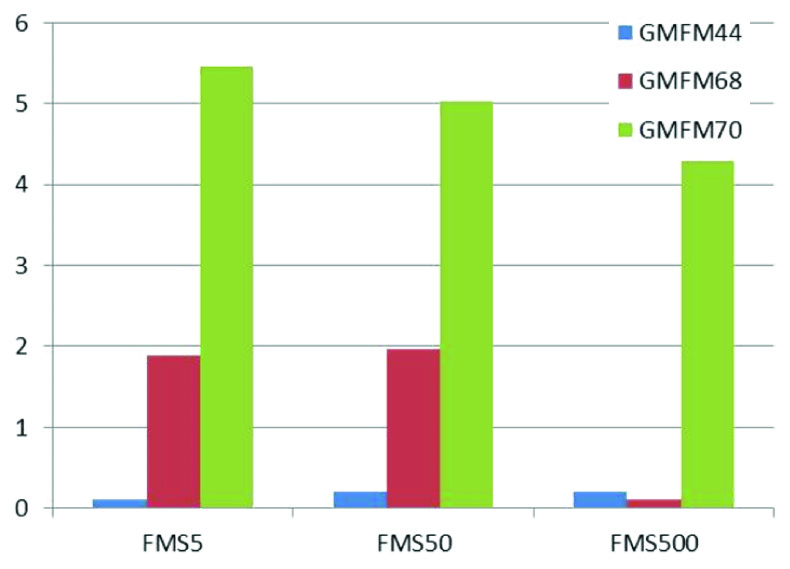
n= 27 (42.86%) were able to walk independently (GMFM 70), were significant & positively correlated in each environmental setting but with decreasing in number in community setting [Table/Fig-4].
Significant positive correlation was found for community setting with GMFM 70 with p=0.008 as compared to GMFM 68 (p=0.125) & GMFM 44 (p=0.118) which suggest that children who are actually walking independently (motor capacity) are only walking in community setting (motor performance).
Discussion
Aim of the present study was to report whether there are changes in capacity & performance in mobility methods in different environmental settings like home, school and community in children with CP. Result of the present study demonstrates that, differences in capacity & performance existing mainly in school & community setting.
On analysis of GMFM 44, Out of 19, total 15 patients were unable to crawl independently. They were either initiating crawling or any other form of floor mobility which may not be exactly used for transition from one place to another & were lifted by their parents to be transited from one room to other, while other 4 patients were able to crawl independently at clinical setting. Out of 4, 3 were performing crawling at home but in spite of having capacity to crawl, 1 patient was not crawling at home. All patients in this category were having clinical diagnosis of spastic quadriplegic CP or dystonic CP & were having GMFCS level IV & V.
None of these patients were put in school for the reason of not having good trunk control, floor mobility or bladder bowel control. Under Government’s project of “SarvaShikshaAbhiyan” special educator allotted to respected area were visiting & advising children for education.
Out of 63, n= 17 (26.98%) were able to walk with support (GMFM 68), were more positively correlated with home & school setting (r= 0.455, r= 0.575) as compared to community setting (r = 0.387). These patients were less preferably using orthosis while walking at home & floor mobility was found faster than supported walking. They used combination of floor mobility & supported mobility at home while they preferred supported walking at school. Social acceptance, peer group demands, motivation of child in school setting might be the factors for preference of supported walking over floor mobility at school compared to home setting.
n= 27 (42.86%) were able to walk independently (GMFM 70), were significant & positively correlated in each environmental setting but with decreasing in number in community setting [Table/Fig-4]. All patients in this category were having clinical diagnosis of either hemiplegic CP or diplegic CP & were having GMFCS level I & II.
In Children walking with or without support (GMFM 68 & 70), total n=7 (11.11%) patients were being lifted by their parents in community. Factors like lack of time, safety issues, high energy consumption by child, various contextual features like surfaces, distances could contribute to dependent mobility [17].
Score 1 of FMS represents child’s use of wheelchair where he may stand for transfers, may do some stepping supported by another person or using a walker/frame [18]. None of the patient studied in the present study used wheelchair for functional mobility in either home, school or community settings.
Out of total 63 patients only 4 (6.34%) patient were using wheelchair in community setting which was pushed by adult. Lack of availability of powered wheelchair was noted. n=33 (52.38%) patients were lifted by their parents in community setting for long time & long distance which can put these parents or caregivers at high risk of musculoskeletal problems.
Sharan D et al., supports prevalence of musculoskeletal problems in caregiver of children with CP [19]. In the studied population, 60% patients were given wheelchair by NGO but they were not using it as it was difficult to bring in all setting, was heavy & very few patients were having four-wheeler.
Tieman B et al., studied changes in mobility of children with CP overtime and across environmental settings in 62 children aged 6-14 years with GMFCS level II-IV & found that mobility methods changes from the methods requiring more gross motor control to methods requiring less gross motor control overtime. Changes within child & within environment are hypothesized to impact changes in mobility methods [20].
Present study is cross-sectional study where changes in mobility methods were reported at one point of time in different environmental settings.
In school setting combination of mobility methods were used by children. Most of children were being lifted by parent or supported by parent by one finger to get entry in school from main gate to classroom. For classroom mobility & classroom to wash area children were using supported walking as mobility method. > 70% of patients in spite of having GMFCS level I or II were not holding their bags on their own & were picked up from school 10 minutes earlier or later in order to prevent fall.
Limitation
Limitation of present study, first, functional mobility was rated using FMS which provides only the child’s most frequently used mobility method. Some children may use several methods of mobility at different environmental settings. Secondly, mobility method was noted cross-sectionally so change in mobility method overtime in an individual child could not be commented. Third, patients with GMFM 44 (crawling) were very less in number to be commented on usual mobility methods.
Conclusion
With present study it can be concluded that a huge paradigm shift is needed in Indian caretakers for perception of community mobility of children with CP. Clinical implication of present study is that examination of motor performance along with motor capacity should be emphasized by therapist & contextual factors should also be considered. Future study with large sample size & with equal no. of subject in each mobility category should be done to get more generalization of result.
[1]. Coleridge P, Disability, Liberation and Development 1993 OxfordOxfam Publications [Google Scholar]
[2]. Rosenbaum P, Cerebral Palsy: What parents and doctors want to know?Available at http://bmj.com/cgi/content/full/326/7396/970?eaf,2003 [Google Scholar]
[3]. Teft D, Guerette P, Furumasu J, Cognitive predictors of young children’s readiness for powered mobilityDev Med Child Neurol 1999 41(10):665-70. [Google Scholar]
[4]. Fernandes T, Independent mobility for children with disabilitiesInternational Journal of Therapy and Rehabilitation 2006 13(7):329-33. [Google Scholar]
[5]. Palisano RJ, Tieman BL, Walter SD, Bartlett DJ, Rosenbaum PL, Russell D, Hanna SE, Effect of environmental setting on mobility methods of children with cerebral palsyDev Med Child Neurol 2003 45(2):113-20. [Google Scholar]
[6]. Larkin D, Summers J, Implications of Movement Difficulties for Social Interaction, Physical Activity, Play and Sports. In: Dewey, D.; Tupper DE., editorsDevelopmental motor disorders: A neuropsychological perspective 2004 Guilford Press:443-60. [Google Scholar]
[7]. World Health Organization: International Classification of Functioning, Disability and Health (ICF). Geneva, Switzerland, World Health Organization, 2001 [Google Scholar]
[8]. Donald J. Lollar, Ed.D. Centers for Disease Control & Prevention, National Center on Birth Defects & Developmental Disabilities, Atlanta, Georgia USA. 2006 [Google Scholar]
[9]. Holdbeeke L, Ketelaar M, Schoemaker MM, Gorter JW, Capacity, Capability and Performance: Different constructs or three of a kind?Arch Phys Med Rehabil 2009 90:849-55. [Google Scholar]
[10]. Tieman B. Usual mobility methods of children with cerebral palsy: A comparison across home, school and outdoors/ community settings. Unpublished doctoral thesis, Hahnemann University, 2002 [Google Scholar]
[11]. Palisano RJ, Tieman BL, Walter SD, Effect of environmental setting on mobility methods of children with cerebral palsyDev Med Child Neurol 2003 45:113-20. [Google Scholar]
[12]. Berry ET, McLaurin SE, Sparling JW, Parent/caregiver perspectives on the use of power wheelchairsPaediatric Physical Therapy 1996 8:146-50. [Google Scholar]
[13]. Haley SM, Coster WJ, Binda-Sundberg K, Measuring physical disablement: the contextual challengePhysTher 1994 74:443-51. [Google Scholar]
[14]. Tieman BL, Palisano RJ, Gracely EJ, Gross motor capability and performance of mobility in children with cerebral palsy: A comparison across home, school and outdoors/community settingsPhys Ther 2004 84:419-29. [Google Scholar]
[15]. Bjornson KF, Graubert CS, validity of GMFMPaediatric Physical Therapy 1998 10:43-47. [Google Scholar]
[16]. Harvey A, Bajer R, Morris ME, Does parent report measure performance? A study of the construct validity of Functional Mobility ScaleDev Med Child Neurol 2010 52:181-85. [Google Scholar]
[17]. Bousquet ER, Hagglund G, Better walking performance in older children with cerebral palsyClin Orthop Relat Res 2012 470(5):1286-93. [Google Scholar]
[18]. The Functional Mobility Scale (version 2) developed by Huge Williamson Gait Laboratory, The Royal Children’s Hospital, Melbourne, Australia. Part of the Gait CCRE [Google Scholar]
[19]. Sharan D, Ajeesh PS, Rameshkumar R, Manjula M, Musculoskeletal disorders in caregiver of children with cerebral palsy following a multilevel surgeryWork 2012 41:1891-95. [Google Scholar]
[20]. Tieman B, Pallisano RJ, Gracely EJ, Rosenbaum P, Chairello LA, O’Neil M, Changes in mobility of children with cerebral palsy overtime & across environmental settingsPhys Occup Ther Paediatr 2004 24(1-2):109-28. [Google Scholar]