Pneumonia is the main cause of death among children under five years of age particularly in developing countries. According to the WHO, there are more than 15 million cases representing 7-13% of annual pneumonia cases which necessitate hospital admission due to their severity [1]. In order to minimize the burden of severe pneumonia, efforts aiming to identify the causative agents are mandatory. Blood, sputum, fluids or tissue samples from the lungs for culture are usually useful, however not promising in young children due to difficulty or inadequacy in collection of samples, as well as transportation difficulties or lack of technical facilities in developing countries [2,3]. Beside chest radiography [4], other means including acute phase reactants, total and differential white blood count and ESR provide support for the diagnosis and management of bacterial infection thus minimizing the burden of the disease by decreasing the hospital stay and decreasing mortality [5–10]. In the absence of definitive aetiology, rapid tools for detecting an inflammatory marker such as C-reactive protein are considered useful to anticipate the possible bacterial aetiology before culture is available, to save time and to lessen hospital stay [11]. The aim of this study was to determine if fever as a clinical variable, total white blood cells count (WBC), C-reactive protein (C-RP) and chest radiography as laboratory variables can anticipate a positive blood culture for cases of clinically severe pneumonia.
Materials and Methods
This hospital-based study was conducted from January 2011 to June 2012, in the Children Emergency Hospital in Khartoum, Sudan, which is a tertiary teaching hospital with a capacity of 150 beds.
All children under five years of age who satisfied the WHO criteria of clinical severe pneumonia were included in the study [12–17]. Consent was obtained from the parents or the child guardian. Children with proven HIV/AIDS, severe malnutrition, tuberculosis, bronchial asthma or with refusal of the guardians were excluded from the study. We recorded demographic data, medical history, vital signs and physical examination results. Blood samples were collected for complete blood count (CBC), C-reactive protein (C-RP) and blood culture using (chocolate blood agar, blood agar, nutrient agar, H and F factors, very special media and tissue media). Colony morphology, alpha hemolytic on blood agar, catalase negative, optochin susceptibility and bile solubility and V factors are used. A chest X-ray was also done for all cases, which was interpreted by a senior radiologist.
A total of 189 children under five years of age satisfied the inclusion criteria. Six variables were used in the analysis after categorizing them into dichotomous variables, namely: culture positive or negative; Age => 36 months or < 36 months; Temperature => 40 0C or < 400C; WBC => 20 000 or < 20 000; C-RP very high (≥ 8mg/l) or normal to moderately high (≤7.9mg/l), and chest radiograph positive or negative for pneumonia.
Statistical Analysis
The IBM Statistical Package for Social Sciences (SPSS 21) [18] was used for data entry and analysis. Two by Two tables were constructed and Odds Ratios, Mantel and Haenszel Chi [19] and 95% confidence intervals (95% CI) were computed using a hand held calculator to estimate the magnitude and statistical significance of the association between each of the variables and culture positivity. All variables were then included in a multi-variable logistic regression model to assess the best predictors of a positive blood culture. The 95% confidence interval was used to test for significance.
Results
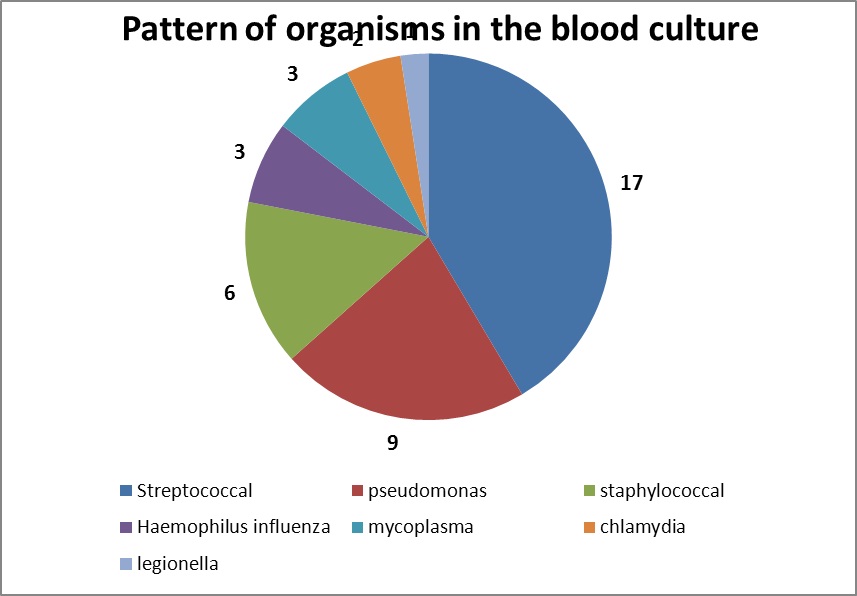
The total number of children who satisfied the inclusion criteria was 189. Out of them, 102 (54%) were females and 87(46%) were males. A temperature of > 40°C was recorded in 80 (42%) of the studied group. Forty-one of the 189 blood samples yielded positive results for bacterial growth, thus, the prevalence of culture positivity was 21.7%. A total white cell count (WBC) ≥ 20000 cell/L was recorded in 65 (34%) and very high C-RP was found in 70 (37%) of the blood samples. Chest X-Ray findings of pneumonia were recognized in 99 (52%) of the study group [Table/Fig-1]. The culture yeilded 17 (41.5%) streptococci, 9 (22%) Pseudomonas, and 6 (14.6%) staphylococci. The remaining 9 (22%) included Haemophilus influenzae, Mycoplasma, Chlamydia and Legionella in small numbers [Table/Fig-2].
Descriptive Statistics, 189 children with Clinically Severe Pneumonia (CSP)
| Variable | N (%) |
|---|
| Gender | Girls | 102 (54) |
| Boys | 87 (46) |
| Age | < 36 months | 141 (75) |
| =>36months | 48 (25) |
| WBC | <20 X109/l | 124 (66) |
| =>20 X109/l | 65 (34) |
| C-RP | very high | 119 (63) |
| Normal to Moderate | 70 (37) |
| Temperature | < 40°C | 109 (58) |
| => 40°C | 80 (42) |
| C X-ray | Negative | 90 (48) |
| Positive | 99 (52) |
| Culture | Negative | 148 (78.3) |
| Positive | 41 (21.7) |
Pattern of organisms in the blood culture
The unadjusted association of the six variables with culture positivity is shown in [Table/Fig-3]. Gender and chest X-ray were not significantly associated with positive blood culture (OR 1.3, 95% CI 0.6-2.6 and OR 1.6, 95% CI 0.8-3.2 respectively). Age (OR 2.7, CI 1.3-5.6), WBC (OR 8.8, CI 4.0-19.4), C-RP (OR 8.7, CI 3.9-19.3) and Temperature (OR 7.4, CI 3.3-16.7) were all significantly associated with a positive culture. However, when all variables were included in a multivariate logistic regression model [Table/Fig-4], the adjusted odds ratios were only significant for WBC ≥20000 cell/L (OR 3.9, 95% CI 1.4-10.9) and temperature ≥40°C (OR 3.1 95% CI 1.2-8.4). The adjusted OR was marginally significant for age (OR 2.4, 95% CI 0.9-5.9, p=0.063).
Unadjusted association of variables with culture positivity
| Culture |
|---|
| +ve | -ve | OR | 95% CI | p-value |
|---|
| Age | ≥36 m | 17 | 31 | 2.7 | 1.3-5.6 | <0.01 |
| <36 m | 24 | 117 |
| Sex | Female | 24 | 78 | 1.3 | 0.6-2.6 | NS |
| Male | 17 | 70 |
| WBC | >20 X109/l | 30 | 35 | 8.8 | 4.0-19.4 | <0.001 |
| ≤20 X109/l | 11 | 113 |
| C-RP | Very high | 31 | 39 | 8.7 | 3.9-19.3 | <0.001 |
| Mod-high | 10 | 109 |
| Temperature | >40 °C | 32 | 48 | 7.4 | 3.3-16.7 | <0.001 |
| ≤40 °C | 9 | 100 |
| C X-ray | +ve | 25 | 74 | 1.6 | 0.8-3.2 | NS |
| -ve | 16 | 74 |
Multiple logistic regression showing adjusted or (95% ci) showing association with culture positivity outcome
| Variable | (Ref. group) | OR (95% CI) | p-value |
|---|
| Age | ≥36 m (<36 =1) | 2.4 (0.9-5.9) | 0.063 |
| Sex | Female (Male =1) | 1.7 (0.7-4.1) | 0.238 NS |
| WBC | >20,000 (≤20,000 =1) | 3.9 (1.4-10.9) | 0.009 |
| C-RP | Very high (Mod-High =1) | 2.2 (0.7-2.2) | 0.168 NS |
| Temp. | >40 °C (≤40 °C =1) | 3.1 (1.2-8.4) | 0.021 |
| C X-ray | +ve (-ve =1) | 1.5 (0.6-3.6) | 0.342 NS |
Additional analysis was attempted to assess the validity of certain clinical findings to predict culture positivity, which is considered the gold standard for diagnosis of pneumonia in this study. Sensitivity, specificity, positive and negative predictive values and their 95% confidence intervals were calculated for each of the six variables [Table/Fig-5]. The best performing variables were WBC, C-RP and temperature with a sensitivity of 73.2%, 75.6% and 78.1 and a specificity of 76.4%, 73.3% and 67.7% respectively. The same variables were the best predictors of a positive culture. The positive predictive values were 46.1% (95% CI 37.8-54.7) for WBC, 44.3% (95% CI 36.6-52.3) for C-RP and 40.0% (95%CI 33.4-47.0) for temperature. The negative predictive value was between 91.1% and 91.7% for all of the three variables with negligible difference between the three.
Variables for prediction of culture positivity
| Variable | Sensitivity (95% CI) | Specificity % (95% CI) | Positive Predictive Value % (95% CI) | Negative Predictive Value % |
|---|
| Age | 41.5% | 79.1% | 35.4% | 83.0% |
| (27.2-56.9) | (71.9-85.0) | (25.4-47.0) |
| Sex | 58.5% | 47.3% | 23.5% | 80.5% |
| (43.1-72.8) | (39.3-55.4) | (18.6-29.3) |
| WBC | 73.2% | 76.4% | 46.1% | 91.1% |
| (58.2-85.0) | (69.0-82.7) | (37.8-54.7) |
| C-RP | 75.6% | 73.3% | 44.3% | 91.6% |
| (60.8-86.9) | (66.1-80.9) | (36.6-52.3) |
| Temperature | 78.1% | 67.7% | 40.0% | 91.7% |
| (63.5-88.7) | (59.7-74.7) | (33.4-47.0) |
| C X-ray | 61.0% | 50.0% | 25.3% | 82.2% |
| (45.5-74.9) | (42.0-58.0) | (20.1-31.2) |
Discussion
To the best of our knowledge this is the first and the only one study addressing predictive factors (clinical or laboratory) of pneumonia in Sudan. In the present study, a high temperature >40°C and an elevated white cell count ≥20000 cell/L were significantly associated with positive blood culture whereas age, gender, elevated C-RP level and chest radiography were not. Sensitivity, specificity, the positive and negative predictive values for prediction of culture positivity was best with high WBC, high C-RP and elevated temperature among children with clinically severe pneumonia.
Few studies had tried to find association with culture positivity with such number of variables. Moreover, the relatively large sample allowed for better statistical results and more stable estimates of significance. However, this study was limited by the low positivity rate of the blood culture in African settings (Schwartz et al.,) [20].
Chest radiograph, in this study, was not a good predictor of culture positivity and hence severe pneumonia. This is in agreement with Hopstaken et al., who observed that chest radiography was an imperfect gold standard for recognition of pneumonia [21]. C-RP association with culture positivity and its predictive value for pneumonia was fairly high in this study. More or less similar results were reported by Koster et al., where not only C-RP but also WBC was found to have a high positive predictive value [22]. However, a lower positive prediction was reported in Mozabique [23]. Koster et al., estimated a positive predictive value for C-RP higher than ours but they reported lower values for the negative predictive value [22]. The predictive values for C-RP, WBC and temperature in our study deserve special attention. They indicate that if these variables are not very high, then the probability that the culture will turn negative, is more than 90% and resorting to culture may well be a wasting of the scarce resources
Temperature of ≥40° C was a significant predictor of a positive culture in this study (Adjusted OR= 3.1, 95% CI 1.2-8.4). A lower similar value {OR=2.2; 95% CI 1.4-3.5) was reported by Michelow et al., [24], however, their sample included all lower respiratory tract infection and their complications as well (i.e. pleural effusion). The age and gender were not significantly associated with a positive blood culture in this study which is consistent with Samir et al., [25].
Our finding suggests that the C-RP is usually high in cases of severe bacterial infection in agreement with a study done previously in Malawi by Diez-Padrisa et al., and by Carrol et al., [26,27]. Markers to predict bacterial infection are highly needed to be employed in many purposes such as the WHO screening program for bacterial vaccine studies, suggested by Madhil et al., and Cheung et al., [28,29]. The data and results in this paper support this hypothesis. Fever and leukocytosis were recommended by Gary in adult patients with severe bacterial infection as a real indication for blood culture which is consistent with this study [30].
Limitations
Such a study usually needs large numbers, utilizing multi-centers and appropriate processing of blood culture in developing countries in general and in Africa in particular. Misuse and non-rational use of antibiotics at reach of patient at any time still hamper the culture results. Inclusion of the children who received prior antibiotics is expected to result in some random misclassification which would only reduce the magnitude of the association. This study would have had an added value if the predictors were used as continuous variables, rather than dichotomous categories to identify a more ideal cut-off point for the temperature, the WBC and the C-RP. Perhaps a lower cut-off point should be used for these variables for screening and prediction of a negative culture. The broad variations in findings from different studies necessitate further research.
Conclusion
This study showed that a temperature of ≥40° C, a WBC of ≥20000 and a high C-reactive protein (C-RP) are significant predictors of a positive blood culture of clinically severe pneumonia. This finding will necessitate admission and empirical treatment without undue waiting for radiology and blood culture reports. The results indicate the independent association of these variables with a positive blood culture result. However, the predictive value of their co-existence was not assessed. On the other hand, chest radiography showed a lower diagnostic value. Nevertheless, urgent empirical treatment for cases of severe pneumonia regardless of eligibility for doing blood culture cannot be over emphasized. More over a search for other tools for accurate investigations should be considered such as PCR.