Diabetes mellitus (DM) is a common endocrine disorder affecting around 387 million people worldwide [1]. The Indian Council of Medical Research-Indian Diabetes Study (ICMR-INDIAB), a national DM study, estimates that currently India has 62.4 million people with DM [2]. The majority (>90%) of them have Type 2 DM (T2DM). A number of studies have reported a high prevalence of pre-clinical diastolic dysfunction among subjects with DM [3]. Diabetes mellitus is one of the major risk factors for diastolic heart failure (DHF). The mortality rates among the patients with DHF ranges from 5-8% annually as compared with 10-15% among patients with systolic heart failure [4]. The evidence suggests that myocardial damage in diabetic patients affects diastolic function before the systolic function. The pathogenesis of this left ventricular (LV) dysfunction in diabetic patients is not clearly understood. It has been proposed that diabetic cardiomyopathy is an independent cardiovascular disease and many underlying mechanisms, such as microvascular disease, autonomic dysfunction, metabolic disorders, and interstitial fibrosis, have been suggested as aetiological factors [5]. Left ventricular diastolic dysfunction (LVDD) represents the first stage of diabetic cardiomyopathy preceding changes in systolic function, reinforcing the importance of early evaluation of ventricular function in individuals with diabetes [6,7]. The diastolic abnormalities are present in diabetic patients in absence of diabetic complications of cardiovascular system [8–10]. So far, very few population-based studies have been carried out in India, to demonstrate the prevalence of DD in newly diagnosed diabetic patients. The relationship between DD and glycemic control is still a matter of debate. Thus, this cross-sectional study was conducted with the aim of determining the incidence of asymptomatic LV diastolic dysfunction in newly diagnosed normotensive cases of type 2 DM subjects and its relation to HbA1C, age at the time of diagnosis, BMI and serum total cholesterol.
To study, the incidence of LVDD in normotensive, newly diagnosed type 2 DM patients by using 2D echocardiography and finding out its correlation with HbA1C.
Materials and Methods
This cross-sectional study was conducted in SVBP Hospital, LLRM Medical College, Meerut, U.P. India over a period of one year between 2013 to 2014. The study comprised a total of 100 cases of newly diagnosed (within 1 month) type 2 DM between the age of 30 and 60 years including both males and females who clinically had no symptoms of cardiovascular involvement and blood pressure <130/80 mmHg, with normal ECG. The diagnosis of diabetes was made on the basis of clinical evaluation, biochemical and ancillary investigation like fasting plasma glucose (FPG)/postprandial plasma glucose (PPPG) and HbA1C according to recent American Diabetic Association (ADA) recommendations. A detailed clinical history with specific reference to cardiovascular symptoms, drug intake and smoking was taken. A complete general and systemic examination particularly for stigmata of cardio vascular status was carried out. All patients with already diagnosed type 2 DM and taking antidiabetic treatment, cardiac diseases like valvular heart disease, ischemic and hypertensive heart disease, congestive heart failure, cardiomyopathy, renal failure, chronic pulmonary disease, severe anaemia and haemoglobinopathies were excluded from the study. Patients underwent thorough clinical examination supported by relevant investigations like blood glucose on admission, FPG/PPPG, renal function tests including electrolytes, fasting lipid profile (FLP), ECG, routine urine and microscopy study, fundoscopy, chest radiography. HbA1C was estimated by Boronate affinity chromatography, which separates total glycosylated haemoglobin by binding to solid–phase dihydroxyborate13 using Nycocard immunoassay kit (USA). Echocardiography was done by # Sonos 4500, EAGFLENE, # Sonos 7500 – Philips. Diastolic dysfunction was evaluated by pulsed doppler echocardiography according to recommendations of the American Society of Echocardiography. Pulsed-wave Doppler (PWD)-derived transmitral inflow velocities was obtained in the apical 4-chamber view, with the sample volume placed at the mitral valve leaflet tips. Measurements included the transmitral early diastolic rapid filling (E-wave) and atrial contraction late filling (A-wave) velocities to calculate E/A ratio, isovolumteric relaxation time (IVRT) and deceleration time (DT).
For tissue Doppler imaging (TDI), the mitral annulus velocity was obtained with a 2 mm sample volume lateral side and septal side of the mitral annulus. Diastolic dysfunction was labeled according to the standard guidelines. Left ventricular overall ejection fraction (systolic function) was calculated by modified Simpson’s method; and left ventricular ejection fraction (LVEF) ≥ 50% was considered as normal. All echocardiographic measurements were averaged over three consecutive cardiac cycles, measured by a single investigator blinded to all other variables. Left Ventricular diastolic dysfunction was considered to be present if any of the following findings were seen, as previously described:
E/A ratio < 1 or > 2
DT < 150 or > 220 ms,
IVRT < 60 or > 100 ms, or
E/E’ ratio > 15 {ratio of mitral peak velocity of early filling (E) to early diastolic mitral annular velocity (E’)}
Classification of LVDD
Grade 1: Delayed relaxation time i.e. E/A <1
Grade 2: Pseudonormalisation
Grade 3: Reversible restrictive pattern
Grade 4: Irreversible restrictive pattern
Statistical Analysis
Statistical analysis was done by estimating the prevalence rate of diastolic dysfunction and correlating with the variables like age, sex, HbA1C etc. Data were analysed for mean, percentage, standard deviation, Student t-test and Fisher’s exact-test, by using SPSS-16(Statistical Package for the Social Sciences) for Windows (SPSS, Chicago, IL). The t-test and Fisher’s exact-test were applied to study quantitative and qualitative data, respectively. A p-value > 0.05 was considered statistically significant.
Observations and Results
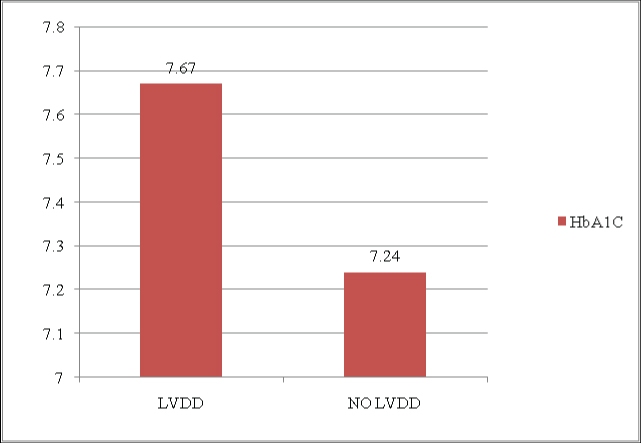
Our study consists of 100 newly diagnosed (within 1 month), normotensive diabetic patients comprising 65(65%) males and 35(35%) females. All studied patients were of age between 30-60 years. Most of the subjects were between 50-60 years of age [Table/Fig-1]. Mean age of the population was 50.08 ± 6.32 years. Mean age of male population was 50.70 ± 5.73 years and that of female population was 48.91±6.99 years. Diastolic dysfunction was present in 41 (41%) of the cases among them 31 were males, 10 were females [Table/Fig-2]. Diastolic dysfunction was prevalent in 10% of patients in age group of 30 -39 years, 24% of patients with age group 40-49 years. Among the age group of 50-60 years diastolic dysfunction was most prevalent (66%). [Table/Fig-2] shows that diastolic dysfunction was more prevalent among males (76%) compared to females (24%) but statistically it was not significant (p =0.088). Out of 41 cases of LVDD, 87.80% cases of grade1 LVDD (29 males and 7 females) and 12.20% cases of grade 2 LVDD (2 males and 3 females) were found. No case of grade 3 LVDD, grade 4 LVDD or systolic dysfunction (EF<50%) was found in the study. In this study, further, the population with LVDD in 2D echo was compared with the population without LVDD using various parameters like FPG, age, HbA1C level, BMI, serum total cholesterol level [Table/Fig-3]. The mean HbA1C of population with LVDD was found higher (7.67±0.90%) as compared to population without LVDD (7.24±0.64%) [Table/Fig-4]. Correlation was found significant using unpaired t-test (p-value=0.0057). This signifies that higher the HbA1C at the time of diagnosis, higher will be the incidence of LVDD. Age of the patients was very significantly associated with incidence of LVDD (p=0.0012), meaning that older the age at the time of diagnosis, higher the incidence of LVDD. BMI (p=0.0702) and serum cholesterol (p=0.1827) were not found to be significantly correlated with incidence of LVDD in this study.
Age and sex wise distribution of cases
| Age Group (Yrs) | Total | Male | Female | LVDD |
|---|
| No. | % | No. | % | No. | % | No | % |
|---|
| 30-39 | 06 | 06 | 03 | 4.61 | 03 | 8.57 | 4 | 9.75 |
| 40-49 | 37 | 37 | 21 | 32.30 | 16 | 45.71 | 10 | 24.39 |
| 50-60 | 57 | 57 | 41 | 63.07 | 16 | 45.71 | 27 | 65.85 |
| Total | 100 | 100 | 65 | 65 | 35 | 35 | 41 | 41 |
Distribution of LVDD according to sex
| Sex | LVDD | Total |
|---|
| Present | Absent |
|---|
| Male | 31 | 34 | 65 |
| Female | 10 | 25 | 35 |
| Total | 41 | 59 | 100 |
P=0.0881 Relative risk = 1.669 95% Confidence Interval= 0.9322 to 2.989
Comparative parameters of the patients with LV diastolic dysfunction (LVDD)
| Parameters | With LVDD | Without LVDD | p-value (t-test) |
|---|
| No. of Patients | 41 | 59 | - |
| Fasting Plasma Glucose (mg/dl) | 189.85 ± 30.92 | 174.45 ± 29.81 | 0.0140 |
| HbA1C (%) | 7.67 + 0.90 | 7.24 + 0.64 | 0.0057 |
| AGE (year) | 52.46 + 5.59 | 48.42 + 6.15 | 0.0012 |
| BMI (kg/m2) | 25.89+ 2.64 | 24.95+ 2.45 | 0.0702 |
| S. Cholesterol (mg/dl) | 190.26 ± 22.47 | 184.54± 19.58 | 0.1827 |
Relationship of LVDD with HbA1C (%)
Discussion
In this study, conducted in western U.P., we assessed the incidence of LVDD, a precursor of diabetic cardiomyopathy and its correlation with glycosylated haemoglobin (HbA1C) and with other parameters like age, BMI and total serum cholesterol in 100 newly diagnosed normotensive, type 2 diabetic patients between the age of 30 to 60 years. LVDD was found in 41% of patients in this study with a predominance of Grade I LVDD (87.80%) evidenced by delayed relaxation time pattern in pulsed doppler echocardiography. No case of LV systolic dysfunction was found. Study demonstrated high incidence of diastolic dysfunction in normotensive and asymptomatic type 2 diabetics even at the time of diagnosis.
Diastolic dysfunction in diabetic patients is believed to represent an earlier stage in the natural history of diabetic cardiomyopathy its timely recognition may help to avoid or significantly delay the onset of CHF [11]. Patil et al., in their study, of 127 asymptomatic subjects found the prevalence of diastolic dysfunction in asymptomatic type 2 diabetics as 54.33% [12]. Higher prevalence could be attributed to the duration of diabetes in these patients, because unlike our study, cases of diabetes were already diagnosed and were of more than 5 years duration. Absence of cases with systolic dysfunction signifies that diastolic dysfunction is the earliest marker of diabetic cardiomyopathy which precedes systolic dysfunction.
Mean of HbA1C (%) was found higher in group with LVDD (7.67±0.90) as compared to group without LVDD (7.24±0.64). This concludes that HbA1C is strongly associated with presence of LVDD (p=0.0057). Incidence of LVDD was also found higher in older patients group specially above 50 year and this correlation was most significant (p=0.0012). Celentano et al., also studied subjects with normal glucose tolerance, with impaired glucose tolerance, and with type 2 DM and found early signs of diastolic dysfunction (assessed by E/A mitral flow ratio), not only in patients with diabetes but also in those with impaired glucose tolerance, independent of the confounding role of ischemia, body weight, and blood pressure [13]. BMI in our study was also not found to be correlated with LVDD, and similarly, serum cholesterol was also found not to be related with LVDD.
Holzmann et al., showed in a middle-aged population without previously diagnosed DM a continuous relationship between concentrations of fasting plasma glucose, HbA1C and LVDD [14]. So, present study confirmed previous findings. Study done by Shreshta et al., in 100 asymptomatic type 2 Diabetes Mellitus, LVDD was found in 71 subjects of whom 60 had impaired relaxation and 11 had a Pseudo normal pattern of ventricular filling detected by Doppler Echo which included Valsalva Maneuver [15].
Conclusion
This study shows that higher HbA1C level (more than 7.24±0.64) is strongly associated with presence of LVDD, considered as precursor of diabetic cardiomyopathy. HbA1C emerges as an important indicator of diastolic dysfunction in early onset diabetes population in the study. Age at the time of diagnosis of type 2 DM was predicted as the most important risk factor for LVDD in these newly diagnosed patients.
P=0.0881 Relative risk = 1.669 95% Confidence Interval= 0.9322 to 2.989