Cytomegalovirus (CMV) pseudotumour of the gastrointestinal tract, is a rare benign entity which is treated with antiviral medications and known to resolve spontaneously in a few cases. This is a case report of a 58-year-old man who presented with right lower quadrant abdominal pain. Contrast enhanced computerized tomography of abdomen and pelvis showed apple core lesion involving proximal transverse colon, ceacum, ascending colon, ileoceacal valve and terminal ileum. Synchronous carcinoma of colon was suspected. At laparotomy, there was growth palpable only in the proximal transverse colon. Histological findings of biopsy specimen revealed CMV pseudotumour. CMV pseudo tumour should be included in the differential diagnosis of apple core lesions of the colon even in immunocompetent adults. Endoscopy and biopsy are strongly recommended before surgery in colonic mass lesions to make a definitive diagnosis and to avoid unnecessary surgery.
Case Report
A 58-year-old man presented to the emergency department with one week history of fever, right lower quadrant abdominal pain, vomiting and loss of appetite. Physical examination revealed tenderness in the right lower quadrant of the abdomen with a firm, irregular mass palpable in the right iliac fossa region. Rest of the examination was unremarkable. Laboratory investigations showed an elevated white blood cell count of 16,370 cells/mm3 with 83% neutrophils. His liver and renal function tests were normal. A provisional clinical diagnosis of malignancy versus appendicitis with appendicular mass was made.
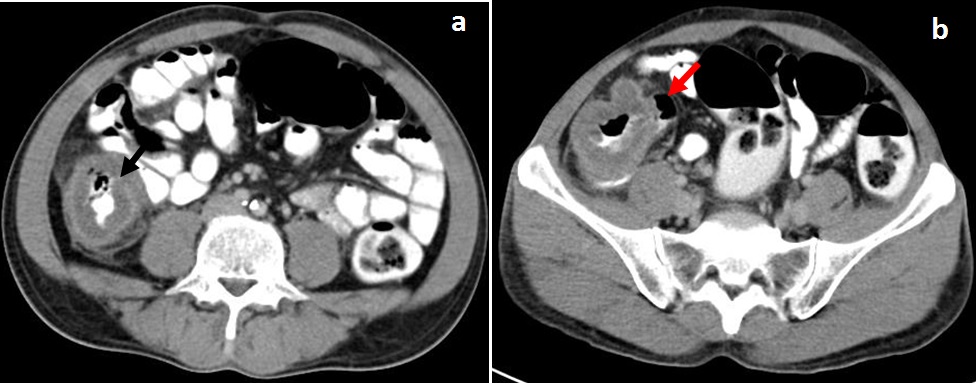
On hospital day 2, 128 slice multidetector contrast enhanced computed tomography (CECT) of abdomen and pelvis showed long segment (50 to 55mm) marked circumferential bowel wall thickening of ascending colon having maximum wall thickness of 20mm with significant luminal narrowing. Concentric bowel wall thickening of cecum, ileo-cecal junction and terminal ileum was also noted with significant luminal narrowing [Table/Fig-1a,b]. Focal eccentric bowel wall thickening of proximal transverse colon predominantly along posterior aspect was noted with mild luminal narrowing [Table/Fig-2,3]. A Synchronous carcinoma of colon was suspected.
Axial CECT images (a,b) showing long segment concentric bowel-wall thickening of ascending colon (black arrow) and cecum (red arrow) with significant luminal narrowing
Axial CECT image showing focal eccentric bowel-wall thickening of proximal transverse colon (yellow arrow) with mild luminal narrowing

Coronal MPR contrast enhanced CT image showing long segment concentric bowel-wall thickening of ascending colon and cecum with significant luminal narrowing - appearing as an apple core lesion (black arrow)

Patient underwent exploratory laparotomy on hospital day five. Intraoperatively there was no growth palpable in cecum, ileoceacal valve, terminal ileum or ascending colon. There was growth palpable only in the proximal transverse colon. Appendix was inflamed. Right hemi colectomy with ileo transverse anastomosis and appendectomy was performed.
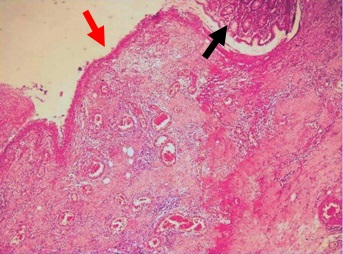
Gross inspection of the colonic mucosa showed multiple ulcers covered with slough [Table/Fig-4]. Microscopy showed eroding ulcerated lesions covered with granulation tissue and dense mixed inflammatory cells [Table/Fig-5]. Intranuclear eosinophilic inclusions were seen. Histopathology was consisistent with CMV pseudotumour. Immunohistochemistry (IHC) was not performed. His postoperative course was uneventful. However, on postoperative day eight he left the hospital against medical advise. He refused to take oral antivirals such as gancyclovir and was subsequently lost to follow up.
Right hemicolectomy specimen showing multiple ulcers covered with slough (yellow arrow)

Histopathology microphotograph shows eroding ulcerated lesions (red arrow) with granulation tissue and dense mixed inflammatory cells. Adjacent normal colonic mucosa (black arrow) is also seen
Discussion
Cytomegalovirus induced pseudo tumour is a rare entity. Only six cases were reported in immunocompetent patients [1–7] and out of them, only two presented as vanishing tumour with spontaneous complete remission [5,7].
CMV is an enveloped, double-stranded and the largest of the Herpesviridae viruses. CMV Infections in the immunocompetent and immunosupressed are not rare; seroprevalence for CMV worldwide ranges approximately from 60%–100% [2].
In immunocompetent patients, primary CMV infection presents as an undifferentiated viral syndrome, or as a mononucleosis-like syndrome. Though considered having a benign, self-limited course, there are reports of severe clinical manifestations with involvement of gastrointestinal tract and the central nervous system as the most frequent sites. Immunocompetent patients in intensive care units, severe sepsis, malnourishment, major trauma and widespread burns may be at risk [2].
Gastrointestinal involvement with CMV can result in gastroenteritis, duodenitis, ileitis, colitis, proctitis or exacerbation of inflammatory bowel disease [8]. The CMV infection of the colon usually manifests as multiple erosions or ulcers and may cause perforation in severe cases. Uncommon manifestations of CMV infections include solitary mucosal ulcers, toxic megacolon, pseudo membrane formation and ischemic colitis [7]. However, the rare presentation of CMV associated gastrointestinal pseudotumours presenting as intraluminal inflammatory polypoidal masses or strictures is reported mostly in immunocompromised patients. Only 31 cases of CMV pseudo tumour colitis were reported so far, among them 17 cases were in HIV positive patients [9–11]. Fourteen cases were reported in non HIV patients and only 6 out of them were in immunocompetent patients. Other case reports in immunocompromised individuals were in patients with organ transplantation, immunodeficiency secondary to common variable immuno deficiency syndrome, chronic renal failure or those receiving steroid therapy or chemotherapy [8,9,12].
Patients with CMV pseudotumour of bowel frequently present with abdominal pain and as non obstructing mass. Other uncommon presentations include fever, change of bowel habits, weight loss, palpable mass, gastrointestinal bleeding and as obstructing mass [9]. The distribution of the inflammatory pseudo tumours include esophagus, fundus, antrum and pylorus of stomach, duodenum, small bowel and colon. Affinity for ileum and right colon was reported [9], similar to our case.
The thickening of bowel wall in patients with CMV is caused histologically by sub mucosal oedema, exuberant granulation tissue, inflammation and fibrosis which lead to the pseudo tumour appearance [9].
Abdominal computed tomography (CT) and barium enema are the most useful imaging studies for CMV colitis. Classic findings include mucosal irregularity and ulceration, bowel lumen strictures, thickened bowel wall and inflammatory infiltration. CMV pseudotumour typically appears as annular regions of luminal narrowing and poor distensibility leading to apple core appearance. These lesions have a sharp transition point to a more normal-appearing colon and can simulate annular constricting carcinoma of the colon. Although these two imaging studies are highly sensitive, the findings are nonspecific for CMV colitis and can be present in colitis of any aetiology [11]. Endoscopic findings comprise of a friable stenosing lesion or a large intraluminal polypoid mass beyond which the colonoscope could not be passed. This is associated with ulcers or erosions [6].
Haematoxylin and eosin staining of the biopsy specimens showing intra nuclear eosinophilic inclusions together with IHC is considered the gold standard in diagnosis of gastrointestinal CMV [9,13].
In addition to CMV pseudotumour, several diseases can cause the appearance of the apple-core lesion of the colon on CT which includes colonic adenocarcinoma, lymphoma, Crohn’s disease, chronic ulcerative colitis, ischaemic colitis, Chlamydia infection, Tuberculosis, Histoplasmosis, Helminthoma, Amoebiasis, villous adenoma, focal diverticulitis, endometriosis, serosal metastatic implants, radiosurgery, NSAID induced colitis and rarely focal amyloidosis [14].
The CMV induced pseudotumour often responds to intravenous antiviral therapy, though response to oral valganciclovir is also reported in one case. Surgical intervention should be reserved for patients whose lesions fail to respond to medical therapy alone or those who present with a surgical indication such as outlet obstruction [9].
To the best of our knowledge only two case reports of CMV induced pseudotumour of the gastrointestinal tract in immunocompetant patients presented as vanishing tumour with spontaneous complete remission and showed improvement without antiviral therapy or surgery. The distribution of the pseudotumour was similar to our case at ileoceacal valve in one case and involved gastric antrum in other case. The pseudotumour disappeared by 7th and 4th week at ileocecal valve and gastric antrum respectively [5,7]. However, in our case there was partial resolution with persistence of pseudo tumour at proximal transverse colon during surgery.
Conclusion
CMV pseudotumour should be included in the differential diagnosis of gastrointestinal mass lesions not only in HIV/AIDS patients and other immunocompromised patients but also in immunocompetent patients. This condition often responds to intravenous or oral antiviral therapy and can even spontaneously resolve in immunocompetent patients like in our case and thus unnecessary surgeries can be avoided.
The purpose of this case report was to familiarize radiologists and surgeons with this potentially treatable rare benign entity. Endoscopic evaluation and histological examination of the lesions is needed to rule out a possible infectious aetiology and is strongly recommended before surgery for suspected masses of the gastrointestinal tract diagnosed on imaging.
[1]. Galiatsatos P, Shrier I, Lamoureux E, Szilagyi A, Meta-analysis of outcome of cytomegalovirus colitis in immunocompetent hostsDig Dis Sci 2005 50:609-16. [Google Scholar]
[2]. Rafailidis PI, Mourtzoukou EG, Varbobitis IC, Falagas ME, Severe cytomegalovirus infection in apparently immunocompetent patients: a systematic reviewVirol J 2008 5:47 [Google Scholar]
[3]. Ryu KH, Yi SY, Cytomegalovirus ileitis in an immunocompetent elderly adultWorld J Gastroenterol 2006 12:5084-86. [Google Scholar]
[4]. Cheung AN, Ng IO, Cytomegalovirus infection of the gastrointestinal tract in non-AIDS patientsAm J Gastroenterol 1993 88:1882-86. [Google Scholar]
[5]. Garcia F, Garau J, Sierra M, Marco V, Cytomegalovirus mononucleosis associated antral gastritis simulating malignancyArch Intern Med 1987 147:787-88. [Google Scholar]
[6]. Maiorana A, Torricelli P, Giusti F, Bellini N, Pseudoneoplastic appearance of cytomegalovirus-associated colitis in non immunocompromised patients:report of 2 casesClin Infect Dis 2003 37:e68-71. [Google Scholar]
[7]. Kawasaki S, Osawa S, Sugimoto K, Cecal vanishing tumour associated with cytomegalovirus infection in an immunocompetent elderly adultWorld J Gastrointest Oncol 2010 2(11):417-20. [Google Scholar]
[8]. Jesus AD, Grossman SA, Paun O, Cytomegalovirus associated colonic pseudotumour: a consequence of iatrogenic immunosuppression in a patient with primary brain tumour receiving radiation and temozolomideJ Neurooncol 2009 94(3):445-48. [Google Scholar]
[9]. Kelesidis T, Tozzi S, Mitty R, Worthington M, Fleisher J, Cytomegalovirus pseudotumour of the duodenum in a patient with AIDS: an unrecognized and potentially treatable clinical entityInt J Infect Dis 2010 14:e274-82. [Google Scholar]
[10]. Rajan Cytomegalovirus infection presenting as a colonic mass in a patient with acquired immunodeficiency syndromeInt Med Case Rep J 2011 4:55-58. [Google Scholar]
[11]. Yudelowitz B, Mahomed A, Cytomegalovirus duodenitis, pseudotumour and cholangiopathy in advanced HIVS Afr Med J 2010 100(11):719-20. [Google Scholar]
[12]. Imam SZ, Khan A, Jaso JM, Foringer JR, Quiz page. CMV colitis presenting as a colonic massAm J Kidney Dis 2010 55:A35-37. [Google Scholar]
[13]. Tan CB, Cytomegalovirus infection of the colon presenting as a mass like lesionCase Rep Gastroenterol 2012 6(2):266-72. [Google Scholar]
[14]. Alzaraa A, Krzysztof K, Uwechue R, Tee M, Selvasekar C, Apple-core lesion of the colon: a case reportCases J 2009 2:7275 [Google Scholar]