Replacement of the lost tooth/teeth due to dental caries, chronic periodontitis, trauma or anodontia results in loss of structural balance, inefficient oral function, poor aesthetics and psychological effects on human beings. Such patients require restoration to achieve normal contour, function, comfort, aesthetics, speech, and overall health. Since centuries missing teeth are replaced using several natural or synthetic substitutes. Conventional rehabilitating methods like removable partial dentures, resin bonded restorations and fixed partial dentures have certain drawbacks such as poor tissue tolerance or discomfort and unacceptance of removable partial dentures, patient’s and dentist’s reluctance to sacrifice sound tooth tissue to accommodate fixed partial dentures and unpredictable survival rates of resin-bonded restorations. Dental implants are latest modality of treatment for partial and completely edentulous patients.
History of dental implants dates back to thousands of years and includes civilizations such as the ancient Chinese 4000 years ago inserted small bamboo sticks into the jaw bone for fixed tooth replacement [1]. Egyptians used ferrous and precious metals; Incas used pieces of sea shells to replace missing teeth [1]. The goal of implant surgery is to insert an endosteal implant in the proper location and angulation so that it will be used as a prosthetic abutment.
The implant dentistry market is exponentially increased with number of implant systems with wide range of rates. The clinical success of few old implant systems have been carried out but recently introduced and economic implant systems are still under clinical surveillance. This study was aimed to assess the clinical success rate of Hi-Tec implant system, which is economical and new in the market. Results of this study will guide the clinician for appropriate implant selection in this competitive market.
Materials and Methods
The study was conducted in the Department of Oral and Maxillofacial Surgery from 2007-2014. In this study we used Single root form implants (Life care, EZ, Hi-Tec, Two stage, Internal Hex, Tapered Self Thread) [Table/Fig-1], Radiographic template (Life care, Hi-Tec), Diagnostic stent & Steel ball, X-ray mesh [Table/Fig-2], Bone caliper, Periotest (Siemen’s) [Table/Fig-3]. The study included ten patients of age 19 to 31 years, out of which 5 males and 5 females, who were in need of restoration of missing mandibular first molar and willing to return for follow-up visits. All the patients demonstrated good general and oral health with motivation to have implant restoration. The procedure was explained, followed by informed written consent.
Showing Single-tooth Hi Tec Implant
Showing the PT Value using PERIOTEST

Inclusion criteria for the study: The patients with history of extraction of mandibular first molar not less than 3 months, not willing to have a removable/fixed partial denture with insufficient periodontal support on natural abutments for a conventional fixed partial denture having edentulous space in the region of mandibular first molar with sufficient bone quality and quantity of 5 mm width, 8mm length & 10 mm height to allow for insertion of at least a 3.3 × 8 mm Life care, Hi-Tec implant were involved in this study.
Exclusion criteria for the study: The patients with systemic conditions which puts the patient at risk during surgery, having habit of smoking, tobacco chewing and alcohol abuse with history of head neck radiotherapy, psychological problems, and para-functional habits like bruxism were excluded from this study.
Methodology
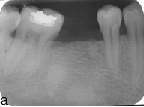
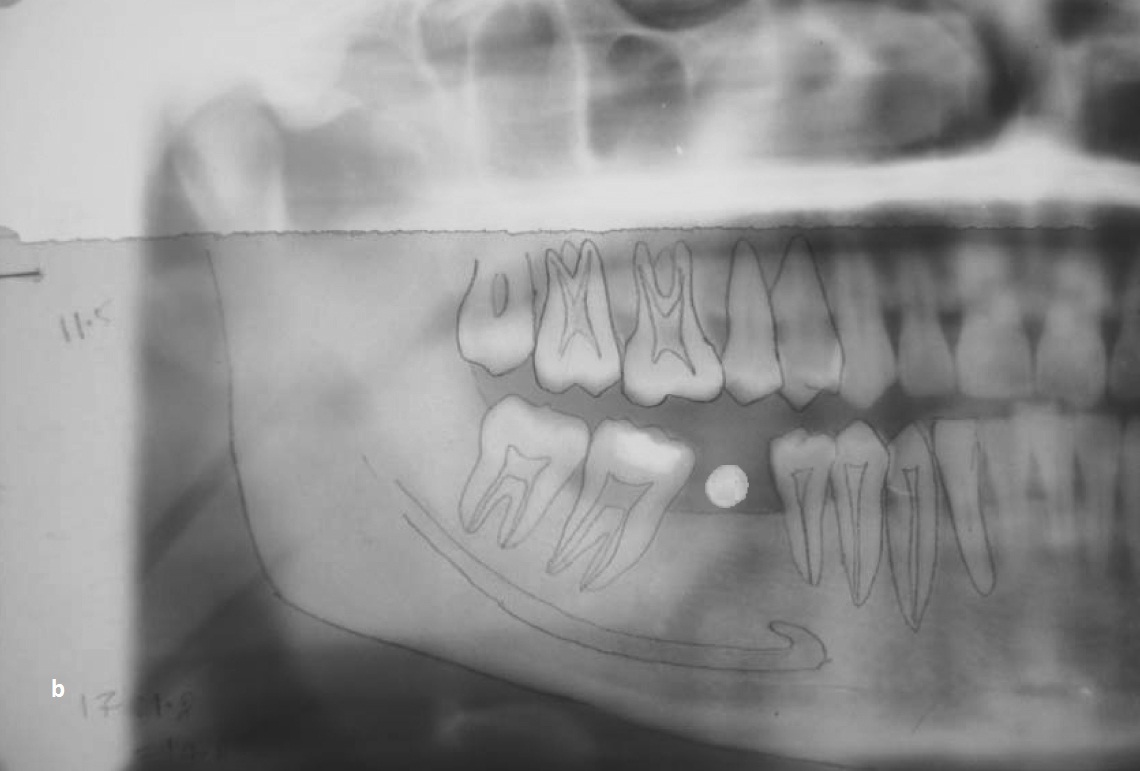
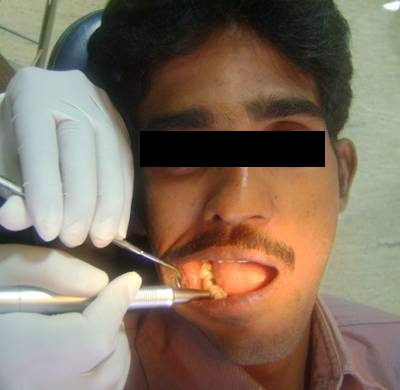
Diagnosis of the patient was done with proper pre-operative analysis through history, clinical [Table/Fig-4], radiographic examination, and routine blood investigations. In each patient, the intra-arch relationship was evaluated using diagnostic casts. Standardized intra oral periapical radiographs using long cone paralleling technique and Panoramic radiographs [Table/Fig-5a] were taken to assess bone and surrounding structures. A diagnostic stent was prepared with steel ball of 5 mm diameter at predetermined implant location and second panaromic radiographic [Table/Fig-5b] was taken. The standardized diameter of the steel ball was used as a reference to assess the radiographic distortion factor. The obtained image allowed for precise evaluation of the available bone height above the mandibular canal for the selection of implant length. Ridge mapping was done using bone caliper to determine the alveolar ridge width for the selection of implant diameter. An individualized acrylic resin surgical stent was fabricated for each patient to obtain an ideal position for implant placement. Oral hygiene instructions given after oral prophylaxis to provide more favorable oral environment for wound healing.
Immediately before surgery, the patients rinsed with 0.12% chlorhexidine mouth wash. Under local anesthesia infiltration (2% lignocaine with 1:80,000 adrenaline), crestal incision was given followed by complete mucoperiosteal flap reflection. Point of entry was marked deep in the bone through the guiding hole made in the surgical stent using a round bur. The implant bed preparation was started with standard pilot drill at the marked point under copious internal and external irrigation of chilled saline. Angulation of the osteotomy drill was checked using paralleling tool. Sequential drilling was done using standard drills with the help of physiodispenser. The longest and widest pre-selected implants were threaded into the prepared site up to the crestal level using ratchet with insertion tool. All implants showed good primary stability. After the placement of implant and adequate stability, the implant mount was removed with the help of hex tool, followed by placement of cover screw. All implants used were having internal hex; the occlusal (platform) aspect of implant is the receiving area for the prosthetic component of restoration. This area of implant was placed at crestal bone level. Implant diameter ranged from 3.3 to 4.2 mm and length from 10 to 13 mm was used. After implant placement, soft tissue edges were sutured to protect the implant sites.
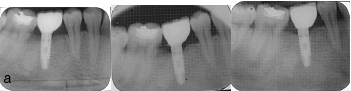
Antibiotics (Cap. Amoxicillin 500 mg tid for 5days) and anti-inflammatory medication (tab Diclofenac sodium bid for 3days) were prescribed for all patients. Sutures were removed after 7days. Chlorhexidine mouth wash used twice daily for 4 weeks. The patients were reviewed at first and third month of first stage surgery. Later 6 months and followed up for 6 years with interval of 12 months. Standardized IOPAs with x-ray mesh were taken to assess the marginal bone levels and peri-implant radiolucency [Table/Fig-6,7a].
Showing edentulous space in mandibular right first molar region

Showing Preoperative IOPA
Showing IOPA Immediately, after 1st and 3rd month post operatively after Implant Insertion
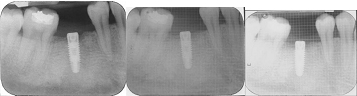
Showing IOPA Immediately after Crown cementation, 1st and 3rd month follow up
The second stage surgical procedure was performed 3 months after the first procedure. Implant was exposed using biopsy punch to remove the cover screw and to place gingival healing cap. Implant mobility was assessed according to clinical implant mobility scale by Carl A Misch [2]. After 2 weeks of healing abutment placement, implants were restored with metal-ceramic single crown prosthesis [Table/Fig-7b]. Patients were reviewed for assessment of implant mobility, marginal bone loss and peri-implant radiolucency at first and third months of crown cementation. [Table/Fig-8] After three months of loading the implant mobility was assessed using PERIOTEST [Table/Fig-9]. Bleeding on probing and probing depth was assessed using standard William’s periodontal probe. All patients were participated in an individually tailored recall schedule first and third month post implant placement, first and third month post prosthetic placement. The total initial follow up period was 6 months following placement of implant. Later patient reviewed every year for 6 years to assess the success rate of implant [Table/Fig-10].
Clinical and radiographic observations: All the ten implants were placed in mandibular first molar region, out of which 6 implants were on right side (60%) and 4 implants were on left side (40%). The sizes of the pre-selected implants varied. The diameter of the implants ranged from 3.3mm to 4.2mm and the mean diameter for males is 3.66 and for female is 4.11 (p=0.007) [Table/Fig-11]. The length of the implants ranged from 10mm to 13mm with mean of 10.9mm for males and 12.4mm for females (p=0.02) [Table/Fig-11]. Bleeding on probing was present in one patient (10%) at first month of loading because of loosening of prosthesis which subsided after cementation of the crown. At third month after crown cementation none of the patient showed bleeding on probing (0%). The probing depth values obtained for all the ten patients at first and third months and subsequent follow up after loading were constant and well within the normal range (1to 3mm) with mean value being 1.8mm and SD of 0.78 [Table/Fig-12]. Even after six years of follow up, no one had significant changes to interpret as implant failure.
Marginal bone levels at crown cementation ranged from 0.5 to 2mm with mean values of 0.95mm on mesial side and 0.82mm on distal side. The marginal bone loss after three months of crown was seen to be ranging from 0 to 0.5mm with mean of 0.13mm on mesial side and 0.15mm on distal side (p<0.05) later it was not significant during subsequent follow up periods [Table/Fig-12,13] The peri-implant radiolucency assessed using standardized IOPA and radiovisiographs (RVG). None of the implants showed peri-implant radiolucency during the follow up period [Table/Fig-14].
Showing OPG after crown cementation

Showing Implants supported prosthesis in occlusion

Showing the evaluation of implant mobility using PERIOTEST
Showing IOPA at the end of study period after 72 months

Showing the comparison of male and female subjects with respect to diameter and Length of the implants placed by t-test
| Male | Female | SD | t-value | p-value |
|---|
| Mean Diameter | 3.6600 | 4.1100 | 0.2012 | -3.5355 | 0.0077* |
| Mean length | 10.900 | 12.400 | 0.8216 | -2.8868 | 0.0203* |
*Significant at 5% level of significance (p<0.05)
Showing the comparison of probing depth (mm) after 1st, 3rd month and 72 months of crown cementation by wilcoxon matched pair test by ranks and Implant mobility test by PERIOTEST PT values
| Male | Female | SD | t-value |
|---|
| After crown 1st month | 1.8000 | 0.7888 | 0.0000 | 1.0000 |
| After crown 3rd month | 1.8000 | 0.7888 | | |
| At the end of study period with time intervals of 12 months until 72 months | - | - | 0.0000 | 1.0000 |
| Implant mobility PT values by PERIOTEST | -1.6000 | 1.0750 | - | - |
Showing the distribution of study subjects by Bleeding on probing, implant mobility according to clinical implant mobility scale and Peri-implant radiolucency at different stages
| Present | Absent | Total |
|---|
| 1) Bleeding on probing for implant |
| After 1st month of crown cementation. | 1 | 9 | 10 |
| After 3rd month of crown cementation | 0 | 10 | 10 |
| at the end of study period with time intervals of 12 months until 72 months | 0 | 10 | 10 |
| 2) Intervals for Implant Mobility |
| At the time of implant placement | 0 | 10 | 10 |
| At the time of 2nd surgery | 0 | 10 | 10 |
| After 1st month of crown cementation | 0 | 10 | 10 |
| After 3rd month of crown cementation | 0 | 10 | 10 |
| at the end of study period with time intervals of 12 months until 72 months | 0 | 10 | 10 |
| 3) Intervals for Peri-implant radiolucency |
| After 1st month of implant placement | 0 | 10 | 10 |
| After 3rd month of implant placement | 0 | 10 | 10 |
| After 1st month of crown cementation | 0 | 10 | 10 |
| After 3rd month of crown cementation | 0 | 10 | 10 |
| At the end of study period with time intervals of 12 months until 72 months | 0 | 10 | 10 |
Showing the comparison of marginal bone level at crown cementation and marginal bone loss after 72 months of crown cementation in mm at mesial and distal side by Paired t-test
| Time | Side | Mean | Std.Dv. | Mean diff. | SD diff. | Paired t-test | p-value |
|---|
| At crown cementation | Mesial side | 0.9500 | 0.6433 | | | | |
| After 3 months of crown cementation | 0.1300 | 0.1567 | 0.8200 | 0.6680 | 3.8818 | 0.0037* |
| At the end of study period with time intervals of 12 months until 72 months | - | - | - | - | - | Non significant |
| At crown cementation | Distal side | 0.8200 | 0.6070 | | | | |
| After 3 months of crown cementation | 0.1500 | 0.1650 | 0.6700 | 0.6767 | 3.1311 | 0.0121* |
| At the end of study period with time intervals of 12 months until 72 months | - | - | - | - | - | Non significant |
*Significant at 5% level of significance (p<0.05)
Discussion
Replacement of lost teeth carried out using dental implants is an internationally accepted treatment modality [2]. The success of an implant depends on osseointegration. An implant forms interlocking and is able to transmit axial loads to the surrounding bone by compression on the inclined faces of the screw threads [2]. If a soft connective tissue layer forms around the implant, loading may lead to some relative motion and gradual degradation of the bone. Osseointegration allows for a direct transfer of stress from the titanium to the bone so that no relative motion occurs at the interface [2].
A consistent philosophy is the desire for clinical rigid fixation corresponding microscopically to a direct bone to implant interface, without intervening fibrous tissue on the major portion of the implant body. Placement of implant is usually performed in two stages like in our study [2]. Stage I surgery involves placement of implant into the bone for a period of 4-6 months for osseointegration depending on the bone quality. In second stage surgery the healing cap placed for proper healing of soft tissue around the site of future abutment followed by placement of abutment and restoration.
The present study included ten patients who were in need of restoration of missing mandibular first molar. The mean diameter of the implants placed in our study was 3.66mm and 4.11mm [Table/Fig-13], whereas mean lengths were 10.9mm and 12.4mm for males and females respectively [Table/Fig-14]. According to Alexandra Behneke [3], in first 2 years more than 80% of the sites showed no bleeding on probing. In the present study bleeding on probing was assessed at first and third month after crown cementation. One patient (10%) had bleeding on probing at first month of loading because of loosening of prosthesis which subsided after recementation of the crown. None of the patients had bleeding on probing at third month of loading (100%) [Table/Fig-12], which was in accordance with results of Alexandra Behneke [3].
Probing depth proved to be the most accurate means of detecting peri-implant destruction. According to Daniel Buser [4] the probing depth values ranged between 1 & 5 mm, the mean probing depth was 2.81 mm. In the study of Alexandra Bhneke [3] the probing depth values were almost constant with median of 1.5 to 2.0 mm. According to Patrick J. Henry [5] the probing depth around implants did not change significantly between the 0 to 3 years and 5 years period of follow-up. In our study the probing depth values obtained were well within the normal range, with mean value of 1.8 mm and SD of 0.78 at first & third month after crown cementation. On comparison of probing depth after first and third month of crown cementation, there was no statistically significant difference with p-value 1 [Table/Fig-14] which was in accordance with the above studies.
Implant mobility is an important clinical parameter that warrants continual assessment during the maintenance period. It may represent the key indicator of fixture health. In the study of Limor Avivi [6] all of the 42 monitored implants were clinically asymptomatic & immobile. In our study implant mobility was assessed using clinical implant mobility scale at the time of implant placement, second stage surgery, first and third month after crown cementation. All the implants were clinically immobile [Table/Fig-14]. PERIOTEST is an electronic device which quantifies the mobility of an implant by measuring the reaction of the peri-implant tissues to a defined impact load [7]. It measures the damping like characteristics of the tissues immediately adjacent to the implants and detects the micro mobility which is attributed to the elasticity of the surrounding bone and it assess the osseointegration of dental implants [7]. The PT values range from -8 to +50, values above 20 are irrelevant in implantology [7], The smaller the PT, the greater the stability damping effect. Negative values are generally good and indicate that the implant is well osseointegrated [1,7]. In the study of Alexandera Behneke [3] the periotest measurements showed negative values with the median of (-4.0) observed after prosthesis placement. After third month of crown cementation we assessed implant mobility using PERIOTEST and the mean PT value was (-01.6) which shows well osseointegrated implants [Table/Fig-13]. These results were in accordance with the above study.
A major criterion for evaluating implant success involves bone level changes around implants [2]. According to William R. Laney [8] mean value of marginal bone loss, mesially 0.14 mm with SD of 0.61 and distally, 0.2 mm with SD of 0.66 was found. Standardized periapical radiographs were used to assess marginal bone loss at the mesial & distal areas of each implant after three months of crown cementation. The mean value of mesial side was 0.13mm with SD of 0.15 and on distal side was 0.15mm with SD of 0.16, which was correlated with the above study. The peri-implant radiolucency is defined as the radiographic evidence of progressive peri-implant bone loss. In the study of Daniel Buser [4] the radiographs obtained of each implant did not reveal any signs of continuous peri-implant radiolucency throughout the observation period of 3 years. In our study none of the implants showed peri-implant radiolucency throughout the follow-up period, which is in accordance with the above study.
In the present study all the 10 implants, placed for restoration of mandibular first molar, healed predictably. There was no bleeding on probing except for one patient who had loosened prosthesis. The probing depths remained constant and well within the normal range. Implant mobility was absent in all the cases with minimal marginal bone loss and without peri-implant radiolucency. All the implants deemed successful at six months of placement according to the clinical criteria [9,10]. Success of implant depends on thick cortical bone which is associated with high implant stability and thus high loading capacity [10]. We excluded smokers in our study because they had a higher incidence of failure and complications following dental implantation and implant related surgical procedures [11].
But there were no same/similar studies found in the literature using our implant. So, the results were compared with the literature in which the same methodology and technique were followed but not the same implant system. The study involved a smaller sample size, with single tooth replacement. The implant is economic when compared with other existing internationally acclaimed (viz. Nobel Biocare) systems [12–14]. But our study warrants the long term studies with a large sample size and multiple replacements along with multi centric randomized blind studies for the predictability of success rate conclusively.
Conclusion
The single-tooth implant restoration using two stage operating technique can be used as a successful treatment modality for restoration of mandibular first molar. However, these results were obtained after six years duration of follow up but with relatively a smaller sample size, the a large sample size with multicenter randomized trail using split mouth and comparison is recommended for the predictability of success rate conclusively.
*Significant at 5% level of significance (p<0.05)
*Significant at 5% level of significance (p<0.05)