Association Between Harmful Oral Habits and Sign and Symptoms of Temporomandibular Joint Disorders Among Adolescents
Vaibhav Motghare1, Jayaprakash Kumar2, Shivalingesh Kamate3, Sumedha Kushwaha4, Richa Anand5, Neha Gupta6, Bhuvandeep Gupta7, Ishan Singh8
1 Private Practitioner, Department of Public Health Dentistry, I.T.S Dental College, Hospital & Research Centre, Greater Noida, India.
2 Professor, Department of Public Health Dentistry, I.T.S Dental College, Hospital & Research Centre, Greater Noida, India.
3 Reader, Department of Public Health Dentistry, I.T.S Dental College, Hospital & Research Centre, Greater Noida, India.
4 P.G. Student, Department of Public Health Dentistry, I.T.S Dental College, Hospital & Research Centre, Greater Noida, India.
5 Senior Lecturer, Department of Public Health Dentistry, I.T.S Dental College, Hospital & Research Centre, Greater Noida, India.
6 Senior Lecturer, Department of Public Health Dentistry, I.T.S Dental College, Hospital & Research Centre, Greater Noida, India.
7 Senior Lecturer, Department of Public Health Dentistry, I.T.S Dental College, Hospital & Research Centre, Greater Noida, India.
8 P.G Student, Department of Public Health Dentistry, I.T.S Dental College, Hospital & Research Centre, Greater Noida, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vaibhav Motghare, Quater No. 3B, Street No. 8, Sector 9, Bhilai, Chhattisgarh-4000, India.
E-mail: vaibhav.motghare@gmail.com
Context
Temporomandibular disorder (TDM) is defined as a heterogenous group of psychophysiological disorders commonly characterised by orofacial pain, chewing dysfunction or both. Various Epidemiological studies had shown occurrence of TMD in all age groups including children. Also research had shown that non nutritional oral habits to be associated with TMD.
Aim
Present study aimed to find whether harmful oral habits are associated with sign and symptoms of TMD among adolescents in Greater Noida.
Setting and Design
Schools in Gautam Buddha district and descriptive study.
Materials and Methods
Cross sectional study was carried out among 240 adolescents (10 – 19 years) studying in schools of Greater Noida. Study population were selected by random sampling to whom screening questionnaires recommended by American Academy of Orofacial Pain (AAOP) were distributed. Patient history and clinical examination was used to determine harmful oral habits. Data analysis was done in SPSS version 21 and Chi-square test was applied.
Results
Sixty one participants (25.4%) displayed no sign and symptoms of TMD, 34 (14.2%) responded affirmatively to atleast one item on the questionnaire and 108(46%) gave at least three affirmative responses. Headache, Neckpain and Toothache were most frequent reported sign and symptoms of TMD (46.2%). There was statistically significant association between gender and sign and symptoms of TMD on three items of the questionnaire (p < 0.05). Nail Biting (45.8%), Biting Lips/objects (37%) were most common habits among the study group. There was statistically significant association between Nail Biting (p = 0.001), Lip Biting/ object biting (p=0.001), Grinding of teeth (p = 0.01) and sign and symptoms of TMD.
Conclusion
A statistically significant association was found between nail biting, lip/ object biting and grinding of teeth with signs and/or symptoms of TMD. Thus there is need for preventive dental treatment and community dental education so that young adults realize importance of early diagnosis and treatment of TMJ disorders.
Adolescent health, Cross-sectional study, Orofacial pain, Questionnaire
Introduction
Tempomandibular joint disorder (TMD) is an enigmatic issue for health care professions all around the globe due to its deleterious effect on stomatognathic system. The term is used to describe “group of orofacial conditions affecting temporomandibular joint and its associated structures” [1]. TMD has multifactorial aetiologies with various initiating factors (trauma, parafunctional habits); predisposing factors (systematic, genetic, structural, psychological) and perpetuating factors (metabolic factors, muscle stress) [2]. It initially manifests as quintessential triology of sign and symptoms in which patient usually experience joint pain followed by clicking sound in joint and finally difficulty in mouth opening [1]. Other commonly occurring sign and symptoms are “soreness of muscles of mastication, attrition of teeth and sensitivity, hyper mobility of teeth, headaches in the temple region, pain in the area of forehead and eyes, pain in the back of the head (possibly extending to the shoulders and neck), fullness in the ears, tinnitus, pressure on the eyes, sensitivity to light, dizzy spells, vertigo, nausea, lack of concentration” [3].
Various epidemiological studies had shown occurrence of sign and symptoms of TMD disorders in all age groups with low prevalence among adolescents [4,5]. Study done by Ebrahimi M et al., and Tecco et al., had shown prevalence of 34.7% and 23.7% among adolescents [6,7]. The range of symptoms occurring in adolescents are considered to be mild in nature [8,9]. Study done by Emodi – Perlman et al., had shown non nutritional oral habits like lip biting, nail biting being associated with TMD among adolescents [10]. Thus it is necessary to make the adolescents aware about the harmful oral habits that could lead to TMD’s. Hence, this study was planned to find the association between parafunctional habits and sign and symptoms of TMD among adolescents residing in Gautam Buddha District.
Materials and Methods
Overview of District
The present study was carried out in Gautam Buddh Nagar district of Uttar Pradesh, India which was “established from the portions of Ghaziabad and Bulandshahar on 6/9/97” [11]. Its headquarters are located in Greater Noida and total geographical area is of 1442 Sq. Km [11]. It has three Tehsils and four developmental blocks viz. Bisrakh, Dadri, Dankaur & Jewar [12]. According to 2011 census total population of the district is 1,202,030 with 652,819 males and 549,211 females [13].
Sample Size Calculation
Sample size was determined by conducting a pilot study among 50 adolescents attending OPD in the Department of Public Health Dentistry. Prevalence rate obtained during pilot study was 18% and considering a confidence interval of 95% with precision fixed at 0.05 the sample size calculated by formula:

Where n = sample size; p = approximate prevalence rate of disease prevalence rate; q = 1 – p and Lis permissible error in the estimation of p. n obtained from the pilot study was 236 (236 ~ 240). In the final study 240 adolescents were included for the study. Ethical clearance was approved by Institute Review Committee of I.T.S Dental College Greater Noida.
Inclusion Criteria
Adolescents studying in the schools of the district in age group of 10-19 y present on the day of survey along with their parents were included in the study.
Exclusion Criteria
Adolescents undergoing orthodontic treatment, having cranio-facial injury and not residing in the district were not included in the study.
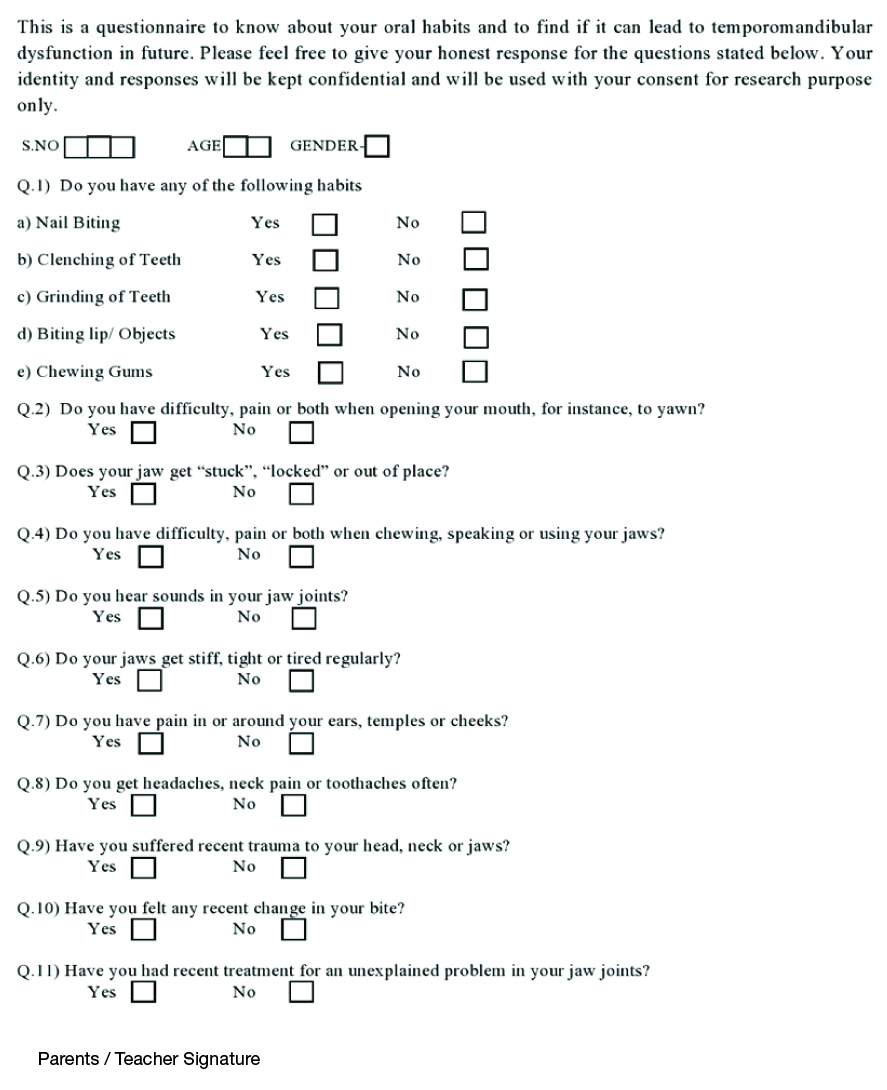
Sampling Procedure
A descriptive cross-sectional study was conducted from January 2014 to June 2014 in which four schools were randomly selected (each school from each developmental block). Informed consent was obtained either from school authorities or parents. Sign and symptoms of TMD and parafunctional habits were analysed by using screening questionnaire recommended by American Academy of Orofacial Pain which consisted of ten questions with yes/no response along with patient history and detailed clinical examination [1,14] [Table/Fig-1]. According to guidelines of AAOP, three or more ‘Yes’ responses indicate TMD [1]. Total 240 adolescents were included from four schools of the district. Clinical Examination was carried by single calibrated examiner in the school premises.
Screening Questionnaire Recommended by “AAOP” Used in the Study
Statistical Analysis
The data obtained was subjected to statistical analysis using Statistical Package for Social Science (SPSS), version 21.0. p-value <0.05 considered as statistically significant at 95% Confidence level. Chi-square test was applied to find association between parafunctional habits and sign and symptoms of TMD.
Results
Study population comprised of 110 (45.8%) male and 130 (54.2%) females with mean age of 13.52± 1.8. Sixty one (25.4%) adolescents reported no sign or symptoms of TMD. Thirty four (14.2%) responded yes to atleast one statement of AAOP questionnaire. 37 (15.4%) participants responded yes to atleast two statements of AAOP questionnaire and a total of 108 (46%) adolescents responded yes to three or more questions.
Total number of 59 (24.6%) participants had no harmful oral habits while 91 (37.9%) and 40 (16.8%) participants had presence of two and three or more habits respectively. Statistically significant association was found between nail biting, biting lip / objects, grinding of teethwith sign and symptoms of TMD (p ≥ 0.05) [Table/Fig-2].
Association between harmful habits and sign and symptoms of TMD
| Harmful habits | Sign & symptoms of TMD | p value |
|---|
| Upto 2 sign and symptoms (n) | 3 or more sign and symptoms (n) |
|---|
| 1. Nail Biting | Yes | 39 | 71 | 0.001* |
| No | 93 | 37 |
| 2. Clenching of teeth | Yes | 26 | 26 | 0.41 |
| No | 106 | 82 |
| 3. Grinding of teeth | Yes | 14 | 24 | 0.625 |
| No | 118 | 84 |
| 4. Biting Lip / Object | Yes | 28 | 61 | 0.001* |
| No | 104 | 47 |
| 5. Chewing Gums | Yes | 41 | 39 | 0.40 |
| No | 91 | 69 |
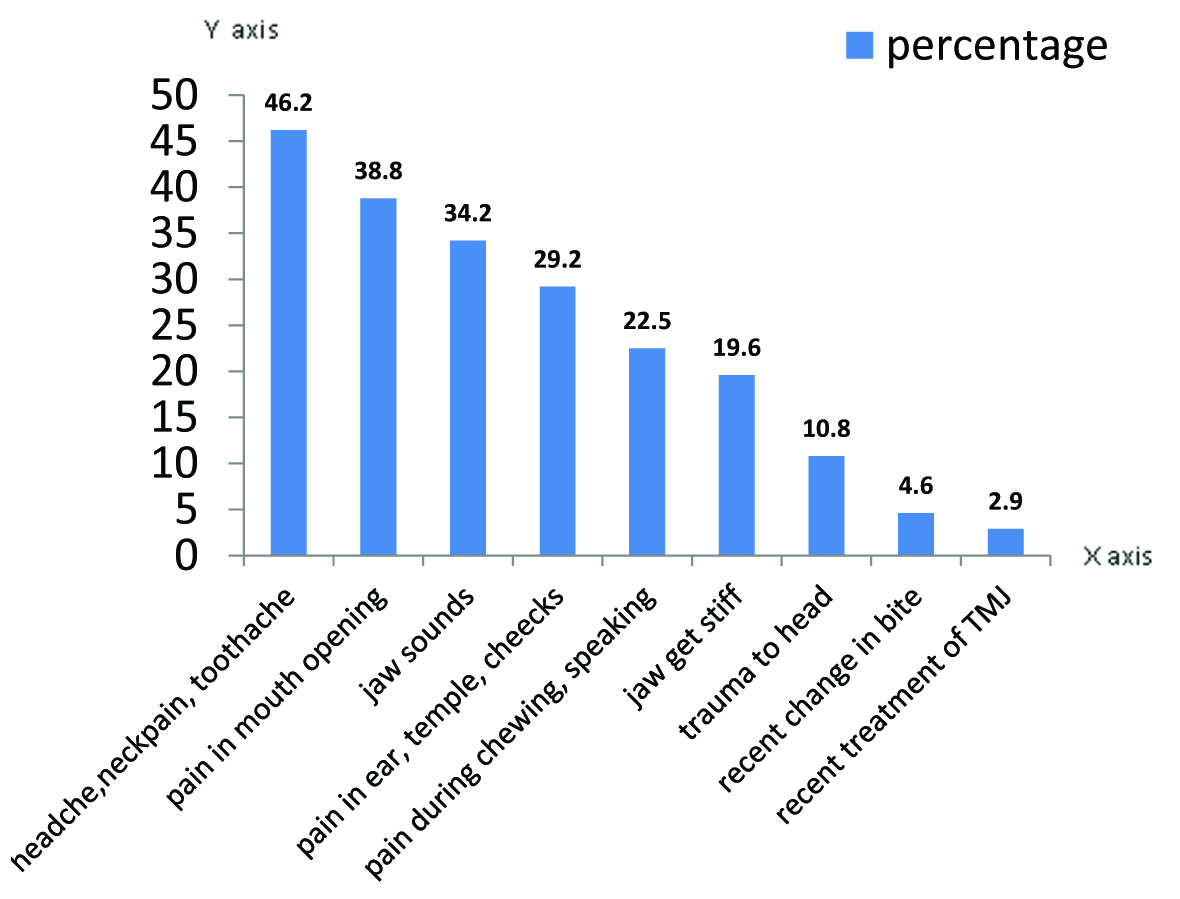
Top three symptoms of TMD reported by study population were headache, neckpain, toothache (46.2%), pain in mouth opening (38.8%) and jaw sounds (34.2%). [Table/Fig-3] describes the detailed description of sign and symtoms of TMD reported by the study population. Statistically significant gender difference was observed for three statements of AAOP questionnaire (p≥ 0.05) [Table/Fig-4] with higher frequency was observed in females for sign and symptoms of TMD when compared to their male counterparts. Higher frequency of TMD symptoms was reported in age group of 13 and 14 y.
Prevalence of sign and symptoms of TMD in study population
Association between gender and sign and symptoms of TMD
| Variables | Male | Female | p-value |
|---|
| Yes | No | Yes | No |
|---|
| 1. | Difficulty, pain while opening your mouth | 43 | 67 | 50 | 80 | 0.92 |
| 2. | Jaw get “stuck”, “locked” or out of place | 12 | 98 | 17 | 113 | 0.60 |
| 3. | Difficulty, pain or both when chewing, speaking or using your jaws | 22 | 88 | 32 | 98 | 0.39 |
| 4. | Hear sounds in your jaw joints | 38 | 72 | 44 | 86 | 0.90 |
| 5 | Jaws get stiff, tight or tired regularly | 15 | 95 | 32 | 98 | 0.03* |
| 6. | Pain around your ears, temples or cheeks | 25 | 85 | 45 | 85 | 0.04* |
| 7 | Getting headaches, neck pain or toothaches often | 53 | 57 | 58 | 72 | 0.58 |
| 8. | Suffered any recent trauma to your head, neck or jaws | 7 | 103 | 19 | 111 | 0.04* |
| 9. | Felt any recent change in your bite | 2 | 108 | 9 | 121 | 0.06 |
| 10. | Recent treatment for an unexplained problem in your jaw joints | 1 | 109 | 6 | 124 | 0.08 |
* = p value ≥ 0.05 was considered statistically significant
Study subjects who gave three or more positive response to the “AAOP” questionnaire were further categorized as “patients with TMD” and who gave upto two positive response were categorized as “without TMD”. Statistically significant association was found between patients with TMD and sign and symptoms like headache, pain in mouth opening, sounds from joint etc [Table/Fig-5].
Frequency & percent of TMD according to presence of sign & symptoms
| Sign & Symptoms | Without TMD N(%) | With TMD N (%) | Total | p value |
|---|
| 1. | Difficulty, pain while opening your mouth | Yes | 15 (16.2%) | 78 (83.8%) | 93 (100%) | 0.001* |
| No | 114 (27.6%) | 33 (22.4%) | 147 (100%) |
| 2. | Jaw get “stuck”, “locked” or out of place | Yes | 8 (27.5%) | 21 (72.5%) | 29 (100%) | 0.003* |
| No | 121 (57.3%) | 90 (42.7%) | 211 (100%) |
| 3. | Difficulty, pain or both when chewing, speaking or using your jaws | Yes | 13 (24.1%) | 41 (75.9%) | 54 (100%) | 0.001* |
| No | 116 (62.3%) | 70 (37.7%) | 186 (100%) |
| 4. | Hear sounds in your jaw joints | Yes | 8 (9.8%) | 74 (90.2%) | 82 (100%) | 0.001* |
| No | 121 (76.5%) | 37 (23.5%) | 158 (100%) |
| 5. | Jaws get stiff, tight or tired regularly | Yes | 15 (32%) | 32 (68%) | 47 (100%) | 0.001* |
| No | 114 (59%) | 79 (41%) | 193 (100%) |
| 6. | Pain around your ears, temples or cheeks | Yes | 14 (20%) | 56 (80%) | 70 (100%) | 0.001* |
| No | 115 (67.6%) | 55 (32.4%) | 170 (100%) |
| 7. | Getting headaches, neck pain or toothaches often | Yes | 26 (23.5%) | 85 (76.5%) | 111 (100%) | 0.001* |
| No | 103 (79.8%) | 26 (20.2%) | 129 (100%) |
| 8. | Felt any recent change in your bite | Yes | 2 (18.2%) | 9 (81.8%) | 11 (100%) | 0.015* |
| No | 127 (55.4%) | 102 (44.5%) | 229 (100%) |
| 9. | Suffered any recent trauma to your head, neck or jaws | Yes | 4 (15.4%) | 22 (84.6%) | 26 (100%) | 0.001* |
| No | 125 (58.4%) | 89 (41.5%) | 214 (100%) |
* = p-value ≥ 0.05 was considered statistically significant
Discussion
Present study was aimed to find association between parafunctional habits and sign and symptoms of TMD among adolescent residing in Gautam Buddha District. In present study there was statistically significant association between harmful oral habits (nail biting;object/lip biting;grinding of teeth) and sign and symptoms of TMD with higher frequency of sign and symptoms observed among females which was accordance to study done by Lauriti et al.,[15]. Previous published literature had enumerated factors like hormonal, genetic, emotional factors which contribute to higher prevalence of TMD among females [16–18]. Significant gender difference was observed in present study for sign and symptoms of TMD which was similar to previous published reports among Iranian and Swedish adolescents [6,18].
Study done by Lobbezoo et al., and Respetro C et al., had stated “bruxism, clenching/grinding of teeth, nail biting, object biting, forward thrust of mandible as parafunctions” [19,20]. In present study statistically significant association was found between Nail biting and TMD. The results were in accordance to study done by Wincur E et al., and Troeltzsch M et al., while Almoudi N et al., and Emodi- Perlman A et al., found no association [10,21–23]. These parafunctional habits should be considered as risk factor for TMD as they act as triggering point for appearance of TMD due to its effect on stomatognathic system.
In present study 46% of adolescents showed sign and symptoms of TMD. Study done by Motta et al., and Thailander et al., showed the prevalence to be 20% and 25% among adolescents, Morinushi et al., showed the prevalence to be 31% in age group of 12 – 14 years and 39.6% among 15- 17 y and Nunes et al., (1997) used helmiko index along with AAOP questionnaire and concluded that 34% adolescents showed mild symptoms of TMD [1,5,24,25]. Headache, neckpain, toothache (46.2%), sounds in the joint (38.7%) and pain in mouth opening (34.1%) were top three sign and symptoms of TMD, similarly observed by Motta et al., among Brazilian adolescents [1]. These three sign and symptoms are considered as classic traid of TMD disorder occurring in a sequential pattern.
AAOP Questionnaire is being recommended by American Association of Orofacial Pain and can be used for screening and diagnosis of individuals with TMD disorders. These screening questionnaires can help in initial identification of individuals having sign and symptoms of TMD which can be sent further for preventive treatment.
Conclusion
This study concluded that there was an association between parafunctional habits and sign and symptoms of TMD, however one of the limitation of this screening questionnaire was that it does not measure the severity of sign and symptoms of TMD and hence further studies need to be conducted for generalizibility of the results.
* = p value ≥ 0.05 was considered statistically significant
* = p-value ≥ 0.05 was considered statistically significant
[1]. Motta LJ, Guedes CC, De Santis TO, Fernandes KP, Mesquita-Ferrari RA, Bussadori SK, Association between parafunctional habits and signs and symptoms of temporomandibular dysfunction among adolescentsOral Health Prev Dent 2013 11(1):3-7. [Google Scholar]
[2]. Venkateswaran S, Saravanakumar Annamalai Divya Yamini Diagnosis & Management of Temporomandibular Joint Disorders- What the Medical and Dental practitioners should know?Chettinad Health City Medical Journal 2013 2(2):52-59. [Google Scholar]
[3]. Okeson JP, Orofacial PainOrofacial Pain: Guidelines for Assessment, Diagnosis, and Management1996ChicagoQuintessence:113-84. [Google Scholar]
[4]. Egermark I, Carlsson GE, Magnusson T, A 20-year longitudinal study of subjective symptoms of temporomandibular disorders from childhood to adulthoodActa Odontol Scand 2001 59(1):40-48. [Google Scholar]
[5]. Thilander B, Rubio G, Pena L, deMayorga C, Prevalence of temporomandibular dysfunction and its association with malocclusion in children and adolescents: an epidemiologic study related to specified stages of dental developmentAngle Ortho 2002 72(2):146-54. [Google Scholar]
[6]. Ebrahimi M, Dashti H, Mehrabkhani M, Temporomandibular disorders and related factors in a group of Iranian adolescents: a cross-sectional surveyJ Dent Res Dent Clin Dent Prospects 2011 5:123-27. [Google Scholar]
[7]. Tecco S, Crincoli V, Di Bisceglie B, Saccucci M, Macrí M, Polimeni A, Festa F, Signs and symptoms of temporomandibular joint disorders in Caucasian children and adolescentsCranio 2011 29(1):71-79. [Google Scholar]
[8]. Egermark-eriksson I, Carlsson GE, Ingervall B, Prevalence of dysfunction and orofacial parafunction in 7-, 11- and 15-year-old Swedish childrenEuropean Journal of Orthodontics 1981 3:163 [Google Scholar]
[9]. Nilner M, Functional disturbances and diseases of the stomatognathic system. A cross-sectional studyJ Pedod 1986 10(3):211-38. [Google Scholar]
[10]. Emodi-Perlman A, Eli I, Friedman-Rubin P, Bruxism, oral parafunctions, anamnestic and clinical findings of temporomandibular disorders in childrenJ Oral Rehabil 2012 39:126-35. [Google Scholar]
[11]. Joshi BC. District Brochure of Gautam Budh Nagar, U.P. 2008 – 09 At: URL: http://cgwb.gov.in/District_Profile/UP/GB%20Nagar.pdf. [Accessed on 1st August 2013] [Google Scholar]
[12]. Website of Gautam Buddha District. 2000; Available from: URL: http://gbnagar.nic.in/. [Accessed on 1st August 2013] [Google Scholar]
[13]. Government of India and Ministry of Home Affairs 2013; Available from: URL: http://censusindia.gov.in/. [Accessed on 1st August 2013] [Google Scholar]
[14]. Micheloni A, Fernandes G, Goncalves D, Camparis C, Temporomandibular disorders among Brazilian adolescents: reliability and validity of a screening questionnaireJ Appl Oral Sci 2014 22(4):314-22. [Google Scholar]
[15]. Lauruti L, Motta L, Silva P, Are Occlusal Characteristics, Headache, Parafunctional Habits and Clicking Sounds Associated with the Signs and Symptoms of Temporomandibular Disorder in Adolescents?J PhysTher Sci 2013 25(10):1331-34. [Google Scholar]
[16]. Kafas P, Leeson R, Assessment of pain in temporomandibular disorders: the bio-psychosocial complexityInt J Oral MaxillofacSurg 2006 35:145-49. [Google Scholar]
[17]. Magnusson T, Egermark I, Carlsson GE, A longitudinal epidemiologic study of signs and symptoms of temporomandibular disorders from 15 to 35 years of ageJ Orofac Pain 2000 14:310-19. [Google Scholar]
[18]. Nassif NJ, Al-Salleeh F, Al-Admawi M, The prevalence and treatment needs of symptoms and signs of temporomandibular disorders among young adult malesJ Oral Rehabil 2003 30:944-50. [Google Scholar]
[19]. Lobbezoo F, van der Zaag J, van Selms MK, Principles for the management of bruxismJ Oral Rehabil 2008 35:509-23. [Google Scholar]
[20]. Restrepo C, Gomez S, Manrique R, Treatment of bruxism in children: a systematic reviewQuintessence Int 2009 40:849-55. [Google Scholar]
[21]. Winocur E, Gavish A, Finkelshtein T, Oral habits among adolescent girls and their association with symptoms of temporomandibular disordersJ Oral Rehabil 2001 28:624-29. [Google Scholar]
[22]. Troeltzsch M, Cronin RJ, Brodine AH, Prevalence and association of headaches, temporomandibular joint disorders, and occlusal interferencesJ Prosthet Dent 2011 105:410-17. [Google Scholar]
[23]. Alamoudi N, Correlation between oral parafunction and temporomandibular disorders and emotional status among saudi childrenJ ClinPediatr Dent 2001 26:71-80. [Google Scholar]
[24]. Morinushi T, Ohno H, Ohno K, Oku T, Ogura T, Two year longitudinal study of the fluctuation of clinical signs of TMJ dysfunction in Japanese adolescentsJ ClinPediatr Dent 1991 15(4):232-40. [Google Scholar]
[25]. Nunes R, Martins MC, Martins EA, Prevalência da Síndrome da Disfunçãoemjovens de 14 a 20 anos de idade. Utilização do Índice de HelkimoRev FacuOdontol Porto Alegre 1986–1987 28/29:10-13. [Google Scholar]