Dermatofibrosarcoma Protuberans of Lumbar Region with Metastasis to Lung: A Rare Presentation
Anil Khurana1, Vijay Kumar J2, Paramjeet Kaur3, Ashok K Chauhan4, Gajender Singh5
1 Medical Officer, Department of Radiotherapy, Pt. BD Sharma, PGIMS, Rohtak, Haryana, India.
2 Junior Resident, Department of Radiotherapy, Pt. BD Sharma, PGIMS, Rohtak, Haryana, India.
3 Associate Professor, Department of Radiotherapy, Pt. BD Sharma, PGIMS, Rohtak, Haryana, India.
4 Senior Professor, Department of Radiotherapy, Pt. BD Sharma, PGIMS, Rohtak, Haryana, India.
5 Associate Professor, Department of Pathology, Pt. BD Sharma, PGIMS, Rohtak, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anil Khurana, Medical Officer, Department of Radiotherapy, Pt. BD Sharma, PGIMS, Rohtak, Haryana, India. E-mail : neelukhurana@gmail.com
Dermatofibrosarcoma protuberans (DFSP) is a cutaneous slow growing soft tissue sarcoma associated with a high local recurrence rate. Common site of presentation is trunk followed by proximal extremity and head and neck region. A case of recurrent DFSP of left lumbar region with metastasis in lung in a 50-year-old woman presented here. Absence of symptoms often leads to a delay in diagnosis. DFSP is often mistaken for other skin conditions, particularly in its early stages.
Chemotherapy, Cutaneous tumour, Recurrence, Soft tissue sarcoma
Case Report
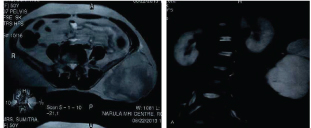
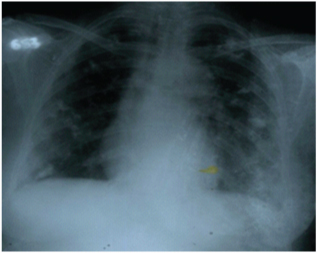
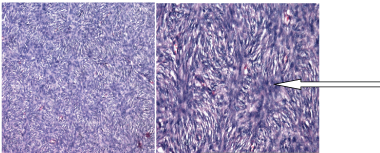
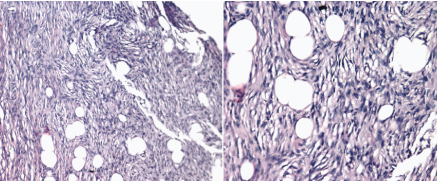
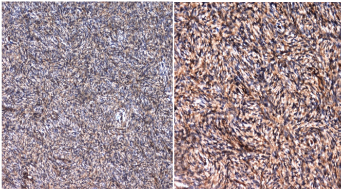
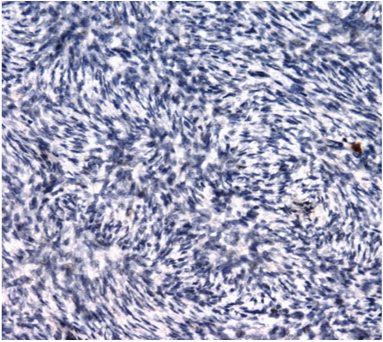
A 50-year-old female presented in Radiotherapy OPD, with an ulcerated growth in the left lumbar region associated with mild to moderate pain since one year. Patient had history of growth five year back at same site for which she underwent excision for five times in duration of five years last 11 months back of presentation. Her family, medical history was not significant. On examination, a multilobulated large well defined growth was present in the left lumbar region, measuring approximately 15 X 20 cm, with a variegated and irregular surface, fixed to underlying tissue and non tender on palpation [Table/Fig-1a,b]. Per abdomen examination was normal. There was no lymph node palpable in cervical, axillary or inguinal region. Blood investigations including renal function tests, liver function tests were normal. On serological examination patient was non reactive for Anti-HCV, HbsAg and HIV 1and 2. Ultrasonography of abdomen revealed a large heteroechoic lesion in left lumbar region with areas of necrosis at its upper pole, showing flow on color doppler seen at the site of growth and there was no lymphadenopathy. MRI abdomen revealed large soft tissue mass with lobulated margin, of size approximately 127 mm X 113 mm X 149 mm seen in subcutaneous plane of left posterior and left lateral aspect. The lesion appeared hypointense on T1W, of mixed intensity on T2W images and hyperintense on STIR images. It caused a compression effect on paraspinal and abdominal muscles. Scoliosis with convexity towards left side was also seen in lumbar region [Table/Fig-2a,b]. Chest X- ray revealed multiple non homogenous opacity in bilateral lung fields [Table/Fig-3]. With the above findings, a provisional radiological diagnosis of soft tissue mass was made. On histopathological examination epidermis was atrophied at places. Dermis revealed a tumour which reached the overlying epidermis and infiltrated subcutaneous tissue at places. Tumour was composed of oval to spindle shaped cells arranged in groups, fascicles storiform pattern [Table/Fig-4a,b] and moderate pleomorphism and few areas of haemorrhage, entrapment of fat cells [Table/Fig-4c,d] and necrosis were also seen. Immunohistochemistry of tumour was positive for vimentin [Table/Fig-5,6] and CD 34 [Table/Fig-7a,b] but negative for smooth muscle actin [Table/Fig-8]. Based on this histopathological findings and IHC markers diagnosis suggestive of Dermatofibrosarcoma protuberance was made. Due to size of the mass, the patient was given 20 Grays of external beam radiotherapy. Presently, the patient is on adjuvant chemotherapy consisting of vincristine, doxorubicin and cyclophosphamide regimen. Till date patient has completed six cycles of chemotherapy without any adverse events. The tumour and opacity in bilateral lung region reduced in size.
A multilobulated large well defined growth measuring approximately of size 15 X 20cm, with an irregular surface

MRI revealed large soft tissue mass lesion with lobulated margin in subcutaneous plane of left posterior and left lateral aspect. The compression effect is notable on paraspinal and abdominal muscles and scoliosis with convexity towards left side in lumbar region
Chest X- ray PA view revealed multiple non homogenous opacity in bilateral lungs
Photomicrograph showing fibroblasts arranged in storiform pattern (Loosely-arranged whorls of elongated, spindled fibroblast-like cells) (10X and 40X)
Photomicrograph showing entrapment of fat cells. (10X&20X)
Photomicrograph showing tumour cells which are positive for vimentin (400X) and Cells showing low proliferative index (Ki 67 200X) respectively

Photomicrograph showing tumour cells which are positive for CD 34 (CD 34 200X and 100X)
Photomicrograph showing tumour cells showing absence of smooth muscle antigen expression (SMA 200X)
Discussion
Dermatofibrosarcoma protuberans (DFSP) is a type of soft tissue sarcoma which is a locally invasive and slow growing tumour. It accounts for 0.01% of all malignancies and less than 0.1% of all the cutaneous neoplasms with reported incidence being 0.8 cases per million persons a year [1]. It is the most frequent cutaneous sarcoma [2]. The term Dermatofibrosarcoma protuberans was coined by Hoffman [3]. Trunk is the most frequently involved site which is involved in 42%-72%, second and third most frequently involved sites are proximal extremities (16% - 30%) and head and neck sites (10%- 16%) respectively. Breast is also rarely involved [4]. Metastasis from DFSP is rare which is in the range of 4-6% [5]. It is also popular for post surgical high recurrence rate similar to the present case [2]. DFSP initially present as a single, raised, red to bluish, firm cutaneous nodule; it is infiltrative in nature and invades the underlying fascia, muscles or bones. Lesion is often covered by a brown yellow, red tinged, sclerodermiform or teleangiectatic and atrophic skin similar to the present case [2]. On histopathological examination there is monomorphous proliferation of cytological bland spindle cells with a visible storiform or whorled (rushmat-like) architecture, low mitotic activity and deep, honeycomb infiltration into subcutaneous adipose tissue.
Diagnosis is made by deep subcutaneous punch biopsy or incisional biopsy and histological analysis to detect. CD 34 expression, MRI scan done for the purpose of preoperative planning to evaluate local extent of tumour and CT scan of the chest to evaluate distant metastasis CD 34 which is an IHC marker is extremely useful in the differentiation from benign fibrous histiocytoma, dermatofibroma and other soft tissue tumours. Sensitivity of CD 34 is from 84% to 100% [2]. Various treatment options includes: Moh’s micrographic surgery. Average recurrence rate of DFSP after Moh’s micrographic surgery is 0.6% (0% to 6.6%) and total recurrence rate is 1.6% [6].
Wide local excision is a surgical procedure in which diseased tissue is removed along with a margin of normal tissue. Diseased tissue obtained is processed for microscopic examination and graded which helps in further management. The incidence of local recurrence following wide local excision depends on length of surgical margins. Roses et al., studied 50 consecutive patients of DFSP patients and concluded that 2 cm or lesser than 2 cm are associated with local recurrence rate of 41% and surgical margins more than 2 cm are associated with local recurrence rate of 24%. Five year recurrence free survival at surgical margins at <1cm,≥=1cm,≥=2cm and ≥=3cm are 59%, 66%, 70%, and 80% respectively [7].
In a retrospective study, Arnaud EJ et al., analyzed the outcomes of 117 patients (mean age 39 years) treated surgically for a DFSP [8]. DFSP is a radio-responsive tumour and RT can be used preoperatively to increase the chance of resectability in selected inoperable cases and postoperatively with positive surgical margins and also in recurrent disease [9]. Dose of preoperative RT varies from 50-50.4 Gy and dose of postoperative RT is 60-66 Gy [10]. Preoperative radiation therapy is indicated in patients with who are at high risk for positive resection margins (patients with larger tumour size and tumour present near the critical structure) followed by surgical resection after an interval of 4-6 weeks. Postoperative RT is indicated in patients with close resection margins (dose of 60 Gy), microscopic positive margins (60-65 Gy) and in gross residual disease (65-75 Gy with field resection after 50 Gy) and it is also indicated in all patients with recurrent or high grade lesions regardless of margin status. Translocation between chromosomes 17 and 22 {t (17:22) (q22; q13)} resulting in COL1A1 PDGFB fusion is present in >95% of cases [11], which leads to the over expression of platelet derived growth factor receptor-beta so the drugs targeting this receptors are used as a clinical modality in treatment of DFSP [12].
Imatinib mesylate has been approved by the FDA and used in the adjuvant treatment in patients with unresectable, recurrent, or metastatic DFSP [13] with objective response rate approaching 50% [14]. U. S. Food and Drug Administration (FDA) granted approval to Imatinib Mesylate in 2006 (October 19) as a single agent for the treatment of DFSP, recommended dose is 800 mg/day. Kamar FG et al., mentioned the use of Sorafenib which is a tyrosine kinase inhibitor in patients with postoperative and post Imatinib failure with good response [2].
Conclusion
DFSP is a low grade cutaneous sarcoma having locally aggressive behavior and high recurrence rate. This study highlights the role of radiation therapy in radical and palliative setting and also highlights the use of Imatinib Mesylate in the management because of its good response rate.
[1]. Rajshri DP, Kishor SH, Nandkumar DV, Dhananjay NV, Giant dermatofibrosarcoma protuberans over an anterior chest wall: a rare case reportIndian J Pathol Oncol 2015 2(1):31-36. [Google Scholar]
[2]. Kamar FG, Kairouz VF, Sabri AN, Dermatofibrosarcoma protuberans (DFSP) successfully treated with sorafenib: case reportClin Sarcoma Res 2013 3(1):5 [Google Scholar]
[3]. Lemm D, Mugge LO, Mentzel T, Hoffken K, Current treatment options in dermatofirosarcoma protuberansJ Cancer Res Clin Oncol 2009 135:653-65. [Google Scholar]
[4]. Deb Roy A, Nishant K, Joshi D, Painful late recurrence of dermatofibrosarcoma protuberans of breast in a centurian femaleJournal of Clinical and Diagnostic Research 2013 7(10):2278-79. [Google Scholar]
[5]. Mendenhall WM, Zlotecki RA, Scarborough MT, Dermatofibrosarcoma protuberansCancer 2004 101(11):2503-08. [Google Scholar]
[6]. Gloster HM Jr, Harris KR, Roenigk RK, A comparison between Moh’s micrographic surgery and wide surgical excision for the treatment of dermatofibrosarcoma protuberansJ Am Acad Dermatol 1996 35(1):82-87. [Google Scholar]
[7]. Roses DF, Valensi Q, LaTrenta G, Harris MN, Surgical treatment of dermatofibrosarcoma protuberansSurg Gynecol Obstet 1986 162(5):449-52. [Google Scholar]
[8]. Arnaud EJ, Perrault M, Revol M, Servant JM, Banzet P, Surgical treatment of dermatofibrosarcoma protuberansPlast Reconstr Surg 1997 100(4):884-95. [Google Scholar]
[9]. Uysal B, Sager O, Gamsiz H, Cicek A, Demiral S, Dincoglan F, Evaluation of the role of radiotherapy in the management of dermatofibrosarcoma protuberansJ BUON 2013 18(1):268-73. [Google Scholar]
[10]. Castle KO, Guadagnolo BA, Tsai CJ, Feig BW, Zagars GK, Dermatofibrosarcoma protuberans: long-term outcomes of 53 patients treated with conservative surgery and radiation therapyInt J Radiat Oncol Biol Phys 2013 86(3):585-90. [Google Scholar]
[11]. Kérob D, Porcher R, Vérola O, Dalle S, Maubec E, Aubin F, Imatinib mesylate as a preoperative therapy in dermatofibrosarcoma: results of a multicenter phase II study on 25 patientsClin Cancer Res 2010 16(12):3288-95. [Google Scholar]
[12]. Labropoulos SV, Razis ED, Imatinib in the treatment of dermatofibrosarcoma protuberansBiologics 2007 1(4):347-53. [Google Scholar]
[13]. Johnson JH, Sherman W, Ratner D, Using imatinib as neoadjuvant therapy in dermatofibrosarcoma protuberans: potential pluses and minusesJ Natl Compr Canc Netw 2010 8(8):881-85. [Google Scholar]
[14]. Rutkowski P, Van Glabbeke M, Rankin CJ, Ruka W, Rubin BP, Debiec-Rychter M, Imatinib mesylate in advanced dermatofibrosarcoma protuberans: pooled analysis of two phase II clinical trialsJ Clin Oncol 2010 28(10):1772-79. [Google Scholar]