PNET of the Abdominal Wall: A Rare Presentation
Srikanth Soma1, Sunil Kumar Shetty2, Shriram Bhat3
1 Senior Resident, Department of General Surgery, Kasturba Medical College, Mangalore, Manipal University, India.
2 Associate Professor, Department of General Surgery, Kasturba Medical College, Mangalore, Manipal University, India.
3 Professor, Department of General Surgery, Kasturba Medical College, Mangalore, Manipal University, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Srikanth Soma, B-404, Amsri Residency, Ameerpet, Hyderabad, Telangana-500016, India. E-mail : soma_986@yahoo.co.in
Primitive neuroectodermal tumours (PNETs) are a malignant group of neoplasms and are neuroectodermal in origin. In most large series published to date, peripheral primitive neuroectodermal tumours usually present in the second decade of life, with a slight male preponderance. Those which occurs peripherally resemble soft tissue sarcomas. Peripheral PNET is rare in presentation and of which only few cases involving the soft tissues of the abdominal wall have been reported. We present a case affecting a young female who presented to us with a progressively enlarging swelling involving the anterior abdominal wall. She underwent wide excision followed by adjuvant therapy based on final histopathology report.
Extraskeletal, Immunohistochemistry, Soft tissue tumour, Surgery
Case Report
A 21-year-old lactating female presented to us with a swelling over the left anterior abdominal wall since 2 months. She had noticed the swelling 15 days post normal vaginal delivery and has been progressing in size since then. There were no other symptoms of note. No history of previous surgeries in the past. Normal obstetric history and no associated comorbid illness. No significant family history.
A solitary non tender swelling measuring 6 × 4 cm was palpable 3 cm lateral to the umbilicus to the left side of the abdomen. Swelling had regular margins and was firm in consistency. Skin over the swelling and surrounding area being normal.
All the routine blood work was normal. Contrast enhanced computerized tomography (CECT) of the abdomen and pelvis revealed a well defined rounded in homogenous intensity mass lesion with non enhancing area within the muscular plane in the para umbilical region – suggestive of soft tissue tumour of the anterior abdominal wall.
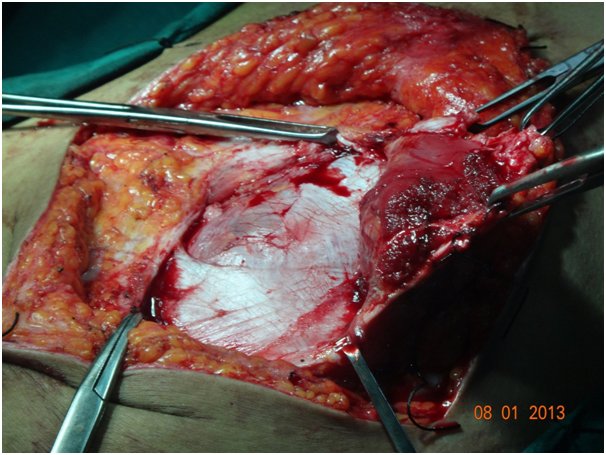
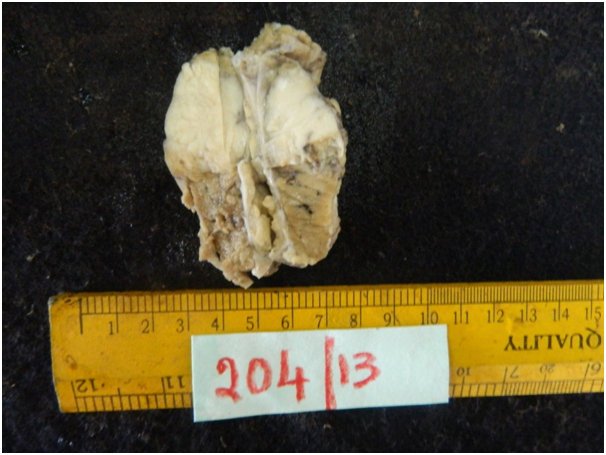
The patient underwent wide local excision of the tumour [Table/Fig-1,2].
Intraoperative photograph showing the surgical excision of the tumour with wide margins within the soft tissue of abdominal wall
Gross specimen of the tumour after its removalGross specimen of the tumour after its removalGross specimen of the tumour after its removalGross specimen of the tumour after its removal
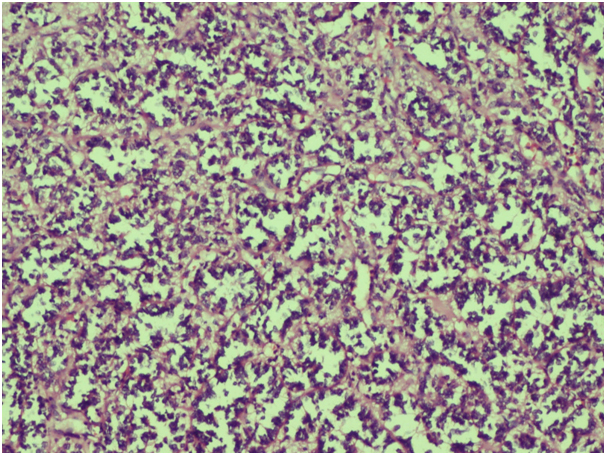
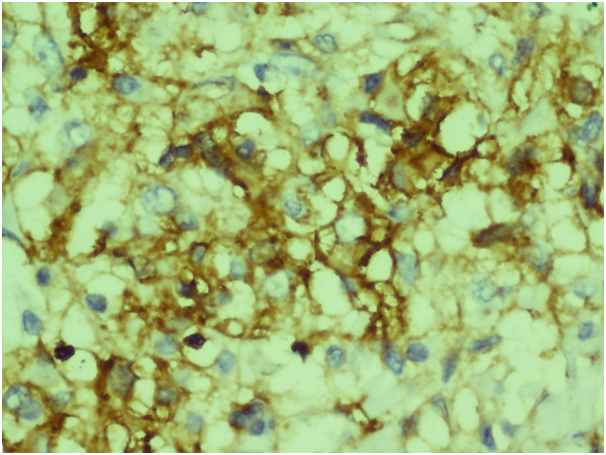
Histopathology showed tumour tissue composed of small round cells with fine to clear chromatin and inconspicuous nucleoli. The cells were arranged in alveolar like pattern having thick fibrous septae [Table/Fig-3]. Large areas of necrosis were evident. Immunohistochemistry showed strong positivity for CD 99 [Table/Fig-4] and vimentin. The microscopic findings and immunochemistry were consistent with the spectrum of primitive neuroectodermal tumours (PNETs).
Tumour tissue composed of small round cells with fine to clear chromatin and inconspicuous nucleoli. The cells were arranged in alveolar like pattern having thick fibrous septae
Immunohistochemistry showing strong positivity for CD 99
CT chest was normal. No other significant abnormalities were seen. Whole body bone-scan showed no evidence of bony metastases. She was referred to oncology department and was advised adjuvant therapy with vincristine, doxorubicin and cyclophosphamide although the lesion was completely excised with adequate margins. The patient has been on regular follow up and disease free since last 6 months.
Discussion
Primitive neuroectodermal tumours (PNETs) are malignant tumours of neuroectodermal origin and are composed of small round cells.
The first description of PNETs was made by Stout in the year 1918 and was thought to originate from the nervous tissue [1]. PNETs are classified as members of the Ewing’s sarcoma family of tumours. Common to all these neoplasms - exhibit a neural phenotype and express the MIC2 protein (CD 99), and similar chromosomal translocation between chromosomes 11q24 and 22q12 are observed in majority of cases [2].
Batsakis et al., classified the primitive neuroectodermal tumour (PNET) family of tumours into 3 groups [3]: PNETs arising from the central nervous system, those arising from the autonomic nervous system and the peripheral PNETs (pPNETs).
The tumours are classified under pPNETs include Ewings sarcoma [4], Malignant pPNETs or peripheral neuroepith-elioma and Askin tumour.
In most large series published to date, PNETs usually present in the second decade of life, with a slight male preponderance. They account for 4-17% of all paediatric soft tissue tumours [5].
The most common sites of presentation for pPNET metastases include the lung, bone marrow and bone. Imaging manifestations of peripheral PNETs are nonspecific, which includes large soft tissue mass with cystic and necrotic areas with heterogeneous enhancement after intravenous administration of contrast materials. Histopathologically, PNETs are highly cellular with sheets of small round cells with their nuclei being hyperchromatic.
Kushner et al., in a review of Memorial Sloan-Kettering’s experience with pPNET, reported a similarly dismal 25% progression-free survival rate at 2 years in patients with only localized disease [6]. Other large series, however, reported somewhat better survival rates in patients with localized disease, with 2 large trials showing 2 years and 3 years survival rates of 65% and 56%, respectively [7,8].
Surgical resection is the preferred initial intervention if diagnosed early followed by adjuvant therapy. Multimodality treatment is advocated to prevent metastatic disease, recurrent disease and to treat residual tumour after resection. Carvajal and Meyers, in a comprehensive review of the chemotherapeutic regimens in the treatment of PNETs recommended a regimen that included vincristine, doxorubicin, and cyclophosphamide with ifosfamide and etoposide [9]. The treatment of metastatic disease similarly includes chemotherapy as well as radiotherapy to all sites of gross disease with surgical excision, where possible.
There have been a number of case reports published for pPNETs involving the maxillary-facial regions [10,11], extremities [12], gynaecological organs [13] and intraabdominal sites [14,15]. Very few reports specifically involving abdominal subcutaneous wall have been reported and most have been in children [16,17] and one in a 60-year-old female [18]. PNETs are a rare form of tumours and this case demonstrates an unusual and rare presentation of a PNET in the abdominal wall of an adult.
Conclusion
Peripheral PNET arising from soft tissues is extremely rare. Although its radiological features are non-specific, it should be kept in mind in the differential diagnosis of soft tissue tumours in young people. Early diagnosis combined with surgical intervention and adjuvant therapy at an earlier stage is the best way possible to provide prolonged disease free interval for patients diagnosed with these tumours as demonstrated in this case.
[1]. Stout AP, A tumour of the ulnar nerveProc NY Pathol Soc 1918 18:2-11. [Google Scholar]
[2]. De Alava E, Gerald WL, Molecular biology of the Ewing’s sarcoma/primitive neuroectodermaltumour familyJ ClinOncol 2000 18(1):204-13. [Google Scholar]
[3]. Batsakis JG, Mackay B, el-Naggar AK, Ewing’s sarcoma and peripheral primitive neuroectodermal tumour: an interim reportAnn Otol Rhinol Laryngol 1996 105(10):838-43. [Google Scholar]
[4]. Castro E, Parwani A, Ewing Sarcoma/Primitive NeuroectodermalTumor of the Kidney: Two Unusual Presentations of a Rare TumorCase Reports in Medicine 2012 2012:1-7. [Google Scholar]
[5]. Windfuhr JP, Primitive neuroectodermal tumour of the head and neck: incidence, diagnosis, and managementAnn Otol Rhinol Laryngol 2004 113(7):533-43. [Google Scholar]
[6]. Kushner BH, Hajdu SI, Gulati SC, Erlandson RA, Exelby PR, Lieberman PH, Extracranial primitive neuroectodermal tumours. The Memorial Sloan-Kettering cancer center experienceCancer 1991 67(7):1825-29. [Google Scholar]
[7]. Jones JE, McGill T, Peripheral primitive neuroectodermal tumours of the head and neckArch Otolaryngol Head Neck Surg 1995 121(12):1392-95. [Google Scholar]
[8]. Jürgens H, Bier V, Harms D, Malignant peripheral neuroectodermal tumours. a retrospective analysis of 42 patientsCancer 1988 61(2):349-57. [Google Scholar]
[9]. Carvajal R, Meyers P, Ewing’s sarcoma and primitive neuroectodermal family of tumoursHematol Oncol Clin North Am 2005 19(3):501-25.:vi-vii. [Google Scholar]
[10]. Ozer E, Kanlikama M, Karakurum G, Sirikci A, Erkilic S, Aydin A, Primitive neuroectodermal tumour of the mandibleInt J Pediatr Otorhinolaryngol 2000 65:257-61.doi: 10.1016/S0165-5876(02)00183-0 [Google Scholar]
[11]. Alobid I, Bernal-Sprekelsen M, Alos L, Benitez P, Traserra J, Mullol J, Peripheral primitive neuroectodermal tumour of the left maxillary sinusActaOtolaryngol 2003 123:776-78.doi: 10.1080/00016480310001213 [Google Scholar]
[12]. Jayakumar S, Jatavalabulla S, Miller IM, Peripheral neuroectodermal tumour of the hand in an adultJ Hand SurgEur 2007 32:460-61.doi: 10.1016/j.jhse.2007.04.001 [Google Scholar]
[13]. Pauwels P, Ambrose P, Hattinger C, Lammens M, Dal Cin P, Ribot J, Peripheral primitive neuroectodermal tumour of the cervixVirchows Arch 2000 436:68-73.doi: 10.1007/PL00008201 [Google Scholar]
[14]. Sethi B, Smith GT, Primitive neruoectodermal tumours arising in the small bowelHistopathology 2007 50:665-66.doi: 10.1111/j.1365-2559.2007.02631.x [Google Scholar]
[15]. Alvarez-Laso C, Azcano E, Gonzalez J, Gonzalez-Pinto I, Primitive neuroectodermal tumour of the retroperitoneumClin Transl Oncol 2008 10:380-82.doi: 10.1007/s12094-008-0217-16 [Google Scholar]
[16]. Taylor GB, Chan YF, Subcutaneous primitive neuroectodermal tumour in the abdominal wall of a child: long-term survival after local excisionPathology 2000 32:294-98.doi: 10.1080/713688937 [Google Scholar]
[17]. Somers GR, Shago M, Zielenska M, Chan HS, Hgan BY, Primary subcutaneous primitive neuroectodermaltumour with aggressive behaviour and an unusual karyotype: case reportPediatr Dev Pathol 2004 7:538-45.doi: 10.1007/s10024-004-2024-6 [Google Scholar]
[18]. Betal D, Shaygi B, Babu R, Jamil K, Sainsbury RJ, Primitive Neuroectodermal Tumour (PNET) in subcutaneous abdominal wall: a case reportInt Semin Surg Oncol 2009 6:10 [Google Scholar]