Catamenial Pain in Umbilical Hernia with Spontaneous Reduction: An Unusual Presentation of a Rare Entity
Divya Pandey1, Ritu Sharma2, Sudha Salhan3
1 Assistant Professor, Department of Obstetrics and Gynaecology, NDMC Medical College, Hindu Rao Hospital, Delhi, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, NDMC Medical College, Hindu Rao Hospital, Delhi, India.
3 Professor and Unit Head, Department of Obstetrics and Gynaecology, NDMC Medical College, Hindu Rao Hospital, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Divya Pandey, R-4/26, Rajnagar, Ghaziabad-201001, Uttar Pradesh, India.
E-mail: dr_devya1@yahoo.co.in
Spontaneous umbilical endometriosis occurring in absence of any previous abdominal or uterine surgery is extremely atypical. Its association with umbilical hernia is very rare and hernia getting spontaneously resolved has not been reported in literature so far. Here we report a case of a patient with spontaneous umbilical endometriosis associated with umbilical hernia which led to spontaneous hernia reduction. This was also associated with multiple uterine fibromyoma and bilateral ovarian endometrioma which were simultaneously treated by total abdominal hysterectomy with bilateral salpingo-oopherectomy along with surgical excision of the endometriotic tissue and repair of the abdominal wall defect. To the best of our knowledge, this is the first described case of spontaneous umbilical hernia reduction due to development of endometriosis.
Hernia reduction, Primary umbilical endometriosis, Primary umbilical hernia, Villar’s Nodule
Case Report
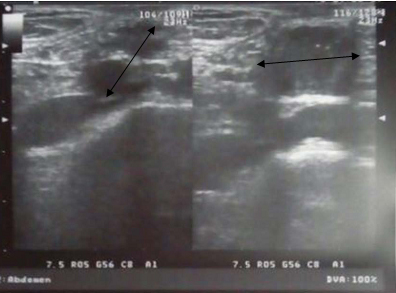
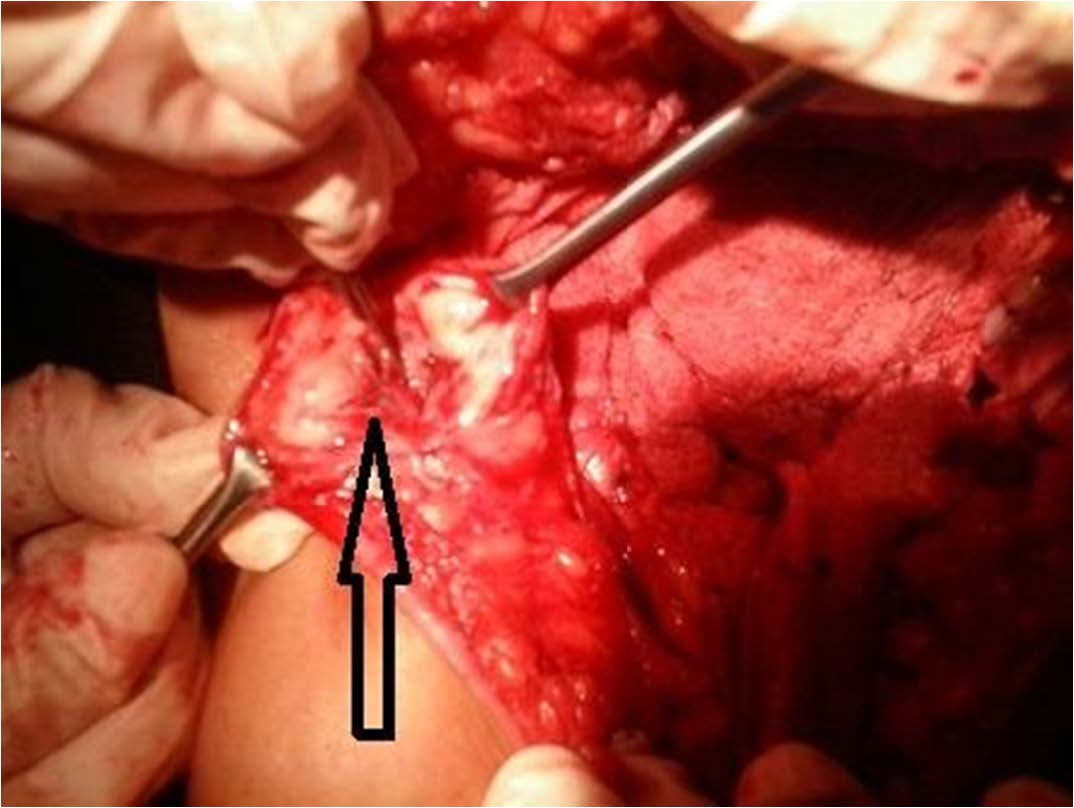
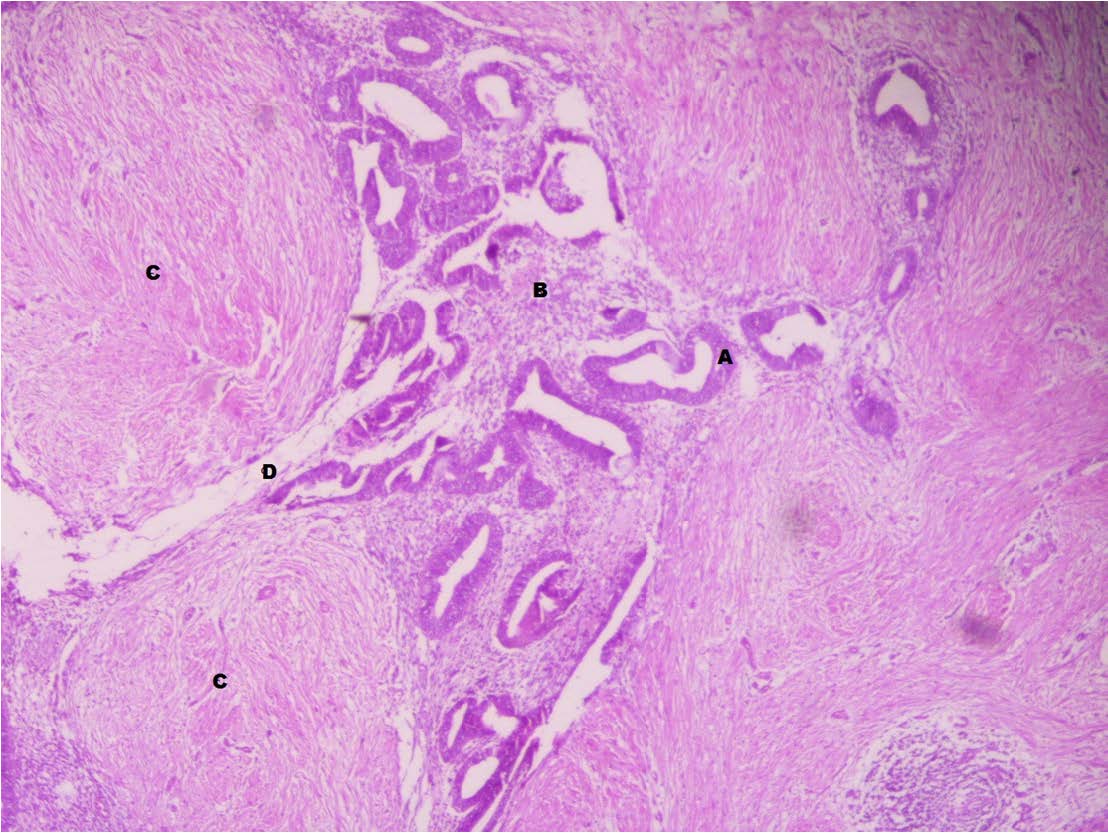
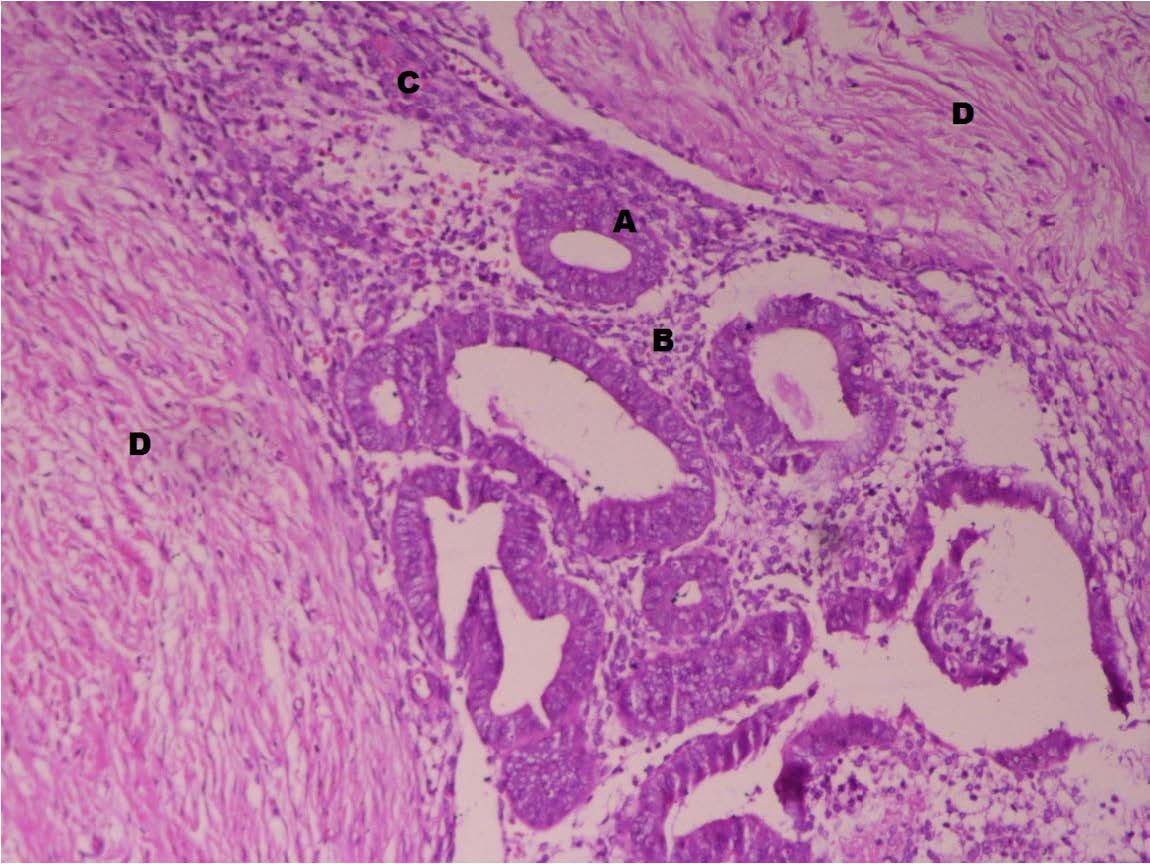
A 47 years old P2L2 women with previous two normal deliveries but without prior history of any abdomino-pelvic surgery presented in Out Patient Department of Obstetrics and Gynaecology of North Delhi Municipal Corporation Medical College, Delhi, India, with chief complaints of cyclical umbilical pain for four months along with menorrhagia and severe congestive dysmenorrhoea. There was history of umbilical swelling with dragging sensation, for one year which increased on activities raising the intra abdominal pressure and was reducible, suggestive of umbilical hernia. There was history of chronic constipation. A 5 months old ultrasound report showed multiple fibroids, bilateral chocolate cysts and umbilical hernia [Table/Fig-1]. With the onset of super imposed cyclical umbilical pain, the umbilical swelling gradually subsided over last 5 months. On abdominal examination, there was supra-pubic mass corresponding to 14 weeks gravid uterus. The umbilicus was absolutely normal on inspection. On palpation, periumbilical induration was present but there was no impulse on coughing. Pelvic examination showed a 14 weeks size, irregularly enlarged, firm, non-tender uterus with restricted mobility along with bilateral, cystic, tender masses of about 5x5 cm each suggestive of ovarian cysts. Posterior fornix was also full. After informed consent she was thus thoroughly evaluated. The latest ultrasound suggested multiple intramural fibromyomas largest being 7.5x7.9 cm along with bilateral ovarian endometrioma. Serum CA-125 was 46.8 IU/ml. Endometrial biopsy showed simple hyperplasia without atypia. In view of symptomatic fibroid and bilateral endometrioma at 47 years age, patient was planned for laparotomy along with total hysterectomy with bilateral salpingo-oopherectomy. Per-operative findings were a 14 weeks uterus with multiple intramural fibroids and bilateral endometrioma 5x5 cm each, densely adherent to the gut. Just beneath the umbilicus there was about 3x3 cm firm nodule [Table/Fig-2] with chocolate fluid and fibro fatty glandular tissue extending and infiltrating through the fascial planes till the rectus sheath defect of about 3x3 cm. Total abdominal hysterectomy with bilateral salpingo-oopherectomy [Table/Fig-3] along with wide excision (with 1 cm margin) of umbilical nodule and mesh repair of the abdominal wall defect was done. The histopathology of excised nodule confirmed endometrioma [Table/Fig-4,5 and 6]. The patient was completely asymptomatic and CA-125 regressed to normal at follow up.
A 3x3 cm parietal wall defect (black arrow) seen in anterior abdominal wall at the umbilical region with evidence of bowel herniating through it
Intraoperative picture showing the location and extent of umbilical endometriosis
Specimen of uterus with multiple fibroids with bilateral tubes and both ovaries with Endometriotic cysts

Scanner View (with 40X magnification) of excised umbilical nodule showing endometrial glands (A) with stroma (B) among fibrous tissue (C) and adipose tissue (D) {H & E Stain}.
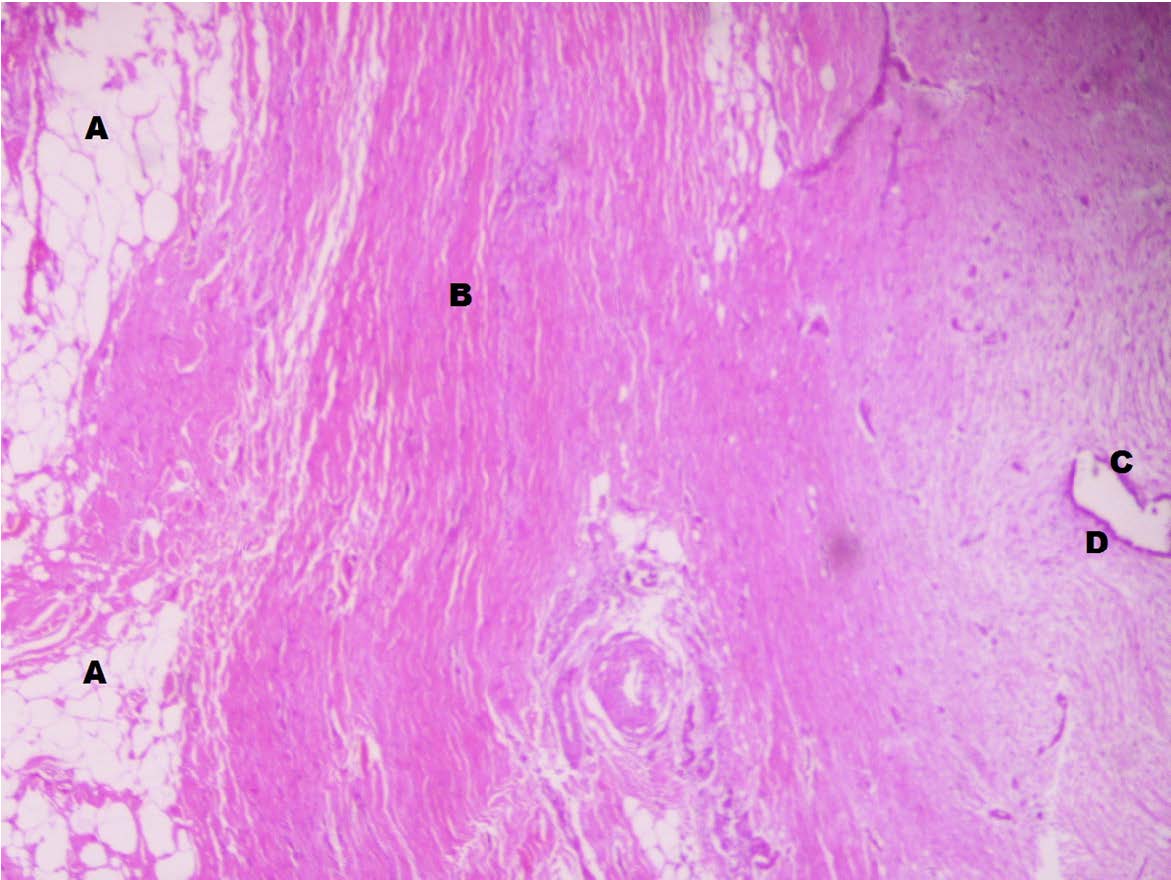
Low Power Microscopic view (with 100 X magnification), from excised umbilical nodule showing magnified endometrial glands (A), stroma (B) and haemorrhage (C) interspersed among fibrous tissue (D) {H & E Stain}
Scanner view (with 40X magnification) of section from the same excised nodule from umbilicus which shows adipocytes (A), fibrous tissue (B), Endometrial gland (C) and surrounding stroma(D) in same field {H & E Stain}
Discussion
Endometriosis is a ubiquitous disease affecting pelvic and extra-pelvic sites. Umbilical endometriosis is a rare entity, with incidence of 0.5 to 1% of all patients with endometriosis [1]. Its development usually follows laparoscopic surgical procedures involving the umbilicus [2]. Only 122 cases of spontaneous umbilical endometriosis have been reported by Victory R et al., over period of 1996 to 2007 [3]. After thorough literature search using MeSH terms “umbilicus”, “endometriosis” and “hernia” on Pubmed from 1900 to 2014 retrieved only 4 cases of endometriosis associated within umbilical hernia [4–7]. But umbilical hernia getting spontaneously resolved due to underlying endometriosis have not been reported in literature so far.
Through this case we have described our experience of a patient with umbilical hernia with cyclical pain at hernia site which regressed spontaneously owing to underlying umbilical endometriosis. This was associated with pelvic endometriosis and multiple uterine fibromyomas.
As far as, development of adult umbilical hernia is concerned, multiparity and chronic increased abdominal pressure leading to disruption of linea alba, are the known predisposing factors, which were there in our case too. As this can lead to strangulation or incarceration, repair is needed which can be done either by conventional Mayo’s method using non absorbable material without mesh or repair using Mesh. Due to high recurrence rates with conventional approach, Mesh repair is preferred and recommended. In our case, the spontaneous reduction although masked the hernia problem but afflicted her to a still more embarrassing problem of excruciating cyclical umbilical pain because of underlying endometriosis.
Development of primary umbilical endometriosis takes into account the two mentioned etiological theories. The first is haematogenous or lymphatic spread theory, based on the fact that lymphatic vessels join the peritoneal cavity to umbilicus along the obliterated umbilical vessels. Migration of pelvic contents in umbilicus has been demonstrated by Scott who injected dye in pelvic cavity and retrieved it from umbilicus [8]. The extra pelvic endometriosis has also been explained by the Metaplasia theory, which suggests that multipotent cells can develop into endometrial tissue, often stimulated by inflammation. Alternatively it may develop through metaplasia of urachal remnants. In our case there were concomitant pelvic and extra pelvic (umbilical) diseases which can be attributed to, convincingly by these two theories.
The preoperative work-up of women with history suggestive of abdominal wall endometriosis include trans abdominal ultrasound with ultrasound guided fine-needle aspiration biopsy preferably and cytological analysis, and computed tomography (CT) [9]. In our case ultrasound was done which suggested the umbilical endometriosis with multiple fibroids and bilateral endometrioma with umbilical hernia.
Though medical treatment with hormone therapy can be considered, treatment of choice for these patients should be surgical excision. Various superficial surgical approaches like thermo coagulation or omphalectomy can lead to relapse, so treatment should be by excisional surgery to avoid disease relapse, recurrence and risk of oncogenic transformation [10].
Luigi Fedele et al., and Mechsner et al., suggested systematic use of laparoscopy which aids in adequate excision of umbilical lesion, accurate reconstruction of the fascial and sub fascial plane and gives opportunity to surgeons to identify and eventually treat concomitant pelvic disease [11,12]. Thus it calls for radical excisional surgery, ideally with laparoscopic assisted approach leading to complete and long term disease free follow up. In our case, laparotomy with wide excision of umbilical endometriosis and mesh repair of anterior abdominal wall defect was completed with total abdominal hysterectomy with bilateral salpingo-oopherectomy which remains universal treatment of choice in this age group patient for pelvic endometriosis. Mesh repair of the defect was sought to, as conventional repair has high chances of recurrence [13].
Spaziani et al., suggested that surgery should be performed in the first 3-4 days of follicular phase to minimize the risk of diffusion of endometriotic cells. Moreover there should be wide excision to prevent local recurrence [14].
Our case was unique in its presentation where there was spontaneous reduction of umbilical hernia owing to underlying endometriosis. The inflammation and fibrosis associated with endometriosis led to the spontaneous closure of the hernial hiatus which was about 3x3 cm rectus sheath defect in the anterior abdominal wall.
Conclusion
Umbilical endometriosis is a very rare disease, but should be considered in the differential diagnosis of umbilical lesions. The clinicians should be sensitized that umbilical endometriosis can coexist with the umbilical hernia especially when patient has history of spontaneous regression of hernia and cyclical umbilical pain. The diagnosis is clinico-radiological and calls for complete excision of pelvic and extra pelvic disease along with co-morbid uterine conditions (multiple fibroids in this case). Abdominal wall defect is to be identified and repaired concomitantly.
[1]. Chatzikokkinou P, Thorfinn J, Angelidis IK, Papa G, Trevisan G, Spontaneous endometriosis in an umbilical skin lesionActa Dermatovenerol Alp Pannonica Adriat 2009 18(3):126-30. [Google Scholar]
[2]. Goldberg JM, Bedaiwy MA, Recurrent umbilical endometriosis after laparoscopic treatment of minimal pelvic endometriosis: a case reportJ Reprod Med 2007 52(6):551-52. [Google Scholar]
[3]. Victory R, Diamond MP, Johns DA, Villar’s Nodule: A case report and systematic literature review of endometriosis externa of umbilicusJ Minim Invasive Gynecol 2007 14(1):23-32. [Google Scholar]
[4]. Stojanovic M, Radojkovic M, Jeremic L, Zlatic A, Stanojevic G, Janjic D, Umbilical endometriosis associated with large umbilical hernia. Case reportChirurgia (Bucur) 2014 109(2):267-70. [Google Scholar]
[5]. Ramsanahie A, Giri SK, Velusamy S, Nessim GT, Endometriosis in a scarless abdominal wall with underlying umbilical herniaIr J Med Sci 2000 169(1):67 [Google Scholar]
[6]. Lovino F, Ruggiero R, Irlandese E, Gili S, Lo Schiavo F, Umbilical endometriosis associated with umbilical hernia. Management of a rare occuranceChir Ital 2007 59(6):895-99. [Google Scholar]
[7]. Yuen JS, Chow PK, Koong HN, Ho JM, Girija R, Unusual sites (thorax and umbilical hernial sac) of endometriosisJ R Coll Surg Edinb 2001 46(5):313-15. [Google Scholar]
[8]. Scott RB, Nowak RJ, Tindale RM, Umbilical endometriosis and the Cullen sign. Study of lymphatic transport from pelvis to umbilicus in monkeysObstet Gynecol 1958 11(5):556-63. [Google Scholar]
[9]. Savelli L, Manuzzi L, Di Donato N, Salfi N, Trivella G, Ceccaroni M, Endometriosis of the abdominal wall: ultrasonographic and doppler charactersticsUitrasound Obstet Gynecol 2012 39(3):336-40. [Google Scholar]
[10]. Lauslahti K, Malignant external endometriosis. A case of adenocarcinoma of umbilical endometriosisActa Pathol Microbiol Scand. Suppl 1972 233:98-102. [Google Scholar]
[11]. Fedele L, Frontino G, Bianchi S, Borruto F, Ciappina N, Umbilical endometriosis: a radical excision with laparoscopic assistanceInt J Surg 2010 8(2):109-11.doi: 10.1016/j.ijsu.2009.11.006. Epub 2009 Nov 24 [Google Scholar]
[12]. Mechsner S, Bartley J, Infanger M, Loddenkemper C, Herbel J, Ebert AD, Clinical management and immunohistochemical analysis of umbilical endometrioisArch Gynecol Obstet 2009 280(2):235-42.doi: 10.1007/s00404-008-0900-4. Epub 2008 Dec 31 [Google Scholar]
[13]. Halm JA, Heisterkamp J, Veen HF, Weidema WF, Long term follow up after hernia repair. Are there risk factors for recurrences after simple or mesh repair?Hernia 2005 9(4):334-37.Epub 2005 [Google Scholar]
[14]. Spaziani E, DiFilippo A, Picchio M, Briganti M, DeCristofano C, Ceci F, Umbilical primary endometrioma-Case reportG Chir 2009 30(5):230-33. [Google Scholar]