Root fracture has been defined as a fracture involving dentin, cementum, pulp and periodontal ligament. Depending on the level of the fracture line various treatment modalities may be employed by the clinician to promote healing. The following case reports highlight how changes in technique allow for conservative management of horizontal root fractures at different levels. This approach allows the patient to retain their natural dentition at an affordable cost and provide a viable alternative to the use of more invasive and expensive alternatives. These patients presented with complaints of pain and mobility in upper front tooth region following trauma. Diagnosis was confirmed on the basis of intra-oral periapical radiographs following which non-surgical root canal treatment was performed.
Dental trauma, Intra-radicular splint, Treatment, Vital
Case Report- I
A 29-year-old female presented to the Department of Conservative Dentistry and Endodontics with chief complaint of pain, swelling and mobility (grade II) in upper right front tooth (11) following traumatic injury one day back. Clinically, 11 appeared to be displaced occlusally and was tender on percussion and palpation [Table/Fig-1a,b]. An occlusal radiograph showed slight Bucco-lingual displacement. An IOPAR showed the level of the fracture was at the junction of middle and apical one third. Repositioning of the coronal segment with finger pressure under local anaesthesia was done. The reduction was confirmed radiographically [Table/Fig-1b,c]. A non-rigid composite- twisted ligature wire splint was placed. The tooth was relieved from occlusion and access was established under rubber dam using split dam technique. Emergency pulp extirpation was done using barbed broach and 3% NaOCl. The apical fragment could not be negotiated using endodontic files. Working length was determined radiographically at 18 mm at the apical most end of the coronal fragment. Following which access was restored with Cavit (3M ESPE, St Paul, Minnesota, USA). Cleaning and shaping was done for the coronal fragment via conventional technique. Obturation was done using lateral cold compaction with gutta percha (META, Horsham, USA) and AH plus (Dentsply, York, USA) [Table/Fig-1d]. Gentle tooth brushing, rinsing with chlorhexidine mouthwash, soft diet and avoidance of chewing on the upper incisor were recommended. The splint was retained for 12 weeks. On 12 months recall the patient was asymptomatic [Table/Fig-1e].
Pre- treatment photograph - shows occlusal displacement of 11

Post splinting photograph –shows wire and composite splint

Pre-treatment radiograph- Cropped occlusal radiograph shows mid-root fracture
Post-obturation radiograph-Following obturation of coronal fragment

Follow up radiograph - At 12 months shows no periapical changes
Case Report- II
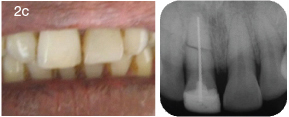
A 55-year-old patient presented with chief complaint of fractured and discoloured maxillary left central incisor (21). History of road traffic accident 5 years ago was reported. No history of pain, swelling or pus discharge was reported. On examination 21 elicited grade I mobility and Ellis class III fracture was present. Multiple angulated IOPA radiographs showed presence of a horizontal mid root fracture with minimal displacement of fractured fragments. [Table/Fig-2a]. Periapical rarefaction was noted. Due to the poor prospective crown by root ratio, root canal followed by placement of porcelain veneer crown was ruled out. The patient was unwilling for extraction and could not afford single tooth implant or fixed partial denture. It was decided to attempt intra-radicular splinting. In the first appointment cleaning and shaping was done till the apex upto size 60 K file (DENTSPLY, York, USA) via conventional technique. Calcium Hydroxide (Metapex, Chungcheongbuk-do, Korea) intracanal medicament was placed and access was temporised with Cavit (DENTSPLY, York, USA). The patient was recalled after two weeks .A sterile 70 K file was placed upto working length. Snug fit of the instrument was assessed and optimal length (2 mm beyond reference point) was determined. The instrument was weakened at this level using Diamond disk (Horico Diamante, Berlin, Germany). It was then replaced within the canal and turned clockwise, until a snug fit was obtained due to binding of the flutes into the dentin [Table/Fig-2b]. The file separated at the weakened area following which, vertical compaction of gutta-percha was done for the apical half. A file was chosen rather than a fibre post due to its higher flexibility and rigid nature allowing passage from coronal to apical fragment. The remainder of the canal was acid etched and restored with composite resin (Tetric-flow, Ivoclar- Vivadent, Zurich, Germany). Coronal labial direct composite veneer like preparation was done and tooth was restored using micro-hybrid composite resin (Aaesthet- X, DENTSPLY, USA). Finishing and polishing was done using Soflex discs (3M ESPE, St Paul, Minnesota, USA) and an IOPA was taken [Table/Fig-2c]. At 12 month recall visit patient was asymptomatic and no mobility or periapical changes were noted [Table/Fig-2d].
Pre-operative clinical photograph and radiograph-Shows fracture wrt 21
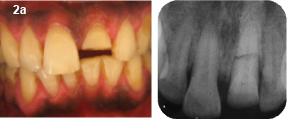
Mid treatment clinical photograph and radiograph- shows intra-radicular splint
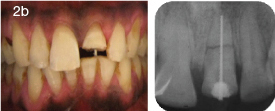
Post treatment clinical photograph and radiograph following composite restoration
Recall photograph and radiograph at 12 months

Case Report- III
A 30-year-old female patient reported with chief complaint of loosened upper anterior following fall two days back. No history of pain was reported. On examination right maxillary central incisor (11) with grade I mobility was slightly extruded. IOPAR was taken at 45, 90, 110 degrees and showed presence of horizontal root fracture [Table/Fig-3a]. Semi rigid splinting using composite and NiTi wire (1725) was done following which a radiograph was taken to confirm the position of the fractured fragments [Table/Fig-3b]. The tooth was relieved from occlusion. The patient was recalled after three weeks. The tooth responded positively to heat (Elements Obturation Unit, Sybron Endo, Calirfornia, USA), cold (Hygenic® Endo Ice, Coltene Whaledent, Ohio, USA,) and Electric sensibility testing (Gentle-Pulse”, Parkell inc, Edgewood, NY, USA). At three months recall patient reported no signs of pain or swelling. The splint was removed after six months. The follow up radiograph showed no periapical changes. The fracture line was clearly visible but no rounding of edges was noted indicating that healing may have occurred by bone and connective tissue deposition [Table/Fig-3]. Vitality was reassessed at three months, six months and one year using all three techniques [Table/Fig-3c].
Multiple angulated pre-operative radiograph indicating presence of horizontal root fracture


Recall radiograph at 12 months

Discussion
Trauma, causing damage to tooth structure frequently leads an individual to seek dental care. The occurrence of root fracture in permanent dentition is relatively rare (0.5-7%) [1]. It is broadly divided into horizontal and vertical root fractures. Horizontal root fracture refers to the presence of a fracture line that is perpendicular to the long axis of the tooth’s root [2]. The aim of this case series is to present a conservative approach to the management of horizontal root fractures to allow for retention of natural dentition.
Clinical management of root fracture depends on pulp vitality, occlusion and the level of the fracture line, degree of mobility and displacement of fractured element [3]. The most common types of root fractures are in the middle third of the root (57%), followed by fracture in the apical third (34%), and in the coronal part [4]. Radiographic examination is essential to diagnose the presence, extent and level of the fracture line and to differentiate it from luxation injuries. A non-rigid splint is placed for varying durations of time for stabilisation [5].
This case series focussed on maxillary central incisors as these are believed to be the most vulnerable to injury, sustaining approximately 80% of all dental injuries [6]. This may be due to their prominent placement in the oral cavity.
The healing of fractured roots showed various patterns which may be desirable such as healing with interposition of calcified tissue or, undesirable like the outgrowth of granulation tissue caused by infected or necrotic pulp. Other possible modalities include interposition of bone and connective tissue (seen as a clear separation of the two fragments) or the interposition of connective tissue (peripheral rounding of the fractured ends) [7,8].
Authors state that partial immobilisation (semi-rigid splinting) and adequate relief from occlusal loading is essential for successful management of root fractures. Most advocate a splinting duration of 2-4 weeks for cases of root fracture [3]. Intra-radicular splinting may be additionally required for repositioning and stabilising the fractured fragments [9]. Others’ have claimed that a longer duration of splinting following root fracture in vital teeth would additionally allow for maintenance of vitality [7,10]. The traumatised neurovascular system and periodontium would re-establish in this prolonged duration of splinting. Monitoring the vitality status of the tooth over time is indicated. Follow up of upto a year is advocated [10].
Different authors have advocated varying approaches for management of horizontal root fractures from elective root canal treatment for preserving the vitality of the tooth. Some authors advocate surgical removal of non-vital apical fragment while others advocate retention of vital ones [1,7,8]. Each technique is best suited to different clinical situations.
In the first case the level of the fracture line (junction of apical and middle third), difficulty in negotiating the apical fragment and an intact periodontal ligament space encouraged us to leave the apical fragment untouched. Studies have shown that such apical fragments rarely undergo pulp necrosis and can be left undisturbed [7]. Orthograde MTA placement was not attempted due to difficulty in negotiating the narrow canal with MAP system (Dentsply Tulsa, USA) and snug fit achieved with standardized gutta-percha. Follow up radiographs show clear demarcation of the fracture line indicating that healing may occur by formation of bone and connective tissue [7,8]. No periapical radioluscency was noted indicating that apical fragment may have retained its vitality.
In the second case an alternate splinting approach was used (intra-radicular) which allowed to improve crown by root ratio as the flexible file could negotiate the displaced apical fragment. Previous study with long term follow up shows good results with the use of stainless steel instruments [9]. Follow up radiographs show complete resolution of periapical rarefactions and a well-defined fracture line.
A longer duration of splinting and preserving the vitality of the pulp in the third case allowed the patient to remain asymptomatic while returning the tooth to its original position [7,10]. No signs of necrosis were noted at follow up visits. The sensibility values remained comparable even at 12 month follow up. Radiographs showed obliteration of fracture line, indicating formation of calcified tissue. Removal of splint was not associated with any increase in mobility. Most patients visited the department from far flung areas; however, a standard follow up of all patients was done up to 12 months post intervention as per protocol. They were further instructed to return to the department in case any the tooth became symptomatic, but no such complaint was reported [3].
It is important to keep in mind that assessment of status of such teeth is done based primarily on absence of symptoms and radiographic assessment of fracture healing. This is a relatively subjective approach to assess prognosis of the tooth in question. Discoloration of tooth over time, inability to bear heavy occlusal loads restricts the use of such techniques to non-load bearing areas. Previous reports highlight the use of one particular technique for management of horizontal fracture, such as immobilization of vital teeth [7]. In this article the authors have attempted to present several different situations which may be encountered clinically, for instance, use of intra-radicular splint to improve crown/root ratio and reposition fractured fragments or longer duration splinting for retaining vitality of teeth with horizontal root fracture. Highlighting the importance of selection of correct technique for management of horizontal root fracture depend on the level of fracture, state of vitality, crown by root ratio and level of mobility of the tooth. The replacement of a single anterior tooth presents the greatest aesthetic challenge to the clinician, many patients are unable to afford implants in such a scenario retention of natural dentition is the best alternative for horizontal root fracture .
Conclusion
Horizontal root fracture following trauma should not be considered as an indication for extraction. This case series highlights the conservative management of horizontal root fractures associated with both necrotic and vital fragments. Depending on the location of fracture line, vitality of pulp and displacement of fractured segment differing techniques may be selected for its optimal management. These Conservative non-surgical management of horizontal root fracture allows for aesthetic, economic alternative in developing economies.
[1]. Malmgren B, Hubel S, Transient discoloration of the coronal fragment in intra-alveolar root fracturesDental traumatology 2012 28:200-4.(http://www.endoexperience.com/documents/fracturediscoloration.PDF) [Google Scholar]
[2]. Aguiar CM, Mendes DA, Camara AC, Horizontal root fracture in a maxillary central incisor: a case reportGen Dent 2013 61(2):12-14. [Google Scholar]
[3]. Andreasen JO, Textbook and color atlas of Traumatic Injuries to the teeth 1981 2nd edPhiladelphia, PAWB Saunders:119-50. [Google Scholar]
[4]. Aras MH, Ozcan E, Zorba YO, Aslan M, Treatment of traumatized maxillary permanent lateral and central incisors horizontal root fracturesIndian J Dent Res 2008 19:354-56. [Google Scholar]
[5]. Croll T, Mark L, Helpin D, Use of self-etching adhesive system and compomer for splinting traumatized incisorsAAPD 2002 24:53-6.(http://www.aapd.org/assets/1/25/Croll1-02.pdf) [Google Scholar]
[6]. Gomes AP, d’Araujo EA, Gonçalves SE, Kräft R, Treatment of traumatized permanent incisors with crown and root fractures: A case reportDent Traumatol 2001 17:236-9.(link attached - http://hinarilogin.research4life.org/uniquesigonlinelibrary.wiley.com/uniquesig0/doi/10.1034/j.1600-9657.2001.170510.x/full [Google Scholar]
[7]. Kucukyilmaz E, Botsali MS, Keser G, Treatments of horizontal root fractures: Four case reportsJ Pediatr Dent 2013 1:19-23. [Google Scholar]
[8]. Wilson R, Manfrin T, Holland R, Repair characteristics of horizontal root fracture: a case reportDental Traumatology 2002 18(2):98-102. [Google Scholar]
[9]. Kocak S, Cinar S, Kocak MM, Kayaoglu G, Intraradicular splinting with endodontic instrument of horizontal root fracture—case reportDent Traumatol 2008 24(5):578-80. [Google Scholar]
[10]. Flores MT, Andersson L, Andreasen J, Guidelines for the management of traumatic dental injuries. I. Fractures and luxations of permanent teethDental Traumatology 2007 23(2):66-71. [Google Scholar]