Astrocytomas constitute a large and heterogenous group of tumours and notorious for wide differences in clinical incidence, gross & microscopic features & biologic behaviour. Although the radiological imaging and surgical techniques have substantially improved, the gold standard remains histopathological examination of an abundantly sampled tissue. However, morphology cannot be accurate prognostic indicator where pathologists receive small biopsy samples. The use of intraoperative cytology not only helps a surgeon in rapid diagnosis, also it is ensured that minimum injury is caused to the normal brain structures surrounding the tumour. Processing of remaining tissue for histopathology and also for immuno labelling gives the accurate grading of tumour indicating its proliferative capacity. The current study was undertaken to assess utility of intraoperative smear cytology in diagnosing and grading astrocytoma and correlating with histopathological and immunolabelling indices.
Materials and Methods
This was a prospective study of one year duration conducted in Department of Pathology, SMS Medical College, Jaipur. Our study included radiologically suspected astrocytic tumours of varying grades which on histopathology were confirmed to be astrocytoma. Patient’s history, clinical findings, radiological data were collected. All the observations were evaluated using simple and basic statistical tool, i.e. percentage.
For cytological examination, a tiny portion (1–2 mm3) of fresh tissue, received intraoperatively, was squashed between two slides to prepare smear. Slide was immediately fixed in methanol and stained using rapid Haematoxylin & Eosin (H&E) staining method. Histology sections were prepared from routine formalin fixed paraffin embedded tissue and stained using routine H&E method. Cytological diagnosis was correlated with final histological diagnosis. Histological diagnosis was used as gold standard and all the cases were graded using the World Health Organization (WHO) criteria published in 2007 [1]. It was based upon the recognition of the presence or absence of four morphologic criteria-nuclear atypia, mitoses, endothelial proliferation and necrosis. Increase in cellularity of astrocytes, mild nuclear pleomorphism and lack of mitotic activity were graded as Grade I. In Grade II, the nuclear pleomorphism increase but atypical mitosis is not seen. Presence of mitosis and marked nuclear pleomorphism were graded in Anaplastic Grade III. In Grade IV astrocytoma endovascular proliferation and tumour necrosis is seen.
Then immunolabelling was done using MIB-1 monoclonal antibody using a dilution of 1:100. Representative tissue blocks were selected and 4-mm thick paraffin sections were floated onto slides previously coated with poly-L-lysine. Antigen retrieval was done by microwave method using sodium citrate buffer (0.01 M at pH of 6.0). Immunostain visualization was achieved with streptavidin-biotin peroxidase technique. The slides were stained with 3, 3’-diaminobenzidine and then counterstained with Haematoxylin.
MIB-1immunostaining was evaluated by counting immunoreactive cells. Fields from the area of maximal labelling were chosen for counting. In glioblastomas (Grade IV), areas of sections free from necrosis or endothelial proliferation were selected. The MIB-1 LI was the number of MIB-1 labelled tumour nuclei expressed as a percentage of the total number (2,000) of tumour nuclei counted. All patients with scanty/predominantly necrotic material were excluded from our study.
Results
It was a prospective study of one year duration where 45 cases were diagnosed as astrocytoma histopathologically.
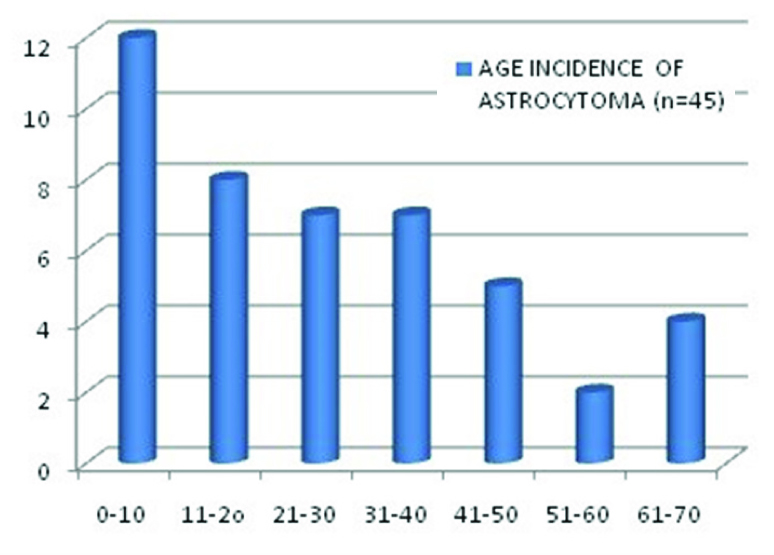
Maximum incidence was in first decade i.e. 12/45 (26.6%) & least in sixth decade with the rise in seventh decade [Table/Fig-1].
Age incidence of astrocytoma (n=45)
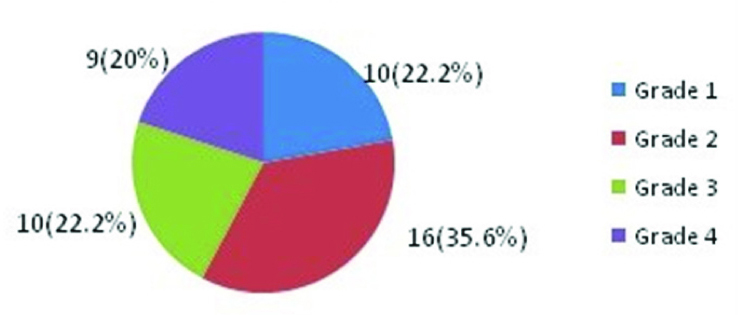
Incidence of individual grades are given below [Table/Fig-2]. It was summarized that maximum incidence were of astrocytoma grade II. Equal number of cases of Grade I (Pilocytic Astrocytoma) and astrocytoma Grade III (Anaplastic Astrocytoma) were observed. Grade IV (Glioblastoma Multiforme) were the least.
Incidence of grades of astrocytic tumours (n=45)
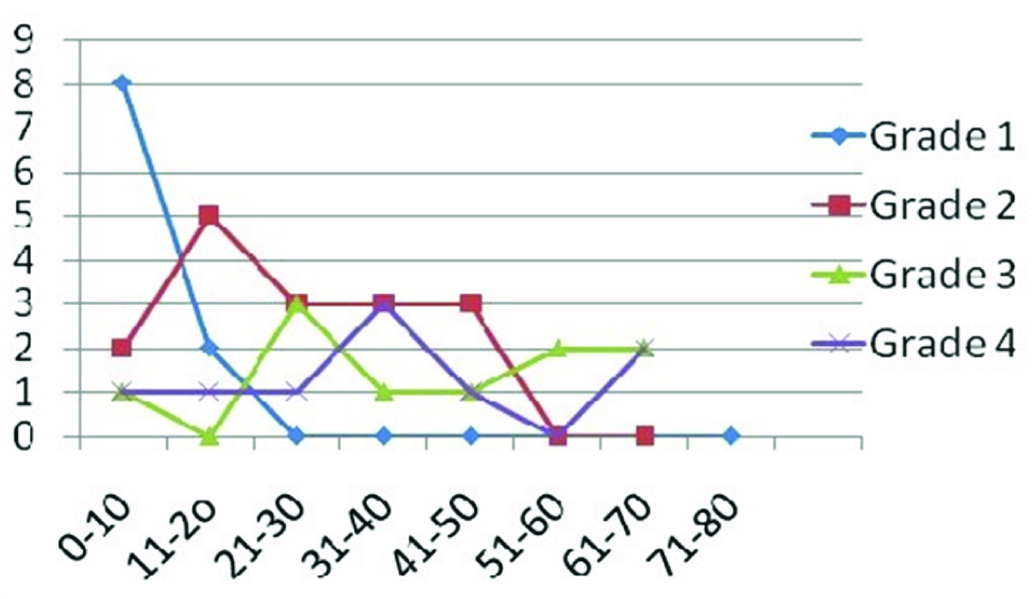
Age incidences of individual grades are shown below [Table/Fig-3]. Maximum incidence of Grade I was in first decade followed by second decade. Grade II astrocytoma occurred more commonly in second followed by third to fifth decade, Grade III in third decade followed by sixth & seventh decade, Grade IV in fourth decade with rise in seventh decade.
Age incidence of various grades of astrocytoma (n=45)
On cyto-histopathological correlation, misinterpretation in intraoperative diagnosis happened in 1 out of 45 cases. Thus we could achieve diagnostic accuracy of 97.7% [Table/Fig-4,5].
Cyto-histological comparison in diagnosis of astrocytoma
| Total cases of astrocytoma (histopathological diagnosis) | Correct cytological diagnosis | Accuracy |
|---|
| 45 | 44 | 97.7% |
Cyto-histological comparison of various grades of astrocytoma
| WHO Grading of Astrocytoma (n=45) | Total cases | Correct cytological grading | Accuracy (%) |
|---|
| Grade 1 | 10 | 09 | 90 |
| Grade 2 | 16 | 16 | 100 |
| Grade 3 | 10 | 10 | 100 |
| Grade 4 | 09 | 08 | 88.9 |
| Total | 45 | 43 | 95.6 |
Cytomorphological grading also correlated well with histological diagnosis [Table/Fig-6]. Only one case was undergraded as malignant astrocytoma.
Cyto-histological Comparison of Diagnosis and grading of astrocytoma
| Histopathological diagnosis | Cytological diagnosis | No of cases (n=45) |
|---|
| Pilocytic astrocytoma(Grade I) | Pilocytic astrocytoma(Grade I) | 09 |
| Pilocytic astrocytoma(Grade I) | Ependymoma | 01 |
| Low grade astrocytoma(Grade II) | Low grade astrocytoma(Grade II) | 16 |
| Malignant Astrocytoma(Grade III) | Malignant Astrocytoma(Grade III) | 10 |
| Glioblastoma Multiforme(Grade IV) | Glioblastoma Multiforme(Grade IV) | 09 |
Further, on immunolabelling, it was found that MIB-LI value increased as histopathological grading increased. MIB-LI of pilocytic astrocytoma (WHO Grade I) [Table/Fig-7] was ≤0.05%. In diffuse astrocytoma (WHO Grade II) [Table/Fig-8] the MIB-1 LI varied from 0.8-2.6% except in one case where it was 3.2% who presented with a recurrent mass. In anaplastic astrocytoma (WHO Grade III) [Table/Fig-9] MIB-1 LI was 3.5% to 7.5% and in Glioblastoma Multiforme (WHO Grade IV) [Table/Fig-10] it was 10-20%.
Squash smear of pilocytic (Grade I) astrocytoma showing long bipolar astrocytes & Rosenthal fibres (H&E,100x); 7b) Tissue section showing eosinophilic granular bodies (H&E,100x); 7c) Occasional MIB-1 immunolabelled nuclei (400x)

(a) Squash smear of Low grade diffuse (Grade II) astrocytoma showing increased cellularity and mild nuclear atypia (H&E,400x); (b) Tissue section showing increased cellularity and mild nuclear atypia (H&E,100x); (c) Few MIB-1 immunolabelled nuclei (400x)

(a) Squash smear of anaplastic (Grade III) astrocytoma showing mitotic activity and marked nuclear atypia (H&E,400x); (b) Tissue section showing marked nuclear pleomorphism (H&E,400x); (c) Many MIB-1 immunolabelled nuclei (100x).

(a) Squash smear of glioblastoma multiforme (Grade IV) showing marked pleomorphism (H&E,100x); (b) Tissue section showing nuclear palisading around necrosis and endovascular proliferation in the inset (H&E,100x); (c) Many bizarre MIB-1 immunolabelled nuclei (400x)

Discussion
The history of intraoperative cytology dates back to 1930, when Eisenhardt and Cushing introduced this technique by using supravital staining [2]. The technique has recently gained importance because of advent of CT and MRI guided stereotactic biopsies. Present work has been undertaken to study the diagnostic accuracy of squash smear technique for rapid per-operative diagnosis and grading of astrocytoma.
In our study, maximum incidence of astrocytoma was in first decade and maximum cases were of low grade diffuse astrocytoma (35.6%). However, literature states that GBM is most common type. We had 10 cases of Pilocytic astrocytoma (Grade I) which were seen in first two decades of life which is consistent with the literature. Grade II & Grade III astrocytomas peak at second & third decade respectively & literature states that their incidence is increasing in children & young adults. Grade IV astrocytoma was seen in adults and elderly age group. On cyto-histological correlation we received discordance of 1 out of 45 cases with accuracy of 97.7%. It was a case of pilocytic astrocytoma which was misdiagnosed as ependymoma due to the presence of perivascular radiating processes which appeared similar to ependymoma. Pilocytic astrocytoma can also have ependymal differentiation. In the present study, accuracy rate of 97.7% is comparable to the other studies conducted in the past [3,4].
Also, 1 out of 45 cases one case was intraoperatively undergraded as anaplastic astrocytoma. This was due to lack of necrotic areas. Hence, whenever such need arises a pathologist should never hesitate to ask for more tissue sample from the operating neurosurgeon. MIB-1 labelling indices also correlated with increasing grading of tumour. One case of low grade astrocytoma who presented with a recurrent tumour had a higher index as compared to other low grade tumour. This indicates an infiltrative nature of these tumour which was not cured after previous surgical resection. Such cases can also progress and present to higher grade as anaplastic astrocytoma or GBM later. Hence, MIB-LI, although not included in WHO grading, can suggest the proliferative nature of tumour. It can be helpful is assigning histopathological grading and in prognosis.
Various markers of proliferative potential have been used as independent indices of malignancy and tumour behaviour including estimation of thymidine labelling index, measurement of S-phase labelling index using bromodeoxyuridine (BrdU), DNA flow cytometry, staining of silver nucleolar organizer regions (AgNORs) and MIB-1 labelling. Out of these, MIB-1 labelling index (MIB-1 LI) is considered to be a preferred immuno-histochemical marker for cell proliferation [5] because of its very short half –life (an hour or less), which makes it less likely to label cells that have excited from the cycling phases and it can also be demonstrated on fixed tissues. There is steadily increasing evidence that Ki-67 do correlate fairly well with the prognosis, not only of individual patients with astrocytomas but, also with grades of malignancy in general such as in breast carcinoma. Many studies have demonstrated a significant positive correlation between MIB-Labelling indices & histological grade and have shown that higher MIB-1 LI is associated with shorter survival, however no cut-off values have been mentioned [6–8]. A study done by Neder et al., [9] also states that patients with MIB-LI of ≥ 3% has lower survival rates as compared to those below 3%. In our study MIB-1 index helped in correlating grading with cytological and histological parameters. MIB-1 labelling helped in assessing higher proliferative areas of tumours where both low grade and higher grades co-existed.
Conclusion
Intraoperative cytology consultation is not only supportive but is diagnostic for astrocytomas. In country like ours where facility of frozen section is not universally available, it wil give a rapid preliminary diagnosis for operative management and planning. Inadequate tumoural sampling with undergrading of some glioblastomas as anaplastic astrocytoma may occur, especially when diagnoses are based on tissues obtained from smaller biopsies.
A corroboration of cytology, histopathological diagnosis along with MIB-1 LI can help in giving accurate diagnosis and planning best management of these patients.