A Study of Eclampsia Cases Associated with Posterior Reversible Encephalopathy Syndrome
Shobha Bembalgi1, Vishal Kamate2, K.R. Shruthi3
1Associate Professor, Department of Obstetrics and Gynaecology, Karnataka Institute of Medical Sciences, Hubli, Karnataka, India.
2Assistant Professor, Department of Obstetrics and Gynaecology, Karnataka Institute of Medical Sciences, Hubli, Karnataka, India.
3Post Graduate Student, Department of Obstetrics and Gynaecology, Karnataka Institute of Medical Sciences, Hubli, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vishal Kamate, H.No. 58, 2nd Cross, Mahadwar Road, Belgaum, Karnataka- 590001, India.
E-mail: vkamate@gmail.com
Objectives
Incidence of eclampsia is 1 in 2000 to 3250 deliveries in developed countries and 1 to 5% in India. Posterior reversible encephalopathy syndrome (PRES) is a constellation of symptoms caused by reversible ischaemia mostly of the posterior cerebral vasculature. PRES has been associated with preeclampsia-eclampsia and acute renal injury. We present a study of patients in whom eclampsia was complicated with PRES. Our aim was to study the clinico-radiological profile, associated complications and outcome of patients who had eclampsia with PRES.
Materials and Methods
A retrospective study was done of all pregnancies diagnosed as eclampsia with PRES syndrome over a four year period from August 2010 to July 2014 managed at Karnataka institute of medical sciences, Hubli, India.
Results
Eleven patients had eclampsia with PRES syndrome of the 36,094 patients delivered in the institution over the study period. Nine of these were primigravidas, 8 were of 20-25 years age group, 10 presented with multiple seizure episodes. In eight patients seizures were controlled only with MgSo4. Perinatal mortality was seen in three patients. There were no maternal deaths in these cases.
Conclusion
Incidence of eclampsia with PRES syndrome was 0.03% amongst the patients delivered in Karnataka institute of medical sciences. The incidence of PRES was more amongst cases of postpartum eclampsias as compared to antepartum eclampsias. PRES was more common in primigravidas and younger age group (20 to 25 years). Signs of imminent eclampsia like headache, epigastric pain and blurring vision were uncommon in these patients. In the majority of the patients seizures were controlled with MgSo4 alone. Prognosis of eclamptic patients with PRES was favourable.
Ante partum eclampsia, Cerebrovascular autoregulation, Imminent eclampsia, Post partum eclampsia, Pre-eclampsia, Vasogenic brain oedema
Introduction
Incidence of eclampsia is 1 in 2000 to 3250 [1,2], deliveries in developed countries and 1 to 5% in India [3,4]. Eclamptic seizures can occur antepartum, intrapartum or postpartum. Late postpartum eclampsias are those that occur 48 hours after delivery and account for 5-26% of all eclampsia cases [5]. Posterior Reversible Encephalopathy Syndrome (PRES) is a usually reversible neurologic syndrome characterized by a variety of clinical features like headache, altered consciousness, visual disturbances and/or seizures [6.9] typically in a patient with new onset hypertension. PRES has been associated with preeclampsia-eclampsia and acute renal injury. Here we present a study of patients in whom eclampsia was complicated with PRES. Our aim was to study the clinico-radiological profile, associated complications and outcome of patients who had eclampsia with PRES.
Materials and Methods
We conducted a retrospective study of all cases of eclampsia complicated with PRES treated at Karnataka institute of medical sciences, Hubli, from August 2010 to July 2014. The clinico-radiological features, associated complications, perinatal and maternal outcomes were studied.
Results
A total of 36,094 patients delivered at Karnataka institute of health sciences, Hubli, during the study period, that is between August 2010 to July 2014. Of these 11 patients had eclampsia complicated with PRES with an incidence of 0.03% of all deliveries. The incidence was more among patients with post partum eclampsia (55%) than those presenting with antepartum eclampsia (45%). The incidence was more in primigravida patients (81%) than in multigravidas (19%). Most patients were of relatively younger age group with 81% cases between 20-25 years age group. There were no cases seen in teenage pregnancy and above 30 years. The demographic factors are summarized in [Table/Fig-1]. Signs of imminent eclampsia prior to onset of seizures were uncommon in these patients although headache was present in few patients after seizure onset. Clinical features are summarized in [Table/Fig-2]. In majority of the patients (64%) the seizures were multiple and were controlled by MgSo4 alone. The remainder required phenytoin sodium due to recurrent seizures inspite of starting MgSo4. Treatment given is summarized in [Table/Fig-3]. Perinatal mortality was high (27%) among patients with PRES and all of these were seen amongst patients with antepartum eclampsia. However, there was no maternal mortality observed in our study. In our study we observed that maternal prognosis in patients of eclampsia with PRES syndrome was good.
Discussion
Posterior Reversible Encephalopathy Syndrome (PRES) also known as reversible posterior leukoencephalopathy syndrome is characterized by headaches, seizures and visual disturbances [6-9] associated with an abrupt increase in blood pressure. The blood pressure in eclamptic patients varies with 20-54% having severe HTN (160/110) 30-60% mild HTN (140-160/90-110) and 10% having no HTN. Most cases of PRES in obstetrics are seen in the setting of acute hypertensive encephalopathy, preeclampsia and eclampsia or nephrotic states. It is thought to be secondary to endothelial damage in the setting of hypertension and failure of cerebrovascular autoregulation with subsequent vasogenic oedema. The posterior circulation is more sensitive to the effects of hypertension.
The rate of increase in BP is a more important factor for development of PRES than the absolute rise in BP. There is development of vasogenic brain oedema mostly in the posterior circulation as a result of breakdown of blood brain barrier [10,11]. An acute rise in BP over a short period of time causes failure of normal autoregulatory mechanisms that usually control blood flow to the brain in a hypertensive state [12-14]. Likewise patients with chronic hypertension are less likely to develop PRES as their circulation is adapted to higher levels of BP. PIH patients don’t seem to enjoy this advantage where increase in BP to high levels occurs in relatively short periods. Another theory suggests that acute rise in BP causes hypoperfusion leading to endothelial damage secondary to hypoxia and subsequent cytotoxic oedema. Sepsis and septic shock can precipitate PRES by endothelial derangement and microcirculatory disturbances.
Generalized seizures are often the most common clinical manifestation of PRES [7]. Headache is the most common symptom. Visual disturbances can range from blurring of vision to hemianopsia or even cortical blindness. However, unlike many other studies and case reports we observed that signs of imminent eclampsia may not be present in patients of eclampsia with PRES syndrome. Hemiparesis, dystonias are rare features. Sluggish pupillary reflexes or myosis can be seen. Papilloedema and haemorrhagic changes on fundus examination can be signs of raised intracranial pressure. Recurrence is reported in 3.8% of cases in a recent series [15].
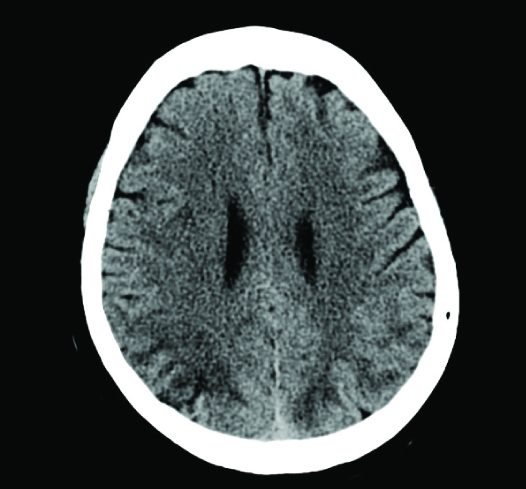
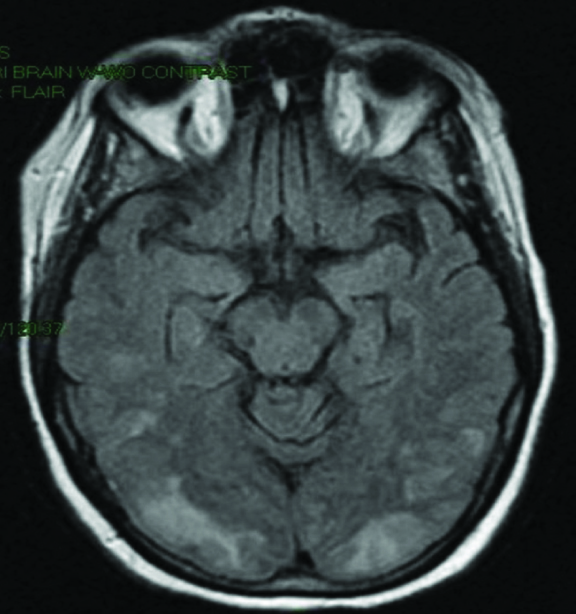
The brain imaging shows oedema of white matter and reversible ischaemic changes predominantly in areas perfused by posterior brain circulation, that is, the parieto-occipital areas [16]. The findings include non-enhancing white matter abnormalities that appear as areas of low attenuation on CT [Table/Fig-4]. MRI is the investigation of choice. On MRI multifocal T2 hyperintensities are seen mainly in parietal and occipital cortex [Table/Fig-5] but can also involve other parts of the cortex, thalamus, basal ganglia, cerebellum and brain stem. Diffusion Weighted Images (DW1) and Apparent Diffusion Coefficient mapping (ADC) can differentiate between vasogenic and cytotoxic oedema [6,17]. Ischaemic changes on DW1 and ADC images are associated with worse prognosis [18]. Focal regions of symmetric hemispheric oedemas are often seen. Haemorrhage, focal haematoma or isolated subarachnoid haemorrhage is seen in 15% of cases [19].
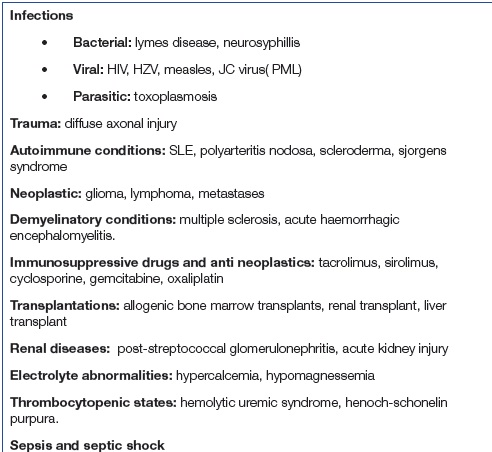
Prophylactic MgSo4 should be started on appearance of imminent symptoms. It is important to treat the aetiology or else this can progress to irreversible neurological sequelae even death. Blood pressure should be controlled by using I.V labetelol or oral nifedepine [20]. However, care should be taken not to cause a sudden hypotension as this may adversely affect the brain perfusion. An immediate reduction of mean arterial pressure by 20-25% in the first two hours should be aimed at followed by gradual reduction thereafter. MgSo4 is the treatment of choice in eclampsia. If the patient is antenatal, delivery should be expedited. In a case of status eclampticus I.V lorazepam is the recommended drug used along with invasive ventilation and other general measures. Treated in time, most patients exhibit complete neurologic recovery within two weeks accompanied by resolution of the radiologic lesions. Prognosis is poorer if there is a large area of involvement or associated ischaemia or infarct. Obstructive hydrocephalus is another known complication. Apart from preeclampsia-eclampsia and acute kidney injury PRES can be seen in a variety of other clinical conditions which are enumerated in [Table/Fig-6].
| Age | <20 | - |
| 20-25 | 9 |
| 26-30 | 2 |
| 31-35 | - |
| >35 | - |
| Parity | Primi | 9 |
| Multi | 2 |
| Time of presentation | Antenatal | 5 |
| Postnatal | 6 |
| Headache/vomiting | 3 | Anaemia | 4 |
| Epigastric pain | - | Abruption | - |
| Anasarca | - | ARF | 1 |
| Hypertension/protienuria | 10 | Pulmonary oedema | - |
| Sudden blindness | - | DIC | - |
| Seizures 1 | 3 | Eclampsia | 9 |
| 2-4 | 7 | PPH | - |
| >4 | 1 | HELLP | - |
| Oliguria | 1 | encephalopathy | 1 |
| Mgso4 | 8 |
| Phenytoin | 1 |
| MgSo4+phenytoin | 2 |
CT scan showing low attenuation of posterior cortical areas
MRI showing white matter hypodensities in parieto-occipital regions
Other conditions associated with Pres
Conclusion
Incidence of eclampsia with PRES syndrome was 0.03% amongst the patients delivered in Karnataka institute of medical sciences. The incidence of PRES was more amongst cases of postpartum eclampsias as compared to antepartum eclampsias. PRES was more common in primigravidas and younger age group (20 to 25years). Signs of imminent eclampsia like headache, epigastric pain and blurring vision were uncommon in our patients. In the majority of the patients seizures were controlled with MgSo4 alone. Prognosis of eclamptic patients with PRES was favourable.
[1]. SJ Ventura, JA Martin, SC Curtin, Births: Final date for 1998National Vital Statistics Reports 2000 48(3) [Google Scholar]
[2]. MR Pradeep, S Lalitha, Retrospective Study of Eclampsia in a Teaching HospitalInternational Journal of Recent Trends in Science And Technology 2013 8(3):171-73. [Google Scholar]
[3]. S Gupte, G Wagh, Preeclampsia–EclampsiaJ Obstet Gynecol Ind 2014 64(1):4-13. [Google Scholar]
[4]. B Anuja, K Sayali, G Sunita, K Anjali, J Sulabha, S Savita, Eclampsia: Maternal and fetal outcomeJ of South Asian Federation of Obstet Gynaecol 2013 5(1):19-21. [Google Scholar]
[5]. MN Jamie, E Shervin, Late Postpartum Eclampsia with Posterior Reversible Encephalopathy SyndromeHospital Physician 2007 43(6):45-9. [Google Scholar]
[6]. SP Vinod, BR Dhamangaonkar, RC Pattanshetti, MM Patil, Posterior Reversible Encephalopathy Syndrome in Early Postpartum Women: A Case ReportJournal of Clinical and Diagnostic Research 2014 8(4):RD01-2. [Google Scholar]
[7]. B Justin, YO Michelle, W Kedra, M Amanda, K Rachael, K Majid, Posterior reversible encephalopathy syndrome in 46 of 47 patients with eclampsiaAm J Obstet Gynecol 2013 208:e1-6. [Google Scholar]
[8]. T Anjan, S Ankur, K Rakesha, Posterior reversible encephalopathy syndromeJ of Obstet Anaesth Crit Care 2014 4(2):50-2. [Google Scholar]
[9]. A Chhabra, S Jagtap, Postpartum seizures with posterior reversible encephalopathy syndrome following cesarean delivery for tripletsJ Obstet Anaesth Crit Care 2014 4(1):50-2. [Google Scholar]
[10]. P Rodrigo, EM Paul, V Joseph, Posterior Reversible Encephalopathy Syndrome: A ReviewCrit Care & Shock 2009 12:135-43. [Google Scholar]
[11]. J Hinchey, C Chaves, B Appignani, J Breen, L Pao, A Wang, A reversible posterior leukoencephalopathy syndromeN Engl J Med 1996 334(8):494-500. [Google Scholar]
[12]. H Xuan, X Jinfeng, C Zao, L Guoliang, J Hong, Posterior reversible encephalopathy syndrome with involvement of the cervical cord and medulla: A case reportJournal of Clinical and Diagnostic Research 2015 9(1):CD01-2. [Google Scholar]
[13]. K Ishikura, M Ikeda, Y Hamasaki, H Hataya, G Nishimura, R Hiramoto, Nephrotic state as a risk factor for developing posterior reversible encephalopathy syndrome in paediatric patients with nephrotic syndromeNephrol Dial Transplant 2008 23(8):2531-36. [Google Scholar]
[14]. MJ Cipolla, JG Sweet, SL Chan, Cerebral vascular adaptation to pregnancy and its role in the neurological complications of eclampsiaJournal of Applied Physiology 2011 110(2):329-39. [Google Scholar]
[15]. JM Sweany, WS Bartynski, JF Boardman, “Recurrent” posterior reversible encephalopathy syndrome: report of 3 cases—PRES can strike twice!J Comput Assist Tomogr 2007 31(1):148-56. [Google Scholar]
[16]. WS Bartynski, Posterior Reversible Encephalopathy Syndrome, Part 1: Fundamental Imaging and Clinical FeaturesAm J Neuro Radiol 2008 29(6):1036-42. [Google Scholar]
[17]. NMAM Ibrahim, EB Manal, MRI imaging of posterior reversible encephalopathy syndrome associated with pregnancyThe Egyptian Journal of Radiology and Nuclear Medicine 2014 45(2):505-10. [Google Scholar]
[18]. JC Diego, HL Patrick, GC Norbert, Posterior Reversible Encephalopathy Syndrome: Prognostic Utility of Quantitative Diffusion-Weighted MR ImagesAm J NeuroRadiol 2002 23(6):1038-48. [Google Scholar]
[19]. CJ Stevens, MKS Heran, The many faces of Posterior Reversible Encephalopathy SyndromeBr J of Radiology 2012 85:1566-75. [Google Scholar]
[20]. American College of Obstetricians and Gynecologists. Emergent therapy for acute-onset, severe hypertension with preeclampsia or eclampsia. ACOG Committee Opinion no. 623, Feb 2015 [Google Scholar]