Amphotericin B Resistant Apophysomyces elegans Causing Rhino-oculo-Cerebral Mucormycosis in an Immunocompetent Host
Debasis Biswas1, Aarti Kotwal2, Barnali Kakati3, Sohaib Ahmad4
1 Professor, Department of Microbiology, Himalayan Institute of Medical Sciences, Jolly Grant, Dehradun, India; Additional Professor, Department of Microbiology, AIIMS Bhopal, Bhopal, India.
2 Associate Professor, Department of Microbiology, Himalayan Institute of Medical Sciences, Jolly Grant, Dehradun, India.
3 Associate Professor, Department of Microbiology, Himalayan Institute of Medical Sciences, Jolly Grant, Dehradun, India.
4 Professor, Department of Medicine, Himalayan Institute of Medical Sciences, Jolly Grant, Dehradun, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aarti Kotwal, Associate Professor, Department of Microbiology, Himalayan Institute of Medical Sciences, Swami Ram Nagar, Jolly Grant, Dehradun, Uttarakhand- 248140, India. E-mail : aartiraghuvanshi@yahoo.co.in
Mucormycosis, an angioinvasive infection is caused by the ubiquitous filamentous fungi of the order Mucorales and class Mucormycetes. Reports of this disease are on the rise over the past few decades. Rhino-oculo-Cerebral presentation associated with uncontrolled diabetes is the predominant characteristic of this entity. We report here a case of rhinooculocerebral mucormycosis (ROCM) due to Apophysomyces elegans (A. elegans) in a 45-year-old diabetic lady with background illness of hypothyroidism and polyradiculoneuropathy. Though this condition is usually managed with surgical debridement of the affected tissue and medical therapy with Amphotericin B, the isolate recovered in our case was found to be resistant to Amphotericin B.
Antifungal susceptibility profile, Diabetes, Mucormycosis
Case Report
A 45-year-old female diabetic patient, with history of hypothyroidism and polyradiculoneuropathy, was admitted to the medical ward of Himalayan Institute of Medical Science, a tertiary care hospital in North India with orbital cellulitis, uniocular blindness, septicemia, acute renal insufficiency and metabolic acidosis. On examination, she was irritable, stuporous and tachypneic. Slight proptosis, conjunctival chemosis and lid swelling was observed in the right eye. Both direct and consensual pupillary reflexes were absent. A mucoid discharge was observed in the congested nasal mucosa. The soft palate showed an eschar which, after taking consent from patient was scraped for diagnostic work up. The scraping was sent for microscopy and culture. The significant findings, among routine laboratory investigations, included leukocytosis and metabolic acidosis. Patient’s restless condition did not allow MRI to be performed properly.
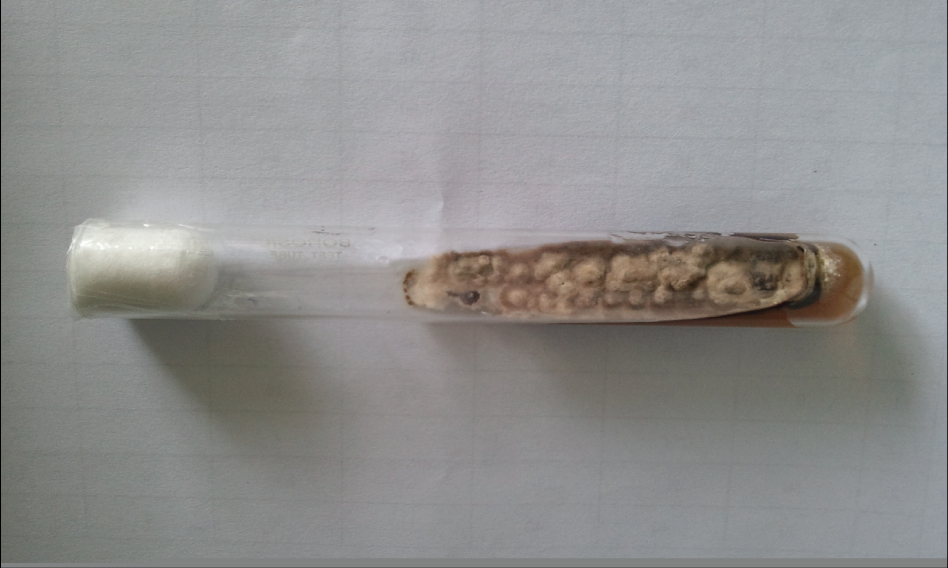
KOH mount, prepared from the scraping, revealed broad, aseptate fungal hyphae. Fast-growing creamy white colonies were grown on sabouraud’s dextrose agar (SDA) [Table/Fig-1]. For sporulation, the isolate was sub-cultured on corn meal agar and incubated at 250C. Abundant sporulation was observed after five days. Microscopically, the Lactophenol cotton blue (LCB) mount revealed broad, hyaline, infrequently septate, thin-walled hyphae. Dark brown and thick- walled sporangiophores, arising singly at the ends of stolon-like hyphae, were seen. Rhizoids were observed at the ends of stolon- like hyphae, but not opposite to the overlying sporangiophores. Abundant sporangia with dark, champagne glass-shaped apophyses, borne at the tips of sporangiophores, were present. Sporangia were present at the tips of sporangiophores and were pyriform and multispored. The sporangiospores were oblong, subhyaline, and smooth [Table/Fig-2].
Apophysomyces elegans colony surface on SDA (sabourauds dextrose agar) medium
Lactophenol cotton blue mount showing dark, thin walled sporangiophore of Apophysomyces elegans and champagne glass shaped apophysis (x400)

The patient was initially managed with broad spectrum antibiotics (pipericillin-tazobactum and clindamycin), local antibiotic eye drops and supportive treatment. Following the microbiological confirmation of infection with Apophysomyces elegans, the patient was put on intravenous liposomal Amphotericin B. However, her condition worsened during the course of treatment. Antifungal susceptibility testing was performed with Amphotericin B, Voriconazole, Fluconazole and Ketoconazole, according to the guidelines of CLSI M-38A document [1]. For all of these antifungal agents, the isolate showed higher MICs compared to the recommended breakpoint for molds. The MIC for Amphotericin B was 16μg/mL (Sensitive: <2μg/ml), for Voriconazole it was 32μg/ml (Sensitive: <8μg/ml), for Ketoconazole and Fluconazole and it was 32μg/ml and 64μg/ml respectively (Sensitive: <16μg/ml). The patient was advised urgent debridement of the tissue and put on Posaconazole. However, she left against medical advice and was lost to follow-up.
Discussion
Rhino-oculo-Cerebral Mucormycosis (ROCM) is a rapidly fatal condition, usually encountered among immunodeficient hosts. Among the causative agents responsible for ROCM, Rhizopus, Lichtheimia, and Rhizomucor have been commonly reported. Apophysomyces elegans (A. elegans), a relatively new addition to the family of Zygomycetes, is now being increasingly isolated from patients throughout the world.
Interestingly, many of the patients suffering from ROCM, due to A. elegans, did not have any immune-compromising co-morbidity [2,3]. This was supported by the study of Gomes et al., who reported that 66% of patients with A. elegans infection have no underlying illness [4]. Similarly, in the largest reported case series on A. elegans, Chakrabarti et al., observed that an underlying disease could be determined in only 2 of the 8 patients [5]. The common predisposing risk factors reported with this infection have included diabetes mellitus [6], organ transplantation [7], alcoholic cirrhosis [5], chronic sinusitis [5] and idiopathic myelofibrosis [5]. Our patient, being diabetic, had one of these common risk factors associated with this condition. Additional risk factors, not commonly reported with this condition, viz. hypothyroidism and renal insufficiency, might have aggravated her risk of acquiring this infection.
Majority of patients have been reported to acquire this infection through percutaneous inoculation of the pathogen following trauma resulting from motor vehicle accidents, burn wounds and insect bites [5]. However, there was no history of antecedent trauma in our patient, which probably hints at acquisition of the rhino-oculo-cerebral infection through spore inhalation.
The management of A. elegans- associated ROCM is also difficult due to the limited therapeutic options available. With the majority of the commonly used azoles (ketoconazole, fluconazole, itraconazole and voriconazole) and echinocandins being ineffective, surgical debridement, Amphotericin B and correction of the underlying medical condition are the usual treatment modalities employed [8]. High dose Amphotericin B (<1.5 mg/ kg/ day) is considered as the drug of choice for mucormycosis. With the recent availability of lipid formulations, better tissue distribution and quicker delivery of the drug to the site of infection has been possible [5]. In a recent review on mucormycosis caused by unusual mucormycetes, Gomes et al., observed that 83% of the A. elegans isolates had MIC of <1μg/ml for Amphotericin B [4]. Strains with a more resistant profile (n= 18) have been recently described, with the MIC50 and MIC90 of Amphotericin B being 2 μg/ml and 4 μg/ml, respectively [9]. Prognostic association has also been demonstrated in this retrospective study with MIC values. All patients with Amphotericin B MICs of <1μg/ml recovered, whereas 43% of patients infected with more resistant strains (MICs of >1μg /ml) died [5]. Chakrabarti et al., also observed poor response to treatment in 2 of their 8 patients. Though treatment failure and relatively high MICs with Amphotericin B have been reported in the literature, this is the first report of an A. elegans isolate that was completely resistant to Amphotericin B.
Conclusion
Isolation of a rare fungus from immune-competent individual should not be ignored. Antifungal susceptibility profile of such fungus assumes great significance in advent of rising incidences of resistance to valued antifungal drugs like Amphotericin B.
[1]. National Committee for Clinical Laboratory Standards. 2002. Reference method for broth dilution antifungal susceptibility testing of filamentous fungi. Approved standard. NCCLS document M38-A. Clinical and Laboratory Standards Institute, Villanova, Pa [Google Scholar]
[2]. Schütz P, Behbehani JH, Khan ZU, Ahmad S, Kazem MA, Dhar R, Fatal rhino-orbito-cerebral zygomycosis caused by Apophysomyces elegans in a healthy patientJ Oral Maxillofac Surg 2006 64(12):1795-802. [Google Scholar]
[3]. Sridhara SR, Paragache G, Panda NK, Chakrabarti A, Mucormycosis in immunocompetent individuals: an increasing trendJ Otolaryngol 2005 34(6):402-06. [Google Scholar]
[4]. Gomes MZ, Lewis RE, Kontoyiannis DP, Mucormycosis caused by unusual mucormycetes, non-Rhizopus, -Mucor, and -Lichtheimia speciesClin Microbiol Rev 2011 24(2):411-45. [Google Scholar]
[5]. Chakrabarti A, Ghosh A, Prasad GS, David JK, Gupta S, Das A, Apophysomyces elegans: an emerging zygomycete in IndiaJ Clin Microbiol 2003 41(2):783-88. [Google Scholar]
[6]. Blair JE, Fredrikson LJ, Pockaj BA, Lucaire CS, Locally invasive cutaneous Apophysomyces elegans infection acquired from snapdragon patch testMayo Clin Proc 2002 77(7):717-20. [Google Scholar]
[7]. Alexander BD, Schell WA, Siston AM, Rao CY, Bower WA, Balajee SA, Fatal Apophysomyces elegans infection transmitted by deceased donor renal allograftsAm J Transplant 2010 10(9):2161-67. [Google Scholar]
[8]. Liang KP, Tleyjeh IM, Wilson WR, Roberts GD, Temesgen Z, Rhino-orbitocerebral mucormycosis caused by Apophysomyces elegansJ Clin Microbiol 2006 44(3):892-98. [Google Scholar]
[9]. Almyroudis NG, Sutton DA, Fothergill AW, Rinaldi MG, Kusne S, In vitro susceptibilities of 217 clinical isolates of zygomycetes to conventional and new antifungal agentsAntimicrob Agents Chemother 2007 51(7):2587-90. [Google Scholar]