Substance abuse has been defined as the use of chemical substances for non medical purposes in order to achieve alterations in psychological functioning. The substances commonly abused in India include nicotine, alcohol, cannabis and opioids. However, the use of solvents and propellants is also on the rise as these are inexpensive, legally available household, industrial, office and automobile products; which are more commonly available to children and adolescents. We hereby describe a 16-year-old boy with combined volatile and alcohol abuse; who presented with increasing ataxia, visual and hearing disturbances.
Alcohol abuse, Diffuse cerebral and cerebellar atrophy, Polychloroprene solvent, Sensorineural hearing loss
Case Report
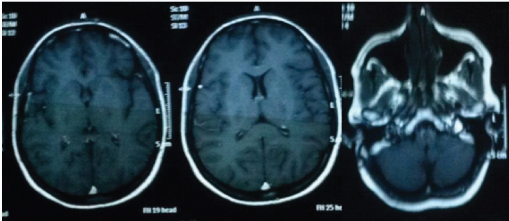
A 16-year-old adolescent male with a normal birth history and developmental milestones and belonging to low socioeconomic status; was brought to the outpatient department by his mother who permitted and consented along with the child in writing the report, complained that the child was smelling a rubber based adhesive using a handkerchief since the last 3 years. There was significant family history of alcohol dependence in father. There was no history of fever, head injury, seizure or attention deficit hyperactive disorder. There was no history of stress, tension or depressive thoughts. The toluene based substance abuse began gradually from 5ml/day and picked up to 20 ml each per day gradually over a span of 1 year which remained relatively stable during the presentation to the outpatient. After acute ingestion of Polychloroprene based solvent; the adolescent complained of tinnitus, slurring of speech, restlessness tremors, dizziness and ataxia. During the phase of withdrawal, there was coprolalia with assaultive and abusive behaviour, increasing fights, maladaptive behaviour and headache. These symptoms increased in severity; which compelled the parent to seek help. In addition, excessive tearing in the morning, headaches, decreased cognitive ability were the prominent symptoms in the morning; due to withdrawal. After obtaining detailed history, it was found that there was no confusion, visual hallucinations and/or seizure. Alcohol abuse began approximately 6 months after the volatile substance abuse, on detailed questioning child was asked whether he needed to cut down on the drinking behaviour, his annoyance, guilty and use of alcohol eye opener in the morning the response was positive for ¾ of the questions. He further added that the alcohol abuse began when the patient’s friends circle changed to include more people of higher age group. The patient used to steal money from his house in order to fetch the abused substance. The child was a school drop out as he faced inability to concentrate and low scores at school. Moreover, he often was involved in assaultive behaviour at school. The alcohol consumption increased from initially 20-40 ml of local alcohol (42.6% w/v) average per day to approx 60-120 ml per day (42.6%w/v); later during the span of last 2 months before presentation to the outpatient department. The child abused glue more than the alcohol due to its easy availability. During times of the day when no glue was consumed; alcohol abuse was noted along with the peers of elder age. During the phase of acute alcohol intoxication alone; the adolescent complained of nausea, headache, dizziness and excessive somnolence however when combined with glue sniffing; disorientation and ataxia, restless, diaphoresis and nystagmus were complained of, in addition. The child also developed blurring of vision and inability to perceive numbers and letters in the central visual field and fixed hearing deficits to increased frequency sound was noted; more prominent during the last 2 months, during which period combined abuse was done and dose of alcohol was increased to about 60-120 ml of (42.8% w/v) alcohol per day. A progressively increasing tendency of violence, disorientation, restlessness was noticed by the mother and his family in the form of anger outbursts, abusive and assaultive behaviour in the last two months during which alcohol intake was accelerated. The child presented to the clinic in a state of withdrawal since the mother had not let the child consume any substances since the last 2 days. The child tried to abstain from glue and alcohol a few times; but each episode of abstinence was followed by increase in the use. During the phase of abstinence; the child complained of increasing slurring of speech, difficulty hearing voices and sleep disturbances. General physical examination revealed a rash over the nostrils and nasolabial folds; a low BMI for age and a debilitated adolescent, with conjunctival pallor and a resting pulse of 92/min, and blood pressure of 110/80 mmHg. The central nervous examination exhibited symptoms of withdrawal including combativeness, irritability, aggressiveness, an impaired long term recall on minimental status examination with a score of 20. The psychometric tests scored low on aptitude and skills. IQ assessment was done using Seguin Form board, Malin’s intelligence scale for Indian child. The test score indicated to a below average intelligence in the child. On the Family Environmental Scale; there was a low score in all subgroups like personal, relationship, and system maintenance. The areas of behaviour control, problem solving, communication, affective response scored low. Cranial nerve examination showed normal pupillary reflexes and mild pallor of both optic discs on fundus examination, hearing loss of sensorineural type on both sides of moderate type. The child had a normal motor examination and sensory examination and flexor plantar response. Cerebellar examination revealed ataxic gait with a wide base and a moderate dyssmetria was observed on finger nose test; abdominal examination revealed hepatomegaly with liver margin 2 cm below costal margin and a span of 12 cm chest and cardiovascular examination was normal. The haematological workup revealed mild anaemia with Hb of 8gm% with MCV of 104 fl/cell, hypersegmented polymorphs and macrocytosis and were noted on the peripheral smear. The vitamin B12 levels were low 12pg/dl (nl200-900pg/dl) and liver function tests had transaminases 3 times the upper limit. (ALT-152U/l, ASt-200U/L, ALP-160U/L). A grade I fatty liver was noticed on abdominal sonogram. Audiometery results demonstrated moderate sensorineural hearing loss. Urine drug screen for alcohol was found to be negative. Urine for heavy metal screen was found to be negative. Renal Function tests, serum electrolyte, glucose, serologic tests for syphilis, urinalysis and chest radiograph were normal. Urine EEG, electromyogram, nerve conduction studies and electro retinogram was found to be normal. The contrast study of the head sequential sections showed cerebellar atropy and cortical atropy and generalized attenuation of white matter [Table/Fig-1]. The patient was admitted for the treatment of alcohol withdrawal and management of withdrawal due to volatile substance abuse; pharmacological therapy was begun using thiamine, Lorazepam, were given to decrease agitation and maintenance fluids were begun as well. Buspirone was begun at 5 mg/day and increased to 30mg/day. When the condition of the child stabilized; a short term course of supportive psychotherapy which included cognitive behavioural therapy was employed. This involved exploring and addressing problems which co-occurred with the abuse as well as the positive and negative consequences of drug use. A family based approach and person centered general counselling was adopted to help in recognizing and reducing craving and avoiding high risk situations. With the management of the patient; there was a subsequent decrease in the frequency of volatile substance abuse as well as decreased craving for the volatile substances as well as the alcohol. The general debilitation of the adolescent was improved during the process of detoxification and high energy feeds were instituted after correcting the vitamin and metabolic disturbances. Social workers were also involved in the process. They took detailed histories, delivered brief interventions to help the child for a behavioural change, and assessed the progress and provided encouragement and assistance to rebuild the child’s life. It also included the development of drug logs (when the child took the drug and when he was abstinent) and progress reviews to avoid the risky situations. Engagement in healthy was promoted and periodic rewards for abstaining were offered to the child. Alcohol dependence in father was also addressed and was included in the treatment. The child was discharged from the hospital uneventfully. The alcohol intake decreased during the subsequent follow-up visits. The child had a regular follow up with the clinic for a span of 1 year during which general condition of the child showed improvement however then subsequently dropped out.
Contrast study of the head: Sequential section associated with cerebeller atrophy and generalized attenuaton of white matter
Discussion
Substance abuse is on the rise in India particularly among the adolescents. The last several decades have noticed a growing prevalence of inhalant use in India; most notably volatile petroleum products, correcting fluids and adhesives [1–3]. There are very few reported studies from India on inhalant abuse. Between 1978- 2003; a study carried out showed that 4.7% of the adolescents used inhalants as the primary drug and 1.2% of them consumed inhalants as the secondary drug [1]. Another study done over a course of 2 years demonstrated that among majority of adolescents; the first use was attributed to curiosity and a desire to experiment [4]. The reason for growing use of inhalants among adolescents may be attributed to the low cost, easy availability and faster action [3,5]. Few studies document higher use of inhalants by adolescents of low to middle socio economic status [3,5,6]. There is also high prevalence of school dropouts and unemployed status [1,3,6].
There are several consequence of inhalant abuse. The patient may suffer from asphyxia, accidental injury, cardiac arrhythmias, respiratory depression; and in most severe cases; it may lead to death [6,7]. Continuous use can lead to the development of withdrawal syndrome on abrupt discontinuation of use. The symptoms observed upon withdrawal include sweating, nausea, vomiting, lack of sleep, craving, lack of concentration, jitteriness, irritability, rise in heart rate, headache, body aches, tingling sensations; and in some of the cases, can even lead to delusions, altered perceptions and hallucinations inhalants produce vapours, these can be sniffed or taken in deep breaths. The effect appears within minutes. The duration of the high can last from minutes to hours [8]. Inhalant abuse in small doses produces a pleasing sensation and a sense of euphoria [7]. However with increasing doses; illusions, auditory and/or visual hallucinations, fearfulness and impaired perception of size and shape may be noticed in the patient. Studies looking at white matter changes demonstrate that inhalant abuse is associated with a lower IQ; affecting both verbal and performance IQ; however the former is affected more [9,10].
Alcohol abuse in India too is rising rapidly. In 1980s, the first age of alcohol use was reported to be 28 years; but this has now fallen to 17 years in 2007 [11]. Alcohol intoxication also has several dire consequences. These include poor judgement, impaired coordination, ataxia, nausea, vomiting, euphoria and slurring of speech. Withdrawal from alcohol consumption can lead to development of anxiety, difficulty with sleep, autonomic instability, hallucinations –visual, tactile or auditory and seizures; called delirium tremens. Alcohol abuse in children manifests as difficult behaviour in school, social impairment, inability to learn and the development of conduct disorder can also occur. A consumption of 40 g of pure alcohol in a day by men and 20 g of pure alcohol in day by women falls under the criteria for heavy drinking; causing harm to health [12].
The child also suffered from anaemia as seen in case. Anaemia in alcoholics has a complex and multifactorial aetiology and can be microcytic or macrocytic. Poor nutrition, liver dysfunction and a state of chronic inflammation all contribute to it [13].
There are many factors which may be contributory to the development of substance abuse in the patient in this case report which can be explained on the basis of bio-psycho-social model. These include family history of substance use, peer pressure, easy availability of drugs, lower social strata, family with conflicts and lack of proper parenting. The patient’s intellectual decline can be explained by the presence of cerebral atrophy findings; similar findings have been reported by the author of various other studies too [14–16]. As seen in our case as well, the loss of vision was progressive and the patient’s visual acuity decrease maybe because of toluene induced optic neuritis and; also the fundic examination in our patient revealed pale optic discs [17]. There are no studies currently in literature featuring combined abuse of glue and alcohol. In our case; when the child was suffering from combined glue and alcohol intoxication; disorientation, ataxia, restless, diaphoresis and nystagmus were noted. In the phase of combined withdrawal; the child complained of increasing slurring of speech and difficulty hearing voices and sleep disturbances.
Conclusion
This case is first of the kind depicting clinical features as well as withdrawal of combined volatile and moderate alcohol abuse. The feature of combined intoxication of the two abused substances makes it difficult for the clinician to reach a diagnosis. Our case report thus puts forward the scenario of increasing combined alcohol and volatile substance abuse and growing problem of the same. Also, this case sensitizes physicians to think of substance abuse to be a complex presentation in the child. However, more exploration, case studies for assessing symptoms of intoxication and withdrawal in case of combined volatile and alcohol abuse are needed.
[1]. Mahal AS, Nair MC, Dependence on petrol – a clinical studyIndian J Psychiatry 1978 20:15-19. [Google Scholar]
[2]. Pahwa M, Baweja A, Gupta V, Jiloha RC, Petrol-inhalation dependence: a case reportIndian J Psychiatry 1998 40:92-94. [Google Scholar]
[3]. Basu D, Jhirwal OP, Singh J, Kumar S, Mattoo SK, Inhalant abuse by adoles-cents: a new challenge for Indian physiciansIndian J Med Sci 2004 58:245-49. [Google Scholar]
[4]. Verma R, Balhara YPS, Dhawan A, Inhalant abuse: An exploratory studyIndustrial Psychiatry Journal 2011 20(2):103-06.doi:10.4103/0972-6748.102493 [Google Scholar]
[5]. Seth R, Kotwal A, Ganguly KK, Street and working children in Delhi, India, misusing toluene: An ethnographic explorationSubst Use Misuse 2005 40:1659-79.[PubMed] [Google Scholar]
[6]. Shah R, Vankar GK, Upadhyaya HP, Phenomenology of gasoline intoxication and withdrawal symptoms among adolescents in India: A case seriesAm J Addict 1999 8:254-57.[PubMed] [Google Scholar]
[7]. Sadock BJ, Sadock VA, Substance-related disorders, inhalant-related dis-ordersIn: Kaplan and Sadock’s Synopsis of Psychiatry: Behavioural Sciences/Clinical Psychiatry10th edPhiladelphia [Google Scholar]
[8]. Joshi M, Vankar G, Gasoline abuse in a 10-year-old child with mental retardation: a case reportSubst Abuse 2015 Feb 12 9:5-8.doi: 10.4137/SART.S20148. eCollection 2015. PubMed PMID: 25733844; PubMed Central PMCID: PMC4332342 [Google Scholar]
[9]. Takagi M, Yücel M, Cotton SM, Verbal memory, learning, and executive functioning among adolescent inhalant and cannabis usersJ Stud Alcohol Drugs 2011 72:1-10. [Google Scholar]
[10]. Yucel M, Takagi M, Walterfang M, Lubman DI, Toluene misuse and long-term harms: a systematic review of the neuropsychological and neuroimaging litera-tureNeurosci Bio behav Rev 2008 32:910-26. [Google Scholar]
[11]. Gururaj G, Murthy P, Girish N, Alcohol related harm: Implications forpublic health and policy in India 2011 Publication No. 73Bangalore, IndiaNIMHANS [Google Scholar]
[12]. Ustun TB, The World Health Surveys. In: Murray CJL, Evans DB, edsHealth Systems Performance Assessment: Debates, Methods and Empiricism 2003 GenevaWorld Health Organization [Google Scholar]
[13]. Colman N, Herbert V, Haematologic complications of alcoholism: overviewSemin Haematol 1980 17:164-76. [Google Scholar]
[14]. Ramcharan K, Ramesar A, Ramdath M, Teelucksingh J, Gosein M, Encephalopathy and Neuropathy due to Glue, Paint Thinner, and Gasoline Sniffing in Trinidad and Tobago-MRI FindingsCase Rep Neurol Med 2014 2014:850109doi: 10.1155/2014/850109. Epub 2014 Jun 18. PubMed PMID: 25045557; PubMed Central PMCID: PMC4087279 [Google Scholar]
[15]. Xiong L, Matthes JD, Li J, Jinkins JR, MR imaging of "spray heads": toluene abuse via aerosol paint inhalationAJNR Am J Neuroradiol 1993 14(5):1195-99.PubMed PMID: 8237703 [Google Scholar]
[16]. Escobar A, Aruffo C, Chronic thinner intoxication: clinico-pathologic report of a human caseJ Neurol Neurosurg Psychiatry 1980 43(11):986-94.PubMed PMID: 7441282; PubMed Central PMCID: PMC490749 [Google Scholar]
[17]. Ehyai A, Freemon FR, Progressive optic neuropathy and sensorineural hearing loss due to chronic glue sniffingJournal of Neurology, Neurosurgery, and Psychiatry 1983 46(4):349-51. [Google Scholar]