Pathologic Surface Changes in the Submental Flap Used for Intraoral Reconstruction: Report of Two Cases
Amin Rahpeyma1, Saeedeh Khajehahmadi2
1 Associate Professor, Department of Oral and Maxillofacial Surgery, Oral and Maxillofacial Diseases Research Center, School of Dentistry, Mashhad University of Medical Sciences, Mashhad, Iran.
2 Assistant Professor, Department of Oral and Maxillofacial Pathology, Dental Research Center, School of Dentistry, Mashhad University of Medical Sciences, Mashhad, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Saeedeh khajehahmadi, Assistant Professor of Oral and Maxillofacial Pathology, Dental Research Center, School of Dentistry, Mashhad University of Medical Sciences, Mashhad, Iran.
E-mail: khajehahmadis@mums.ac.ir
Soft tissue reconstruction is often necessary after pathologic resection of oral squamous cell carcinoma. Although morphologic changes are common after transfer of the flaps to the oral cavity, pathologic changes within the transferred flaps, used for intraoral reconstruction, are rare events. Despite the widespread use of submental flap for oral cavity reconstruction, there are no reports in this respect. In this article, pathologic changes in the surface epithelium of transferred submental flaps are demonstrated with the report of two cases. The occurrence of lichen planus in a submental flap that had been used for reconstruction of lateral tongue border is reported in one case and in another patient, squamous cell carcinoma arising in the transferred de-epithelialized submental flap, used for maxillary and buccal reconstruction, is shown.
Oral cavity reconstruction, Squamous cell carcinoma, Surface epithelium
Case Reports
First Case
The patient was a 65-year-old edentulous female with squamous cell carcinoma (SCC) of the tongue (right lateral border) without cervical lymph node metastasis.
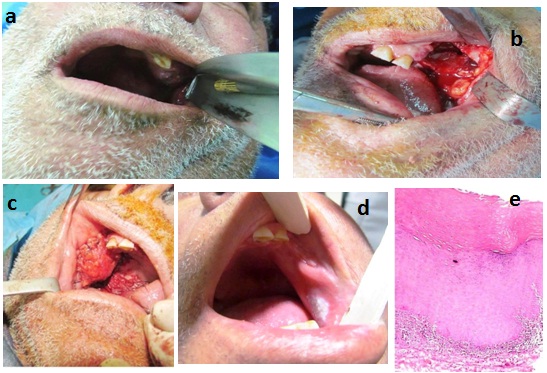
Orthograde submental flap was used for reconstruction after pathologic resection with wide margins [Table/Fig-1a]. A course of radiotherapy was advised by the oncologist. At the second-year follow-up, an erosive lesion was detected on the surface of the transferred flap [Table/Fig-1b]. In the excisional biopsy, it was compatible with lichen planus. Low-power photomicrograph showed hyperkeratosis, saw-toothed rete ridges and band-like infiltration of lymphocytes immediately subjacent to the epithelium [Table/Fig-1c]. There were no other signs of lichen planus in other parts of the oral cavity as well as any previous history of lichen planus. Two-year follow-up of the patient after excisional biopsy showed no signs of recurrence.
(a) Submental flap for reconstruction of the tongue lateral border. (b) Two years after engraftment an erosive lesion appeared. (c) Low-power photomicrograph shows hyperkeratosis, saw-toothed rete ridges and band-like infiltrate of lymphocytes immediately subjacent to the epithelium (H&E staining, original magnification ×100)

Second Case
The patient was a 55-year-old male with left maxillary and buccal squamous cell carcinoma [Table/Fig-2a]. Maxillary bone had been invaded by carcinoma. Size of the lesion was 5×3 cm [Table/Fig-2b]. Orthograde de-epithelialized submental flap was used for reconstruction after surgical resection with wide margins [Table/Fig-2c]. The flap uptake was uneventful. Six months after surgery, an elevated mucosal plaque with smooth, white and well-demarcated borders appeared on the cheek [Table/Fig-2d]. Administration of topical anti-fungal drugs for two weeks was not beneficial. The excisional biopsy revealed hyperkeratosis with a thickened spinous layer (acanthosis). The keratin layer consisted of a combination of hyperparakeratosis and hyperorthokeratosis. Numerous chronic inflammatory cells were noted within the subjacent connective tissue [Table/Fig-2e]. Nine months after the first surgery, an ulcer appeared in the retromolar region within the confines of the submental flap [Table/Fig-3a] that histologically was squamous cell carcinoma in incisional biopsy taken under local anaesthesia [Table/Fig-3b]. The lesion was resected with wide margins and reconstructed with a nasolabial flap [Table/Fig-3c,d].
(a) Pre-operative photograph showing ulcerative mass in the left edentulous maxillary ridge. (b) Maxillectomy defect and resected buccal mucosa. (c) De-epithelialized submental flap is used for reconstruction of buccal mucosa and maxillary alveolar ridge.(d) Buccal mucosa lesion with smooth, white and well-demarcated epithelialized flap.(e) High-power photomicrograph demonstrating hyperparakeratosis (on the left side) and hyperorthokeratosis (on the right side). A number of chronic inflammatory cells are noted within the subjacent connective tissue (H&E staining, original magnification ×400)
(a) Ulcerative lesion in the retromolar area. (b) Histopathologic feature of squamous cell carcinoma (H&E staining, original magnification ×100). A histopathologic feature of the keratotic lesion near the oral commissure was similar to the [Table/Fig-2e]. (c) Nasolabial flap was used for reconstruction after resection (One month after operation). (d) Flow up at six month shows uneventful flap uptake

In both cases, surgical margins in the main specimens were clean and adjunctive radiotherapy was administrated after surgery. None of the patients used tobacco (smoking or smokeless) and/or alcohol before and after surgery.
Discussion
After pathologic resection of oral squamous cell carcinoma (OSCC), soft tissue reconstruction is often necessary. Pedicled or free flaps are the most prevalent techniques for reconstruction of the resected lesion [1]. Pathologic changes within the transferred flap are uncommon [2]. Recurrence of the lesion, if any, often occurs in the interface between the flap and the remaining oral mucosa [3]. Despite the widespread use of submental flaps for oral cavity reconstruction, there is not any study describing the behaviour of this flap in situ. Studies in this topic are restricted to histologic changes in free or pedicled myocutaneous flaps (free radial forearm and pectoralis major flaps) used for intraoral reconstruction, which have shown that the transferred flaps maintain their architecture but are characterized by chronic inflammation in all the tissues and Candida infection in half of them [4,5].
Negative margins of the excisional biopsy specimen, boundary of the lesion within the flap and the superficial location, not reaching deep structures, all indicated that the pathologic changes were actually within the flap not from the bed or recurrence of the lesion in the adjacent oral mucosa. In the first case, these pathologic changes occurred in the transferred submental skin; in the second patient they happened after complete epithelialization of the raw surface of the flap that had been de-epithelialized before transfer to the oral cavity for prevention of hair problem in male patient.
The skin component of free or pedicled flaps, transferred to the oral cavity, shows some morphological changes as influenced by environmental factors, influenced by saliva, mechanical and chemical stimulus and Candida infection [6]. Epithelial changes such as psoriasis, focal acantholytic dyskeratosis and carcinoma are pathologic [7,8]. Pedicled pectoralis major myocutaneous flap, free radial forearm flap and skin grafts with pathologic changes after intraoral transfer have already been reported [9–11]. Two cases that were reported in this article are the first reports of pathologic changes in the submental flap.
The submental flap was introduced in 1993 and nearly two decades have elapsed since its introduction to the reconstruction world [12]. Ease of flap harvest, proximity to the oral cavity and large skin paddle are advantages of this flap [13]. It can be structurally classified into myocutaneous, fasciocutaneous and osteomyocutaneous [14]. The de-epithelialized variant is used in male patients with heavy beard to avoid the second surgery for hair removal or multiple sessions of laser application [15]. The difference between the second case in this article and the other reports of SCC developing in myocutaneous flaps, transferred to the oral cavity, is the time interval during which the second primary SCC had developed. Most second primary tumours have appeared several years after the initial tumour resection and reconstruction surgery [16]. This time was much shorter in the presented case in this article (9 months). De-epithelialized variant of submental flap used in this patient may have played an important role in this event. Raw surface of the flap exposed to the oral cavity for secondary epithelialization may be sensitive to oncogenes. Thin epithelium with persistent chronic inflammatory cells scattered beneath it (in fibrotic background) may be the other responsible factor.
Conclusion
Flap surface should be checked periodically for potential pathologic changes after transfer to the oral cavity. Some changes might have clinical importance. This checkup is more important in de-epithelialized variants. Skinless flap exposed to the oral cavity for secondary epithelialization and thin formed epithelium with persistent chronic inflammatory cells may have critical roles in this topic.
[1]. Rahpeyma A, Khajehahmadi S, Buccinator-based myomucosal flaps in intraoral reconstruction: A review and new classificationNational journal of maxillofacial surgery 2013 4:25-32. [Google Scholar]
[2]. Fyfe EC, Guest RG, St Rose L, Eveson JW, Focal acantholytic dyskeratosis arising in an intraoral skin flapInternational journal of oral and maxillofacial surgery 2002 31(5):560-61. [Google Scholar]
[3]. Pinto FR, de Matos LL, Palermo FC, Kulcsar MA, Cavalheiro BG, de Mello ES, Tumour thickness as an independent risk factor of early recurrence in oral cavity squamous cell carcinoma. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-LaryngologyHead and Neck Surgery 2014 271:1747-54. [Google Scholar]
[4]. Beahm EK, Evans GR, Colome-Grimmer MI, Histologic changes of intraoral free skin flapsAmerican journal of surgery 1997 174:492-94. [Google Scholar]
[5]. Bussi M, Valente G, Curato MP, Carlevato MT, Cortesina G, Is transposed skin transformed in major head and neck mucosal reconstruction?Acta oto-laryngologica 1995 115:348-51. [Google Scholar]
[6]. Rubino C, Dessy LA, Farace F, Ena P, Mazzarello V, Microscopic and immunohistochemical analysis of the skin changes of free forearm flaps in intraoral reconstructionAnnals of plastic surgery 2002 49:362-68. [Google Scholar]
[7]. Dimitrakopoulos I, Lazaridis N, Scordalaki A, Dermal psoriasis involving an oral split-skin graft. Case reportAustralian dental journal 1998 43(5):321-23. [Google Scholar]
[8]. Max Robinson C, Prime SS, Paterson IC, Guest PG, Eveson JW, Expression of Ki-67 and p53 in cutaneous free flaps used to reconstruct soft tissue defects following resection of oral squamous cell carcinomaOral oncology 2007 43:263-71. [Google Scholar]
[9]. Cymerman JA, Kulkarni R, Gouldesbrough D, McCaul JA, First report of squamous cell carcinoma arising within an intraoral radial forearm free flapInternational journal of surgery case reports 2013 4:731-34. [Google Scholar]
[10]. Montgomery WW, Varvares MA, Samson MJ, Goodman ML, Cutaneous squamous cell carcinoma occurring in a pectoralis major myocutaneous flap. Case report and literature reviewThe Annals of otology, rhinology, and laryngology 1993 102:206-08. [Google Scholar]
[11]. Sa’do B, Nakamura N, Higuchi Y, Ozeki S, Harada H, Tashiro H, Squamous cell carcinoma of the oral cavity derived from a skin graft: a case reportHead & neck 1994 16:79-82. [Google Scholar]
[12]. Rahpeyma A, Khajehahmadi S, Submental artery island flap in intraoral reconstruction: A reviewJournal of cranio-maxillo-facial surgery: official publication of the European Association for Cranio-Maxillo-Facial Surgery 2014 [Google Scholar]
[13]. Rahpeyma A, Khajehahmadi S, Reconstruction of the maxilla by submental flapANZ journal of surgery 2014 [Google Scholar]
[14]. Rahpeyma A, Khajehahmadi S, Onlay bone grafting simultaneous with facial soft tissue augmentation in a hemifacial microsomia patient using de-epithelialized orthograde submental flap: a technical noteAnnali di stomatologia 2014 5:30-3. [Google Scholar]
[15]. Rahpeyma A, Khajehahmadi S, Oral reconstruction with submental flapAnnals of maxillofacial surgery 2013 3:144-47. [Google Scholar]
[16]. Tokita R, Nagashio S, Shinohara A, Kurita H, Second primary squamous cell carcinoma arising in a skin flap: a case report and literature review on etiologic factors and treatment strategyJournal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons 2013 71:1619-25. [Google Scholar]