Introduction
Sedation is an essential component of the management of intensive care patients. It allows patient’s unawareness of the environment and reduction of discomfort and anxiety caused by procedures such as tracheal intubation, mechanical ventilation, suction and physiotherapy. Benzodiazepines like midazolam, propofol and opioids are among the agents commonly used for sedation in intensive care unit (ICU)[1-3]. Dexmedetomidine, an α2-adrenoceptor agonist, has also been approved for use as a short-term medication (<24 hours) for sedation in ICU.
Inadequate sedation can result in hypercatabolism, immuno-suppression, hypercoagulability and increased sympathetic activity that are associated with significant outcome impairment [4]. On the other hand, over sedation can increase time on ventilator support thereby exacerbating the risk of lung damage and neuromuscular alterations besides increasing ICU stay [5]. Sedation requirement also vary between patients, and among individuals throughout the course of their illnesses. Therefore continuous monitoring of sedation is essential.
Many clinical and instrumental tools for sedation monitoring have been proposed [6]. The clinical tools (e.g. Ramsay sedation scale) are subjective sedation scales, in which the patient is scored in relation to the response to the standard stimulus. But with these subjective scales distinction among different levels of sedation, especially at the deeper ones, is very difficult. Moreover, a great variability among physicians in applying stimuli and in evaluating responses is observed. Bispectral index (BIS), an objective monitoring modality, outcome these shortcomings of sedation scoring system and is now an accepted tool for the evaluation of effect of sedative drugs on central nervous system (CNS).
The present study aims to compare dexmedetomidine and propofol for sedation in ICU and also endeavour correlation between RSS and BIS.
Materials and Methods
The present prospective randomized patient-blinded study was carried out after obtaining institutional ethical committee approval and patient’s written informed consent. In all 60 haemodynamically stable patients, aged between 18 to 80 years divided into 2 groups of 30 patients each, requiring sedation and mechanical ventilation were given sedation for 12 hours. Pregnant females, excessive obesity (body weight over 50% above ideal body weight), severe hepatic, renal, or CNS involvement, significant arrhythmias or high degree of atrioventricular nodal block and patients who had allergies to drug were excluded from the study.
On arrival of the patients to ICU, baseline measurements including vital signs, 12- lead ECG, chest X-ray, blood samples (blood gases, haematology, and blood biochemistry), ventilation variables and APCHE II score were completed. They were instrumented with BIS™ 4 electrode sensor leads (fronto-temporal application). The BIS score was measured by means of BIS™ LoC 4-Channel OEM module (Covidien) with BIS VISTA™ Monitoring System (Aspect Medical Systems, Inc.). Only those measurement in which the SQI (Signal Quality Index) was between 80 to100 were considered.
After instrumentation ten minutes resting period was allowed for the baseline measurements.
The patients were allotted randomly to receive i.v. infusion of either of the two study drugs. Group A received dexmedetomidine at loading dose of 1 μg/kg over 10 min followed by a maintenance infusion of 0.5 μg/kg/hr (0.2-0.7 μg/kg/hr). Group B received propofol at loading dose of 1mg/kg over 5 min followed by a maintenance infusion of 2mg/kg/hr (1-3mg/kg/hr). Both the group of patients received fentanyl at 1 μg/kg prior to the study drugs. The degree of sedation was measured using Ramsay sedation score (RSS) and BIS. The BIS values were monitored continuously whereas RSS assessment was done hourly. Ramsay score was compared with the average of BIS values obtained 60 seconds before and after the stimulus application. In both the groups target was to achieve and maintain RSS of 4 or 5. The RSS of 4 represented asleep patients with basic response to glabellar tap or loud auditory stimuli whereas score 5 included patients with sluggish response to glabellar tap or loud auditory stimuli. If the aimed RSS level was not achieved or maintained by the study drug alone (dexmedetomidine at its maximum dose of 0.7 μg/kg/hr for 1 hour and propofol at its maximum dose of 3mg/kg/hr for 1 hour) then it was supplemented with 0.2mg/kg propofol bolus for maximum three successive boluses at an interval of 3 to 5 min. Even then if the desired RSS level was not achieved the case was labelled as failure.
After study drug initiation, vital signs (heart rate-HR, non invasive mean blood pressure-MAP, mechanical ventilation mode, inspired oxygen concentration (FiO2), positive end-expiratory pressure-PEEP) were monitored continuously and recorded at every 10 minutes interval during the first hour and thereafter every 60 minutes till the end of study. The ventilator settings, FiO2 and PEEP were adjusted according to ARDSnet ventilatory protocol. Inj. paracetamol 15mg/kg TDS was given for pain management in surgical patients. At the end of the study the BIS values in the study groups were correlated with RSS.
Statistical Analysis
The sample size was calculated with the help of medcalc software for statistical analysis. Based on assumption that there would be a 30% reduction in the mean heart rate following therapy, calculation yielded that sample size of 25 patients will be required in each group if results are to be significant (with α = 0.05 and power of 80%). Additional 5 patients were enrolled in each group taking into consideration potential exclusions later during the study.
Mean, Standard Deviation (SD) and Standard Error of Mean (SEM) were presented as descriptive statistics. Dichotomous outcomes were compared using Chi-square test. Student's t-test was used to compare numerical variables. Intragroup comparison was done using analysis of variance (ANOVA). Analysis was done using SPSS VERSION 17. The result were considered significant when p-value was <0.05.
Results
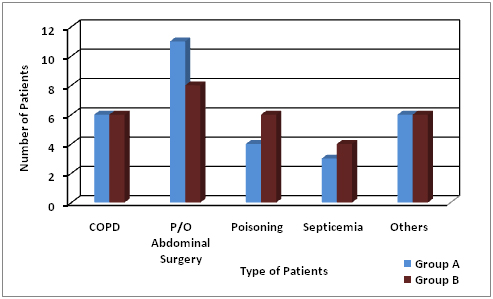
All the 60 patients completed the study. The demographic profiles of both the groups were comparable [Table/Fig-1]. These groups were also comparable with respect to baseline vital parameters and baseline investigations. The study groups included both surgical and medical patients [Table/Fig-2].
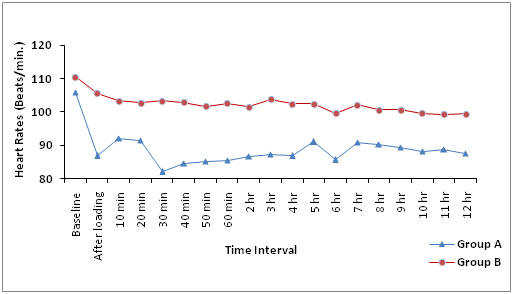
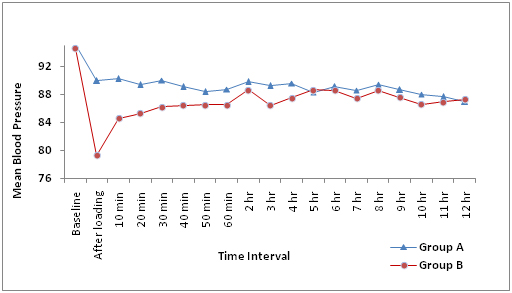
The comparison of baseline parameters of in two groups with values obtained subsequently lead to following observations. It revealed statistically significant difference in heart rate (HR) after loading dose (p<0.01) and at all times during sedation (p<0.05) with Group A (dexmedetomidine) patients having lower HR than Group B (propofol). The maximum drop in HR was seen at 30 min of infusion (p<0.001) [Table/Fig-3]. The mean blood pressure (MAP) showed statistically significant drop (p<0.01) following loading dose in propofol group. At rest of the time intervals no such differences were noted in MAP in either group [Table/Fig-4]. Both groups were comparable with respect to mean oxygen saturation, FiO2 and PEEP following loading dose.
The desired level of sedation was achieved in both the groups but patients receiving dexmedetomidine were aroused easily with adequate sedation when compared with patients receiving propofol. In Group A, out of 30 patients, 18 patients required rescue drug propofol whereas in group B only six patients required it. The Chi-square test gives p-value as 0.0398 (<0.05) which is statistically significant. Thus the use of rescue drug propofol was more in group A patients compared to Group B for achieving the desired RSS. It is also observed that 4 patients on dexmedetomidine developed bradycardia whereas none in propofol group. Bradycardia was responsive to intravenous inj. atropine 0.6mg.
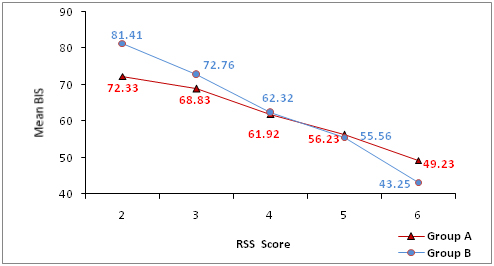
Correlation of Ramsay sedation score (RSS ) with BIS
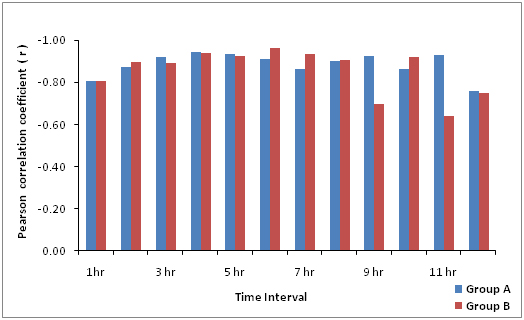
A total 720 Ramsay score (60 patients × 12 scores each) were obtained and compared with BIS values. The variation range in values of the Ramsay score was between 2 and 6. The BIS range varied from 39 to 97. We observed that with increase of the Ramsay scores there was a progressive decrease in the BIS scores [Table/Fig-5]. On applying the Pearson test we observed good and significant correlation between Ramsay score and BIS in both the groups; p-value <0.01 and average ‘r’ values of -0.88 in group A (dexmedetomidine) and of -0.85 in Group B (propofol) [Table/Fig-6].
Discussion
Sedation forms an integral component of bedside care for patients in the intensive care unit (ICU). Inadequate sedation techniques may have an adverse impact on the morbidity and mortality in ICU [7]. In fact the monitoring of depth of sedation has currently been considered as an emerging standard of care[8,9]. The employment of an objective method such as BIS, which give an immediate indication of the sedation level of the patient, could resolve shortcomings of subjective scoring systems namely the reproducibility and validity of results and the difficulty in interpretation of results. De Deyne C et al., [10], however in their study of depth of sedation observed a wide range in BIS values in patients sedated in ICU and had advocated further studies to find out applicability of BIS as monitoring modality to guide sedation. Thus there is a need for well-designed randomized trials comparing the effectiveness of available sedative agents as well as of sedation monitoring modality.
Hence, we conducted a prospective randomized control study to compare i.v. dexmedetomidine and i.v. propofol for sedation and haemodynamic stability in mechanically ventilated ICU patients as well as to compare BIS to RSS. No case was labelled failure in the study. The random sampling made the distribution of the patients in all groups comparable. There was even distribution of age groups in two groups. Therefore clinically insignificant variations in age simply helped us to alleviate these confounding factors like distribution metabolism, excretion and action of different drugs. Similarly, clinically insignificant variations in weight helped us to alleviating a point of controversy because obesity as well as cachexia has clinically significant effect on the clinical action of drug. The APACHE score and baseline investigations were comparable in both the groups. Both medical and surgical patients were enrolled in the study and there was no difference in type of patients admitted in the two groups. This consideration followed observation by Simmons LE et al., who in their study found that the correlation between subjective and objective scales varied in medical and surgical patients [11].
The baseline means HR was similar in both the groups. However, after loading dose, there was statistically significant (p-value <0.05) decrease in heart rate in dexmedetomidine group (86.83±26.28) compared to propofol group (105.60±19.51). During the entire period of sedation it was observed that patients sedated with dexmedetomidine had significant lower heart rate compared to patients sedated with propofol (p-value <0.05). Similar results were found by Esmaoglu A et al., Vinit K. Srivastava et al., and RM Venn et al., in their study comparing dexmedetomidine and propofol [12-14]. Decrease in HR can be attributed to sympatholytic and analgesic effects of dexmedetomidine [15].
We observed statistically significant fall in MAP following loading dose in propofol group. This observation was similar to Weinbroum AA et al., who observed that 68% of patients receiving propofol (p <0.001) had more than 20% decrease in systolic blood pressure after the loading dose {propofol 1.3 ± 0.2 mg/kg} [16]. Vinit K Srivastava et al., also observed reduction in MAP after propofol administration although the magnitude of fall in MAP was less [13]. This may be due to reduced rate of administration of loading dose of propofol in their study. Except for this period, values of MAP in both the groups in our study were comparable with statistically no significant difference (p-value >0.05). RM Venn et al., similarly in their randomized double blind study comparing dexmedetomidine with propofol found no differences in arterial pressure between the groups [14].
In our study the target of sedation was to keep the Ramsay sedation score at 4 or 5 in both groups. After loading dose we observed that the mean RSS in group A patients was 5 (5.03±0.66) and in group B was 4(4.6±0.62) with p-value <0.05, which is statistically significant. Thus we concluded that the desired level of sedation was achieved in both the groups. Despite adequate sedation Group A patients were aroused easily when compared with the Group B patients. These observations are also supported in a similar study by Richard R. Riker who found no difference in the time patients spent within the sedation target range with dexmedetomidine or propofol and an easy arousal in dexmedetomidine sedated patients [17].
We also observed that rescue drug propofol was used in 60% of patients in dexmedetomidine group for achieving the desired RSS compared to 20% patients in propofol group. This may be because easy arousability with dexmedetomidine may be likely to be misjudged as inadequate sedation on clinical examination.
It is observed that 13% patients develop bradycardia in dexmedetomidine group. The observations are supported by results of similar study by Richard R. Riker albeit with a higher incidence of bradycardia in dexmedetomidine group (42.2% {103/244} vs. 18.9% {23/122}; p<0.001) compared to propofol [17]. The greater proportion of patients with bradycardia may be due to higher dose of dexmedetomidine infusion (0.2-1.4 μg/kg/hr) used in their study. Further, all four patients in our study developed bradycardia after loading dose of dexmedetomidine. This finding is consistent with observations of Ickeringill M et al., who concluded that these undesirable haemodynamic effects can be avoided without compromising sedation by omitting the loading dose of dexmedetomidine [18].
A wide variation range in values of the Ramsay score and BIS was observed. But with increase of the Ramsay score there was an associated decrease in the BIS score. The average r-value of -0.88 and -0.85 with Pearson test in two groups separately (dexmedetomidine and propofol group respectively) proves that a good correlation exists between BIS values and Ramsay score and hence also verifies the applicability of BIS for monitoring sedation in ICU patients. Consales G et al., in their study found a similar correlation between the two scores [19]. The results are also in accordance to observations by Yaman F et al., who found a significant correlation between BIS and common sedation scales (RAS, SAS, RASS, AICES) [20].
Demographic characteristics in two groups
| Characteristics | Group | N | Mean | Std. Deviation | Std. Error Mean | Significance |
|---|
| Body weight | A | 30 | 67.20 | 12.15 | 2.70 | t-1.36 p>0.2 |
| B | 30 | 63.50 | 8.51 |
| Age | A | 30 | 43.30 | 20.25 | 3.68 | t-1.24 p>0.3 |
| B | 30 | 49.26 | 16.74 | 3.12 |
| APACHE Score | A | 30 | 16.13 | 3.81 | 0.70 | t-1.84 p>0.1 |
| B | 30 | 14.53 | 2.83 | 0.58 |
Type of patients in two groups
Mean heart rate at different time interval in two groups
| Time Interval | Group A | Group B | Significance |
|---|
| Mean | Standard Deviation | Mean | Std. Deviation |
|---|
| Baseline | 105.80 | 26.12 | 110.50 | 19.13 | t-.0.79 p>0.5 |
| After loading | 86.83 | 26.28 | 105.60 | 19.51 | t-3.140 p<.01 |
| 10 min | 92.03 | 21.98 | 103.43 | 18.01 | t-2.19 p<0.05 |
| 20 min | 91.46 | 20.84 | 102.83 | 17.66 | t-2.27 p<0.05 |
| 30 min | 82.03 | 21.29 | 103.43 | 17.57 | t-4.24 p<0.001 |
| 40 min | 84.70 | 20.86 | 102.96 | 17.62 | t-3.66 p<0.001 |
| 50 min | 85.16 | 21.22 | 101.66 | 17.29 | t-3.30 p<0.01 |
| 60 min | 85.53 | 22.31 | 102.66 | 18.72 | t-3.22 p<0.01 |
| 2 hr | 86.73 | 22.56 | 101.60 | 17.96 | t-2.82 p<0.01 |
| 3 hr | 87.40 | 22.63 | 103.76 | 17.52 | t-2.94 p<0.01 |
| 4 hr | 86.90 | 23.09 | 102.43 | 16.88 | t-2.97 p<0.01 |
| 5 hr | 91.03 | 24.25 | 102.43 | 17.15 | t-2.10 p<0.05 |
| 6 hr | 85.70 | 22.12 | 99.63 | 17.71 | t-2.69 p<0.02 |
| 7 hr | 90.83 | 23.42 | 102.23 | 15.59 | t-2.21 p<0.05 |
| 8 hr | 90.33 | 24.00 | 100.73 | 15.28 | t-2.00 p<0.05 |
| 9 hr | 89.40 | 24.76 | 100.73 | 15.36 | t-2.13 p<0.05 |
| 10 hr | 88.23 | 24.55 | 99.60 | 16.28 | t-2.11 p<0.05 |
| 11 hr | 88.73 | 24.32 | 99.33 | 15.60 | t-2.00 p<.05 |
| 12 hr | 87.56 | 23.92 | 99.53 | 16.24 | t-2.26 p<0.05 |
 |
Mean Blood pressure at different time interval in two groups
| Time Intervals | Group A | Group B |
|---|
| Mean | Std. Deviation | Std. Error Mean | Mean | Std. Deviation | Std. Error Mean |
|---|
| Baseline | 95.10 | 12.51 | 2.28 | 94.53 | 15.32 | 2.79 |
| After loading | 89.90 | 12.39 | 2.26 | 79.30 | 12.07 | 2.20 |
| 10 min | 90.16 | 14.14 | 2.58 | 84.56 | 16.20 | 2.96 |
| 20 min | 89.33 | 13.18 | 2.40 | 85.30 | 16.00 | 2.92 |
| 30 min | 89.93 | 12.59 | 2.29 | 86.16 | 14.99 | 2.73 |
| 40 min | 89.06 | 13.14 | 2.39 | 86.43 | 15.49 | 2.82 |
| 50 min | 88.30 | 12.21 | 2.23 | 86.50 | 15.89 | 2.90 |
| 60 min | 88.66 | 13.20 | 2.37 | 86.46 | 15.73 | 2.87 |
| 2 hr | 89.73 | 13.34 | 2.43 | 88.60 | 15.50 | 2.83 |
| 3 hr | 89.20 | 11.38 | 2.07 | 86.43 | 16.26 | 2.96 |
| 4 hr | 89.53 | 12.14 | 2.21 | 87.46 | 15.73 | 2.87 |
| 5 hr | 88.26 | 12.71 | 2.32 | 88.60 | 15.50 | 2.83 |
| 6 hr | 89.03 | 11.40 | 2.08 | 88.53 | 15.78 | 2.88 |
| 7 hr | 88.50 | 12.35 | 2.25 | 87.40 | 16.09 | 2.93 |
| 8 hr | 89.40 | 13.82 | 2.52 | 88.53 | 15.07 | 2.75 |
| 9 hr | 88.60 | 12.76 | 2.33 | 87.53 | 15.73 | 2.87 |
| 10 hr | 88.00 | 12.17 | 2.22 | 86.56 | 15.48 | 2.82 |
| 11 hr | 87.60 | 11.97 | 2.18 | 86.93 | 16.15 | 2.95 |
| 12 hr | 86.90 | 12.03 | 2.19 | 87.23 | 15.07 | 2.75 |
 |
Description of mean BIS for RSS score in two groups
| RSS | 2 | 3 | 4 | 5 | 6 |
|---|
| Groups | A | B | A | B | A | B | A | B | A | B |
| N | 12 | 17 | 49 | 46 | 166 | 177 | 103 | 103 | 30 | 17 |
| Mean BIS | 72.33 | 81.41 | 68.83 | 72.76 | 61.92 | 62.32 | 56.23 | 55.56 | 49.23 | 43.25 |
| Std. Devi-ation | 12.75 | 4.83 | 9.86 | 4.59 | 6.38 | 6.50 | 5.59 | 6.48 | 11.96 | 2.62 |
| Mini-mum | 42 | 74 | 41 | 63 | 40 | 51 | 39 | 45 | 38 | 38 |
| Maxi-mum | 84 | 90 | 84 | 84 | 82 | 97 | 75 | 86 | 82 | 47 |
 |
Correlation between RSS and mean BIS in two groups
Strengths of The Study
A major strength of our study was its design. It was a randomized controlled trial with adequate concealment of allocation. In our study, randomization was successful as the two groups were similar with regards to baseline demographic variables as well as for the various baseline investigations. We also recorded the need of rescue drug in both the groups which is absent in other similar studies. The study duration of 12 hours was well above most of the similar studies.
Limitations of The Study
The main limitation of the study is that it is a single center study. It also carries scope for comparing analgesia sparing effect of study drugs and also for study over longer duration of sedation.
Conclusion
We conclude that adequate level of sedation can be achieved by both dexmedetomidine and propofol. While dexmedetomidine-treated patients are easily arousable, the only notable adverse effect is bradycardia. The data obtained from the study validate BIS monitoring for ICU sedation. BIS monitoring can be useful in defining an appropriate sedation level in ICU patients while still maintaining the use of the scoring systems in care for ICU patient.
Acknowledgment
The authors sincerely acknowledge contribution of Dr. S.C. Paliwal (Msc. Tech., Ph.D., LL.B.) and Dr. Anamika Purohit (M.S. Obstetrics and Gynaecology) for their guidance and support in preparing this article.
[1]. Rowe Katherine, Fletcher Simon, Sedation in the intensive care unitContin Educ Anaesth Crit Care Pain 2008 8(2):50-55. [Google Scholar]
[2]. J Martin, M Franck, M Fischer, C Spies, Sedation and analgesia in German intensive care units: how is it done in reality? Results of a patient-based survey of analgesia and sedationIntensive Care Med 2006 32(8):1137-42. [Google Scholar]
[3]. Y Shehabi, JA Botha, MS Boyle, D Ernest, RC Freebairn, IR Jenkins, Sedation and delirium in the intensive care unit: an Australian and New Zealand perspectiveAnaesth Intensive Care 2008 36(4):570-78. [Google Scholar]
[4]. M Sydow, P Neuman, Sedation in critically illInt Care Med 1999 25:634-36. [Google Scholar]
[5]. CG Hughes, S McGrane, PP Pandharipande, Sedation in the intensive care settingClin Pharmacol 2012 4:53-63. [Google Scholar]
[6]. G Carrasco, Instruments for monitoring intensive care unit sedation.Crit Care 2000 4:217-25. [Google Scholar]
[7]. A Shafery, Complications of sedation with midazolam in the intensive care unit and a comparison with other sedative regimensCritical Care Med 1998 26:947-56. [Google Scholar]
[8]. J Jacobi, GL Fraser, DB Coursin, RR Riker, D Fontaine, ET Wittbrodt, Task Force of the American College of Critical Care Medicine (ACCM) of the Society of Critical Care Medicine (SCCM), American Society of Health-System Pharmacists (ASHP), American College of Chest Physicians. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adultCrit Care Med 2002 30(1):119-41. [Google Scholar]
[9]. JP Kress, AS Pohlman, MF O’Connor, JB Hall, Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilationN Engl J Med. 2000 342(20):1471-77. [Google Scholar]
[10]. M De Dyne Cstruys, Use of continuous Bispectral EEG monitoring to assess depth of sedation in ICU patients.Int care Med. 1998 24:1294-98. [Google Scholar]
[11]. LE Simmons, RR Riker, BS Prato, GL Fraser, Assessing sedation during intensive care unit mechanical ventilation with the Bispectral Index and the Sedation- Agitation ScaleCrit Care Med 1999 27(8):1499-504. [Google Scholar]
[12]. A Esmaoglu, A Ulgey, A Akin, A Boyaci, Comparison between dexmedetomidine and midazolam for sedation of eclampsia patients in the intensive care unit J Crit Care 2009 24(4):551-55. [Google Scholar]
[13]. VK Srivastava, S Agrawal, S Kumar, A Mishra, S Sharma, R Kumar, Comparison of Dexmedetomidine, Propofol and Midazolam for Short-Term Sedation in Postoperatively Mechanically Ventilated Neurosurgical PatientsJ Clin Diagn Res 2014 8(9):GC04-7. [Google Scholar]
[14]. RM Veen, Comparison between dexmedetomidine and propofol for sedation in the ICUBr J Anaesth 2001 87(5):684-90. [Google Scholar]
[15]. R Gertler, HC Brown, DH Mitchell, EN Silvius, Dexmedetomidine: a novel sedative-analgesic agentProc (Bayl Univ Med Cent) 2001 4(1):13-21. [Google Scholar]
[16]. AA Weinbroum, P Halpern, V Rudick, P Sorkine, M Freedman, E Geller, Midazolam versus propofol for long-term sedation in the ICU: a randomized prospective comparisonIntensive Care Med 1997 23(12):1258-63. [Google Scholar]
[17]. RR Ricker, Comparison of dexmedetomidine vs midazolam for sedation of critically ill patientsJAMA 2009 301:489-99. [Google Scholar]
[18]. M Ickeringill, Y Shehabi, H Adamson, U Ruettimann, Dexmedetomidine infusion without loading dose in surgical patients requiring mechanical ventilation: haemodynamic effects and efficacyAnaesth Intensive Care 2004 32:741-45. [Google Scholar]
[19]. G Consales, C Chelazzi, S Rinaldi, AR De Gaudio, Bispectral Index compared to Ramsay score for sedation monitoring in intensive care unitsMinerva Anestesiol 2006 72(5):329-36. [Google Scholar]
[20]. F Yaman, N Ozcan, A Ozcan, C Kaymak, H Basar, Assesment of correlation between bispectral index and four common sedation scales used in mechanically ventilated patients in ICUEur Rev Med Pharmacol Sci 2012 16(5):660-66. [Google Scholar]