Tobacco has numerous carcinogens and mutagens which have deleterious effects on human beings. Effect of carcinogens has been observed to be more on rapidly dividing cells which include germ cells. The maximum prevalence of smoking is observed in young adult males in the reproductive period [1]. Despite this, the undesirable effects of smoking on male reproductive health are less recognized and the impact of cigarette smoking on male fertility and sperm characteristics still remains controversial. Hence, this prospective study is undertaken to observe the effects of smoking on a few selected seminal fluid parameters like sperm count and motility and to compare the results with other similar studies.
Materials and Methods
The study was conducted in Fertility clinic, Adichunchanagiri Institute of Medical Sciences, B.G.Nagara, over a period of 1 year and including 20 non-smokers and 103 smokers in the age group between 25 to 40 years attending the primary infertility clinic who smoked a minimum of 10 cigarettes per day. They were categorized on the basis of duration of smoking as those smoking cigarettes for less than 5 years or for more than 5 years [Table/Fig-1].
Depicts entire study group
| Sl no. | Smoking history | Numbers | Percent |
|---|
| 1 | Non smokers | 20 | 16.3 |
| 2 | Smoking history less than 5 years | 42 | 34.1 |
| 3 | Smoking history more than 5 years | 61 | 49.6 |
| 4 | Total | 123 | 100.0 |
A detailed history including the duration and number of cigarettes smoked per day was elicited from the subjects. The subjects were instructed to observe three days of sexual abstinence since a longer period of abstinence reduces the sperm motility and a shorter period reduces the sperm count. The subjects were instructed to obtain the sample by masturbation making sure to include the first portion of the ejaculate since it is the most concentrated and contains the highest number of sperms. Condom collection was not entertained as it contains spermicidal agents. Ejaculation after coitus interruptus was also not preferred since it leads to loss of the first portion of ejaculate.
The entire ejaculate was collected in a clean, dry, sterile and leak-proof wide-mouthed plastic container in a collection room attached to the laboratory. Routine semen analysis was carried out under light microscopy according to the 5th edition of WHO laboratory manual for the examination and processing of human semen.
Following liquefaction of semen, the wet sample was first assessed by placing 10μl of semen onto a glass slide and covered with a coverslip. Approximately 200 spermatozoa in 5 fields at 200x magnification were counted for calculating the percentage of motility under three categories as progressive motility, non-progressive motility and immotility [2]. Sperm counting was then done by using modified Neubauer counting chamber. The total number of sperms was calculated by using the formula [2], Total Sperm Count = Number of sperms counted x 50,000/ml Semen samples from 20 non-smokers were also collected in a similar fashion for comparison.
Inclusion Criteria
TMen with primary infertility.
Aged between 25 to 40 years.
Exclusion Criteria
Subjects with occupational exposure to excessive heat and chemicals.
Subjects with undescended testis, varicocele, hydrocele and past history of surgery for their repair.
Subjects with chronic illnesses like diabetes mellitus, hypertension and tuberculosis.
Subjects on any type of long- term medication.
Results
Results of the study group is shown in [Table/Fig-1,2,3,4,5,6,7,8,9]. Five non-smokers showed sperm motility of less than 32%, the cause for which was not established. Obviously, the reduced sperm motility in this group was definitely not due to cigarette smoking since they were non-smokers. 71 smokers showed low sperm motility. Overall percentage of low motility was more in cigarette smokers than in non-smokers. Among 103 cigarette smokers, 31% had normal motility. The entire data was statistically significant as the p-value was less than 0.0001. In our study of 103 cigarette smokers, 25 subjects (20.3%) showed low sperm counts. The entire data was statistically significant as the p-value was less than 0.0001. Cigarette smoking was found to have a detrimental effect on both the sperm motility and the sperm count, but the effect on sperm motility was greater than that of sperm count.
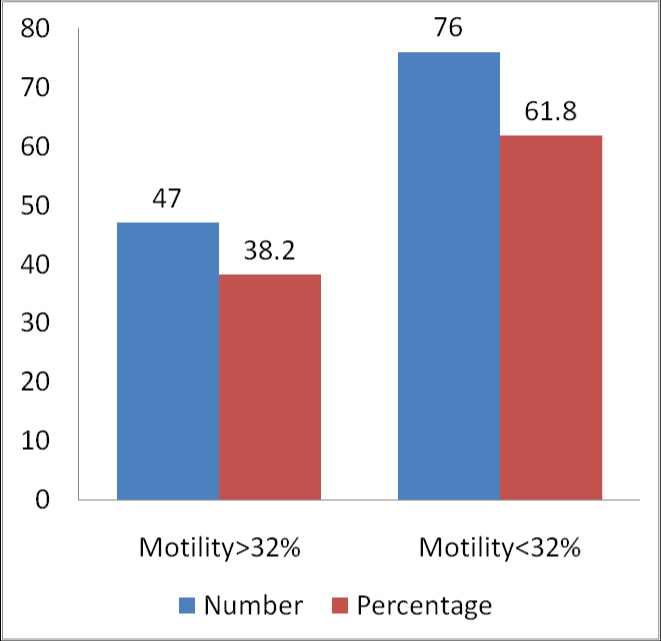
Sperm motility in the entire study group
| Sl no. | Motility | Frequency | Percent |
|---|
| 1 | Normal motility (greater than 32%) | 47 | 38.2 |
| 2 | Low motility (less than 32%) | 76 | 61.8 |
| 3 | Total | 123 | 100.0 |
Bar graph depicting sperm motility in the entire study group
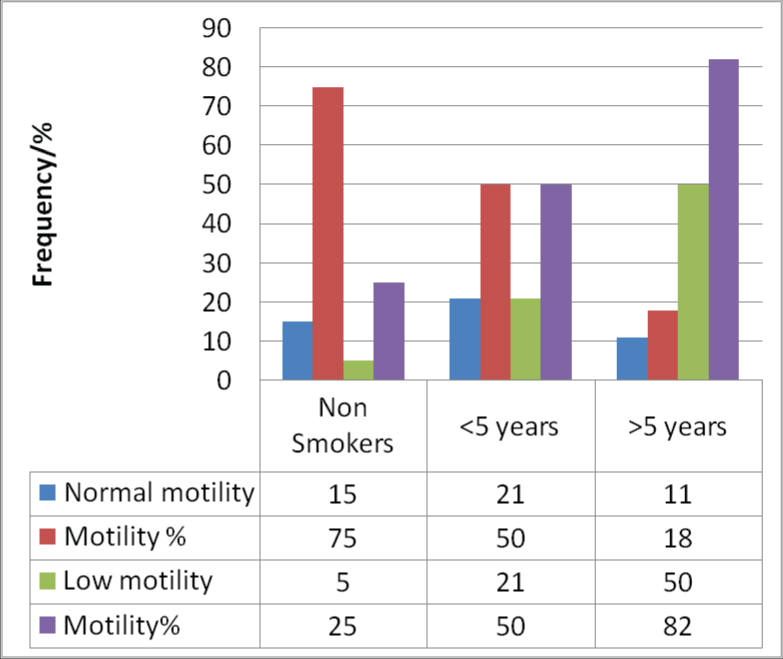
Comparative analysis of Sperm motility in Non-smokers and Smokers
| Sl no. | Smoking history | Sperm motility greater than 32% | Sperm motility less than 32% |
|---|
| 1 | Non smokers | 15(75%) | 5(25%) |
| 2 | Smoking history less than 5 years | 21(50%) | 21(50%) |
| 3 | Smoking history more than 5 years | 11(18%) | 50(82%) |
| 4 | Total | 47(38.2%) | 76(61.8%) |
Bar graph showing comparative analysis of Sperm motility in Non-smokers and Smokers. Statistical analysis of results pertaining to sperm motility by Chi square test p-value = 0.0001 Chi – square = 24.457 df = 2
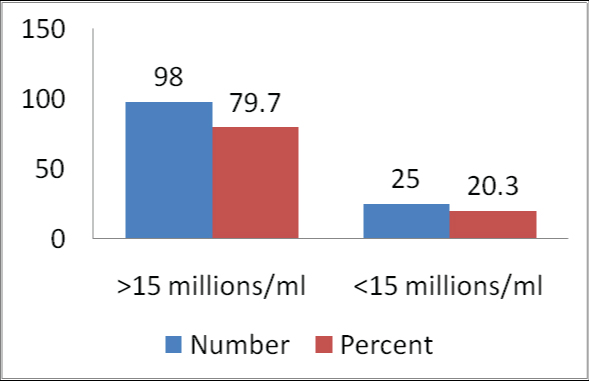
Sperm count in the entire study group
| Sl no. | Sperm Count (15 million/ml) | Frequency | Percent |
|---|
| 1 | Normal | 98 | 79.7 |
| 2 | Low | 25 | 20.3 |
| 3 | Total | 123 | 100.0 |
Bar graph depicting sperm count in the entire study group
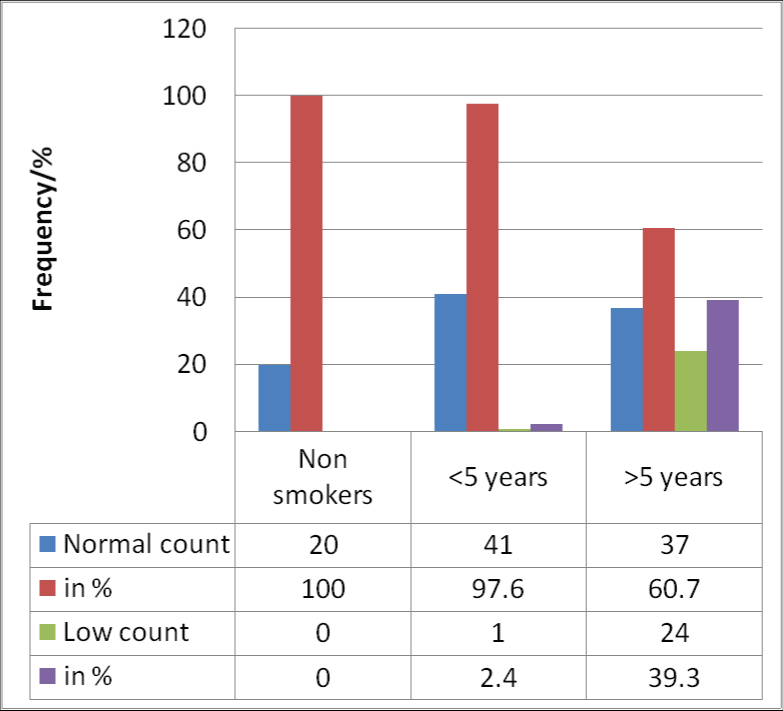
Comparative analysis of sperm count in non-smokers and smokers
| Sl no. | Smoking history | Normal count | Low count |
|---|
| 1 | Non smokers | 20(100%) | 0(0%) |
| 2 | Smoking history less than 5 years | 41(97.6) | 1(2.4%) |
| 3 | Smoking history more than 5 years | 37(60.7%) | 24(39.35%) |
| 4 | Total | 98(79.7%) | 25(20.3%) |
Bar graph showing comparative analysis of Sperm count in Non-smokers and Smokers.
Statistical analysis of results pertaining to sperm count by Chi square test
p-value = 0.0001 Chi – square = 27.079 df = 2
Discussion
Although the detrimental effects of cigarette smoking on all the seminal parameters have been proven by many studies, its effect on the individual parameters is yet to be established. Smoking causes increase in the concentrations of reactive oxygen species, cadmium and lead which affect sperm quality [3]. But in cases of a good primary testicular function it may mask or compensate the free radical injuries. The effectiveness of spermatogenesis is measured by sperm count. But sperm motility indicates epididymal maturation and sperm functional capability [4]. Sperm motility is attributed to its tail which is composed of flagella. The energy required for the movement is provided by the mid piece which is rich in mitochondria [5]. Motility is vital in normal functioning of sperm, as it not only helps in transportation but also helps in penetrating the outer layers of ovum for fertilization [6]. Hence, the sperm motility can be considered as the most important factor influencing fertility.
According to previous research, it has been demonstrated that, mammalian sperm must remain motile in the female genital tract and free energy released from the hydrolysis of ATP is required for this movement [7]. Zavos et al., have reported reductions in sperm motility associated with abnormalities in the ultrastructure of the flagellum and the axonemal structures of the sperm tail [8]. Garrett et al., have concluded in their study that pregnancy rates increase with superior sperm morphology and motility [9].
The present study showed decreased sperm motility and sperm count in cigarette smokers which was more evident in those with a smoking history of more than 5 years [Table/Fig-2,3,6,7]. Out of the 103 subjects, 25 had low sperm count whereas 71 had low sperm motility [Table/Fig- 4-7]. On comparing these two parameters, it was observed that the sperm count was less affected than the sperm motility. Zakarya Bani Meri et al., showed that there was a significant decrease in sperm concentration among heavy smokers as compared to the light smokers. They concluded that, cigarette smoking has a deleterious effect on some of the seminal fluid parameters like motility, morphology and leukocyte count which may in turn result in male subfertility [10]. Farkhunda Nadeem et al., identified the potential hazardous chemicals present in cigarette smoke which may cause sperm abnormality by affecting the chromosomes. They opined that, smoking can decrease male fertility by decreasing the sperm motility and percentage of normal sperm cells, and that a decrease in the percentage of motility of sperm cells and normal morphology is correlated with the number of cigarettes smoked per day [11]. This is in concurrence with our study as well as the studies by Shaaraway M et al., Vytas Kaulikauskas et al., Vogt et al., Hughes ED et al, Vine MF et al., Alexander E et al., Al Bader A et al., S.Sinclaire, Arabi M and Somwanshi et al., [12–21]. In striking contrast to our observations and all the other studies, the study by Azar Aghamohammadi et al., opined that cigarette smoking does not appear to adversely affect sperm parameters since there was no significant difference in sperm quality in smokers except for semen volume and total sperm count. However, they concluded quitting smoking is clearly beneficial in terms of enhancing general health and more research is necessary to evaluate its role in male fertility [22].
Conclusion
Most men with no proven cause for infertility are known smokers. The vital seminal parameters which play a major role in male fertility like sperm motility and sperm count are decreased due to smoking and show a further decline with continuation of smoking for more than five years.