Effectiveness of Intensive Interactive Classes and Hands on Practice to Increase Awareness about Sharps Injuries and Splashes among Health Care Workers
Nonika Rajkumari1, Purva Mathur2, Jacinta Gunjiyal3, Mahesh Chandra Misra4
1 Assistant Professor, Department of Microbiology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India.
2 Additional Professor, Department of Laboratory Medicine (Microbiology Division), Jai Prakash Narayan Apex Trauma Centre, All India Institute of Medical Sciences, New Delhi, India.
3 Nursing-in-Charge, Hospital Infection Control, Hospital Infection Control Unit, Jai Prakash Narayan Apex Trauma Centre, All India Institute of Medical Sciences, New Delhi, India.
4 Professor, Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nonika Rajkumari, Assistant Professor, Department of Microbiology, 2nd Floor, Institute Block, JIPMER, Dhanvantri Nagar, Puducherry - 605006, India.
E-mail: nonika.raj@gmail.com
Background
Occupational exposure to sharps and splashes pose a major hazard among health care workers (HCWs); so knowledge and awareness regarding sharps/splashes by blood and potentially infectious body fluids (BBF) is a must. Hence, the study was done to assess the extent of knowledge of the staff and using awareness classes and hands on practice as a model to increase awareness as well as prevention.
Materials and Methods
This prospective interventional cohort study, using before – after trial, was conducted in a Level I trauma care centre. All cadres of HCWs were enrolled randomly into 5 different groups of 15 each. This study was conducted in 2 phases – interactive classes and hands on practice (Phase I) and questionnaire assessment and work area observation (phase II). This was repeated twice and the final outcome was analysed. A systematic level of grading was used to assess the improvement.
Results
It was observed that Group 1 (doctors) and group 2 (nurses) had the maximum knowledge about such exposures and its prevention compared to the other groups (groups 3, 4 and 5) during the initial assessment (Phase I). The remaining groups showed a major improvement after the 2nd assessment, though their knowledge was poor in the beginning. Groups 1and 2 showed 32% and remaining groups showed a 25% improvement in voluntary reporting after the second assessment (Phase II).
Conclusion
Awareness classes and hands on practice are indeed useful in generating knowledge about sharps/ splashes. Certain incentives given at right time can improve it further.
Awareness, Health care workers, Interactive classes, Needlestick injuries, Prophylaxis, Voluntary reporting
Introduction
Needle & sticks/sharps injuries (NSI) and splashes by blood and infectious body fluids (BBF) are a major occupational hazard among healthcare workers (HCWs) in trauma care set ups. Workers in the trauma care profession are especially prone to sharps-related injuries and splashes, as sharps including needles are the commonly used things during surgical procedures. NSIs and splashes are a hazard in regard to transmission of infectious blood borne diseases, among them hepatitis B and C viruses and HIV [1]. HCWs and students are at risk of injuries during daily procedures such as vein puncture or sewing [2–4]. There is a high risk of experiencing a potentially infectious injury or splash of blood or body fluid during work hours [2,5–7].
The prevalence of hepatitis B and C viruses and HIV among hospitalized patients is many times higher than in the general population [8], and hence such exposures should be taken seriously. Previous studies have demonstrated a lack of risk awareness and a high underreporting rate among medical staff and undergraduate medical students [3,4] including high rate of unreported exposures [5,6,9–11]. Factors like lack of risk awareness, lack of time, and ignorance of the reporting system as well as trivialization by superiors and shame have been evaluated as possible reasons for under-reporting [5,9]. The Directive 2010/32/EU “Prevention from sharp injuries in the hospital and healthcare sector”, issued to protect workers from these risks, requires an integrated approach to prevention including awareness-raising, education, training, elimination of unnecessary needles, safe procedures for sharps use and disposal, banning of recapping, vaccination, use of personal protective equipment, provision of safety-engineered devices, and appropriate surveillance, monitoring, response and follow-up [12]. NSIs were defined as injuries with needles or other sharp instruments that were contaminated with potentially infectious patient material [1,12].
All the staff including those in the clinical area and those working in the laboratories of the hospitals also comes under the high risk settings both in the pre-analytical as well as the post analytical settings [13]; knowledge and awareness regarding NSI/sharps as well as splashes by blood and potentially infectious body fluids (BBF) is a must. Similar findings were also observed among those staff who was involved in hospital cleaning and biomedical waste disposal. A study has also emphasised the necessity to educate or create awareness among all the HCWs including those staff like waste disposal staff and laboratory technicians who are not directly involved in patient care but are nevertheless exposed to such risk [14].
A trauma centre represents a busy, surgical emergency health set-up, with risk of such exposures to the HCWs. Only few studies have been done to explore the awareness of such exposures and the improvement in their knowledge about NSIs/ sharps and splashes exposures in trauma-based set-ups. Such study will help in determining the baseline knowledge of such exposures through classes and assessments of different HCWs including comparability of level of knowledge about such injury and splashes to body fluid. This will also help in preventing avoidable exposures and what to do if such an exposures occurs in different HCWs of the hospital and may also help to set up rules in high risk areas.
A study conducted in JPNATC, AIIMS among voluntarily reported NSIs and splashes exposures found that besides doctors (36.2%) and nurses (14.6%), hospital waste disposals staff also faces high exposure (7.6%) to NSIs and splashes as well as rate of underreporting was high (51.1%) [15]. Hence, due to this magnitude of the problem and to create more awareness and find a way to reduce the problem, this study was conducted prospectively.
Aim
To assess the usefulness of classes in HCWs in improving the knowledge of needle stick and sharps injuries including testing of their current knowledge and management of such exposures in an apex trauma care centre of India.
To evaluate the staff awareness of effective and correct practices of NSIs/ sharps injuries and splashes at all stage: generation, segregation, destroying, treatment & disposal and also management of such exposed HCWs at a Trauma Center in New Delhi. The study also tried to evaluate their exposure reporting practices including the post-exposure prophylaxis measures.
Materials and Methods
The study was performed at a Level I Trauma Centre, New Delhi catering to a reference population of 16.3 to 17.8 million inhabitants during the study period. It has 176 functional beds with an average total admission per year of 5,914 during the study period. The Institute’s hospital infection control team consist of 4 microbiologists and 7 nurses. All protective equipments like heavy duty gloves, needle cutter at every station, sharps containers, coloured coded waste bins and well as round the clock sharps and splashes reporting and blood testing facility are provided in the hospital.
Facilities provided to the HCWs for sharps and splashes reporting include:
Round the clock voluntary reporting facility of an exposure to any health care workers.
A Microbiology Senior Resident and a Hospital Infection Control nurse are especially assigned for this work.
Round the clock testing for any blood borne viral infections with immediate information regarding the test results.
Back tracing of any exposure of any HCW if they fail to report.
A defined proforma is filled up for any exposed staff and such staffs are followed up for 6 months.
Any HCWs exposed to any positive source of HIV is referred to the AIIMS HIV cell for emergency prophylaxis and medicines to be given accordingly.
Any HCW exposed to a HBV positive source were asked their vaccination history and given Immunoglobulin and Hepatitis B vaccination accordingly.
A total of 75 HCWs irrespective of the gender, who were working in various departments of the Trauma Center, were enrolled for the study. It was performed for a period of 4 months from January, 2014 to April, 2014. They were divided into 5 different groups: (1) Group 1(Doctors), (2) Group 2(Nurses), (3) Group 3(Hospital attendants), (4) Group 4 (Hospital cleaning staff and waste disposal staff) and (5) Group 5(Laboratory technicians). Each group consisted of randomly selected 15 members. These HCWs were enrolled randomly on a voluntary basis and only their work area and their work position were noted (Doctors, nurses, attendant etc.). They were first divided into the above 5 groups and their inclusion in the study groups were decided by draw of lots. In each of the group, the volunteers were given a number each and a second unrelated person picked up 15 volunteers in each group by picking up chits with the number written on it.
All the HCWs were explained about the procedure and those who wished to participate voluntarily were included after taking their informed consent. They were explained that it will not affect their duties on a routine basis.
It was conducted after dividing the period into two phases: (1) Classes and workshops and (2) Assessments and observation on how much improvement can be seen in the management of NSIs/sharps and splashes exposure. Classes were conducted twice in the months of January and then again in March, 2014 along with hands on practice. Classes were conducted separately for each group of HCWs via interactive lectures, audio-visual aids and hands on practice through role playing in the class rooms and in their respective areas of work. Assessments were done at the end of the month of February, 2014 after the first set of classes and hands on practice though questionnaire and also by verbally asking them. This was again repeated at the end of April, 2014 after the second set of classes conducted in March, 2014. The changes and improvements were noted and assessed.
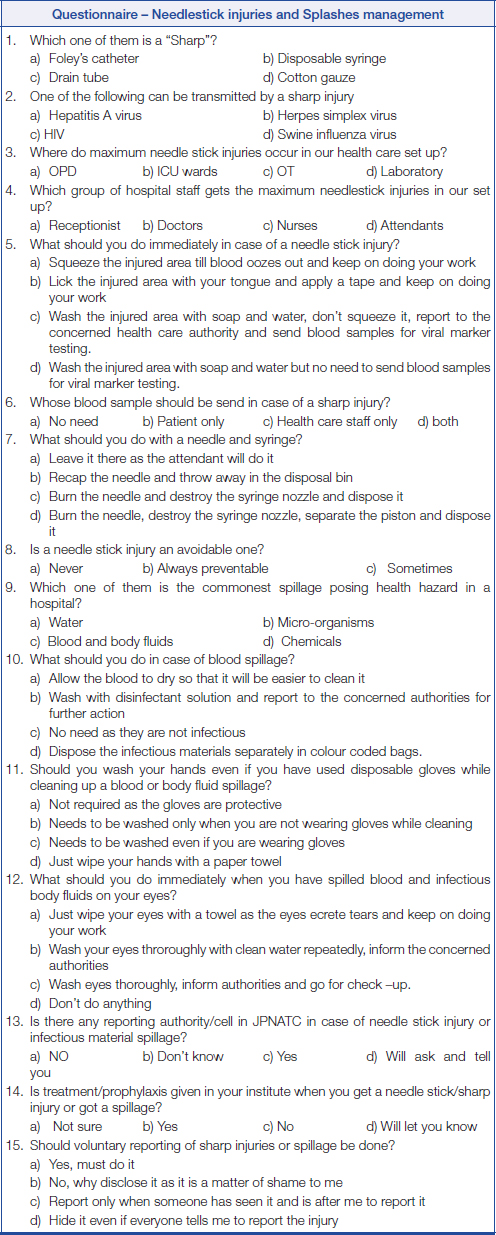
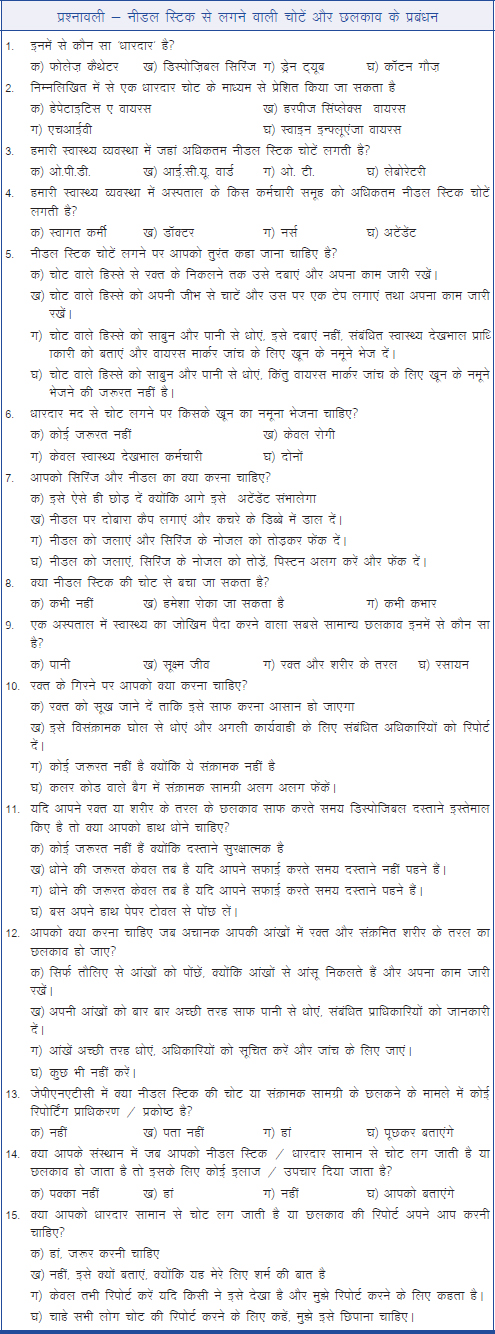
An anonymous questionnaire of 15 questions concerning NSIs/splashes among medical health workers was designed. It was evaluated by a team of Microbiologists and Hospital Infection Control Staff who are specialized in NSIs/sharps injuries and splashes and was piloted in different groups of HCWs. The questionnaire was made both in English and Hindi languages for easy comprehension among different health care staff [Table/Fig-1,2]. The questionnaire was given to each HCW before the starting and after the end of each class and hands on practice was conducted at the Center. In this way, it was ensured that participants were assessed of how much knowledge each had before such a class and how much they gained after the end of each session. The questionnaire content was determined based on the literature and the analysis of the existing injury reports at the facility as discussed below. The questionnaire concerned 5 basic topics: (1) Rate of NSIs and splashes; 2) circumstances and risk factors for NSIs and splashes; 3) reporting behaviour; 4) present knowledge and their suggestions; and 5) personal data.
Testing and management according to the National AIDS Control Organization of India (NACO) guidelines were also explained to them [16]. NSI and sharps injuries were listed separately and explained how to manage and report when such an exposure occurred. Other exposures, such as mucosal contacts, for example blood splashes into the eyes, as well as wound contacts were also explained to them.
The HCWs were assessed at the end of February and April, 2014 regarding their knowledge and what to do when such an exposure occurred and mistakes like incorrect managing of the wound when exposed, improper sharps disposals etc were explained to them including its proper correction. The improvement between the 2 assessments was compared.
All the questionnaires were given before and after the classes and their knowledge assessed based on point system on the correct answers they gave in the questionnaires and how they managed when such an exposure occurred in their areas of work. This was assessed by non-informed, anonymous visits by one HICN or a Microbiology Senior resident. They observed the performances of these HCWs in their work area and then subsequent scoring was done. One point was given for every correct answer and for each HCW; the points were tallied and noted. The level of correct answers and observations were divided into 3 cut off levels [Table/Fig-3]. Also, comparison was done on how much benefit was obtained by each group of HCWs at the end of each class and between the first and second set of classes.
Level of knowledge was assessed based on the cut off as above for each group
| Number of correct questions answered by the HCWs | Level of knowledge |
|---|
| < 7 questions | Level 1 |
| >7 questions but <10 questions | Level 2 |
| >10 questions but ≤ 15 questions | Level 3 |
Results
It was observed that Group 1 (doctors) and group 2 (nurses) had the maximum knowledge about such exposures and how to prevent it compared to the other groups (groups 3, 4 and 5) during the initial assessment. After the classes and hands on practice, it was observed that all the groups showed significant changes and improvement in their knowledge and implementation in their day to day practices regarding how to avoid such injuries and exposures and what to do in case of such accidental exposure. The details are shown in [Table/Fig-4,5]. [Table/Fig-4] showed that groups 3 and 4 showed no improvement after the classes and notable changes could be seen only after the second assessment which was an important finding. Also, the teaching pattern may not be the same among the professional group of workers and hence outcome was bound to be different in different groups. It was also noted that the retention and effect may vary in long term.
Comparison between the various groups of health care workers in their knowledge and application before and after the awareness classes (first assessment – January – February’14)
| Theoretical | Practical implementation in their work areas |
|---|
| Groups | Before classes/hands on practice | After classes/hands on practice | Improvement (%) | Before classes/hands on practice | After classes/hands on practice | Improvement (%) |
|---|
| Group 1 (Doctors) | Level 2 | Level 3 | 80% | Level 1 | Level 2 | 50% |
| Group 2 (Nurses) | Level 2 | Level 3 | 80% | Level 1 | Level 2 | 50% |
| Group 3 (Hospital Attendants) | Level 1 | Level 2 | 50% | Level 1 | Level 1 | 0 |
| Group 4 (Hospital cleaning staff and waste disposal staff | Level 1 | Level 2 | 50% | Level 1 | Level 1 | 0 |
| Group5 (Laboratory technicians) | Level 1 | Level 2 | 50% | Level 1 | Level 2 | 50% |
Comparison between the various groups of health care workers in their knowledge and application before and after the awareness classes (second assessment – March – April’14)
| Theoretical | Practical implementation in their work areas |
|---|
| Groups | Before classes/hands on practice | After classes/hands on practice | Improvement (%) | Before classes/hands on practice | After classes/hands on practice | Improvement (%) |
|---|
| Group 1 (Doctors) | Level 3 | Level 3 | 95% | Level 3 | Level 3 | 95% |
| Group 2 (Nurses) | Level 3 | Level 3 | 95% | Level 3 | Level 3 | 95% |
| Group 3 (Hospital Attendants) | Level 2 | Level 3 | 80% | Level 2 | Level 3 | 80% |
| Group 4 (Hospital cleaning staff and waste disposal staff | Level 1 | Level 2 | 50% | Level 2 | Level 3 | 80% |
| Group5 (Laboratory technicians) | Level 2 | Level 3 | 80% | Level 2 | Level 3 | 80% |
Level 1: < 7 correct questions/procedures, Level 2 : > 7 but <10 correct questions/procedures, Level 3: >10 but ≤ 15 correct questions/procedures
Groups 1 and 2 performed very well in both the classes and in their practical implementation after the awareness classes/hands on practices and even showed more improvement after the second assessment in their work areas. However, the other groups (groups 3,4 & 5) had average knowledge at the beginning of the awareness classes (Level 1) but a dramatic improvement was seen in them after the end of the first assessment regarding their practical outcomes. The rate of voluntary reporting among them has also increased to 20% after the end of first assessment and by 25% after the end of the second assessment. The rate of voluntary reporting was low (10%) among groups 1 and 2 though they had practically implemented well in their work areas after the end of first assessment; but by the end of second assessment, it had improved up to a level of 32%.
In the study, awareness classes and hands on practice were found to be very useful in spreading awareness and improving the knowledge to combat the problem of NSI/sharps and splashes exposures.It should be implemented routinely among the various HCWs along with compulsory hepatitis B virus vaccination.
Discussion
It was seen that groups 1 and 2 had the maximum knowledge about the exposure and its prophylaxis compared to the other groups in our study. This finding showed that knowledge had a significant relationship with the level of education as well as those attending sharps exposure and prevention classes regularly. Similar finding was seen in another study conducted among dentists who also falls under the high risk of sharps injuries [17]. In our study too, it was observed that doctors and nurses have the highest exposure rate which was also seen in another study from Germany [2]. Our study showed an increase in the performance level in their work place in all the groups but the significant improvement was seen among those in groups 3,4 and 5 after phase II compared to those of groups 1 and 2 since the beginning. Also, voluntary reporting improved up to 32% among these groups (3, 4 and 5). These findings also reflect what was seen in another study done using only questionnaire and practical implementation after their study [18].
The study observed that level of education is related to more awareness about such exposures and what is the prophylaxis available but it does not necessarily mean that it is practised. The other groups like hospital attendants, laboratory technicians though did not have much knowledge in the beginning of the study, but they picked up quickly regarding what is to be done correctly to avoid exposures and how to go for voluntary reporting in case of exposure. Creating such awareness classes and practical hands on experience helps to create awareness in a step wise fashion too. Those who had enrolled in this study went and practised themselves and also acted as guide and mentored others to do the right practice to avoid injuries and to report and receive prophylaxis in case of exposure thereby compounding the benefit of the awareness classes and hands on practice.
This study also tried to look into the problems faced by the HCWs while actually performing their duties which can cause the exposure so that health care intervention policy can be chalked out and implemented later. This study tried to instil in the health care workers that care of their health lies in their hands and the authorities have given them all the facilities and only this can be availed if they promptly and voluntarily report such exposures and are aware of it. Our study tried to explore short term but intensive interactive classes with hands on practice and graded the improvement both through questionnaire as well as the improvement in work area and reduction in injuries and voluntary reporting. Other studies just used either a questionnaire survey or just assessment of the awareness of injuries among HCWs.
Limitations of the Study
The study was conducted in just one series using 75 HCWs only. A larger number of HCWs could have provided a more streamlined view but this was not possible due to the shift duties of the staff or due to work constrains. Immediate post education showed an improvement in our study and as was expected. A reassessment after a period of time is required to ascertain if this improvement is sustained.
Future Prospective
This can also be managed by providing certain incentives to different HCWs in various work areas like giving an award for the NSIs/sharps and exposure free section or a particular area in the hospital. Encouraging proper disposal and segregation of such sharps so that staff who are not directly involved in the patient’s health care does not get such an exposure accidentally. Encouraging and making Hepatitis B vaccination mandatory.
Encouragement of routine awareness classes among all the HCWs and especially among those newly inducted staff. Safety protocol drills by each respective section in charge on a monthly basis so that such a habit gets ingrained in the health care workers and to avoid preventable injuries. Awareness classes should be included in the medical students as well as the staff training classes too as a part of their studies curriculum.
Conclusion
Awareness classes along with hands on experience has provided an encouraging improvement in the NSIs/sharps exposure management and hence must be incorporated as a routine practice, supplemented with timely incentives.
Level 1: < 7 correct questions/procedures, Level 2 : > 7 but <10 correct questions/procedures, Level 3: >10 but ≤ 15 correct questions/procedures
[1]. Lauer AC, Reddemann A, Meier-Wronski CP, Bias H, Gödecke K, Arendt M, Needlestick and sharps injuries among medical undergraduate studentsAm J Infect Control 2014 42:235-39. [Google Scholar]
[2]. Wicker S, Jung J, Allwinn R, Gottschalk R, Rabenau HF, Prevalence and prevention of needlestick injuries among health care workers in a German university hospitalInt Arch Occup Environ Health 2008 81:347-54. [Google Scholar]
[3]. Wicker S, Ludwig A-M, Gottschalk R, Rabenau HF, Needlestick injuries among health care workers: occupational hazard or avoidable hazard?Wiener Klinische Wochenschrift 2008 120:486-92. [Google Scholar]
[4]. Blitz J, van Rooyen M, Cameron D, Using an audit of medical student behaviour to inform curriculum changeTeach Learn Med 2010 22:209-13. [Google Scholar]
[5]. Salzer HJ, Hoenigl M, Kessler HH, Stigler FL, Raggam RB, Rippel KE, Lack of risk-awareness and reporting behavior towards HIV infection through needlestick injury among European medical studentsInt J Hyg Environ Health 2011 214:407-10. [Google Scholar]
[6]. Wicker S, Nürnberger F, Schulze JB, Rabenau HF, Needlestick injuries among German medical students: time to take a different approach?Medical Educ 2008 42:742-45. [Google Scholar]
[7]. Hofmann F, Needlestick injuries in health care: frequencies, causes and preventive strategiesGesundheitswesen 2002 64:259-66. [Google Scholar]
[8]. Wicker S, Cinat J, Berger A, Doerr HW, Gottschalk R, Rabenau HF, Determination of risk of infection with blood-borne pathogens following a needlestick injury in hospital workersAnn Occup Hyg 2008 52:615-22. [Google Scholar]
[9]. Sharma GK, Gilson MM, Nathan H, Makary MA, Needlestick injuries among medical students: incidence and implicationsAcad Med 2009 84:1815-21. [Google Scholar]
[10]. Varsou O, Lemon JS, Dick FD, Sharps injuries among medical studentsOccup Med (Oxford) 2009 59:509-11. [Google Scholar]
[11]. Moon CS, Hwang JH, Lee CS, Park KH, Kim ES, Exposure to blood and body fluid among medical students in KoreaAm J Infect Control 2010 38:582-83. [Google Scholar]
[12]. Council of the European Union Council Directive 2010/32/EU of 10 May 2010 implementing the Framework Agreement on prevention from sharp injuries in the hospital and healthcare sector concluded by HOSPEEM and EPSUOfficial Journal of the European Union 2010 L 134(53):66-72.Available at: http://eur-lex.europa.eu/LexU-riServ/LexUriServ.do?uri=OJ:L:2010:134:0066:0072:EN:PDF. Accessed May 2, 2014 [Google Scholar]
[13]. De Carli G, Abiteboul D, Puro V, The importance of implementing safe sharp practices in the laboratory settings in EuropeBiochem Med (Zagreb.) 2014 24:45-56. [Google Scholar]
[14]. Alavian SM, Comments on behaviour of health care workers after injuries from sharp instrumentsTrauma Mon 2014 19(1):e17040 [Google Scholar]
[15]. Rajkumari N, Thanbuana BT, John NV, Gunjiyal J, Mathur P, Misra MC, A prospective look at the burden of sharps injuries and splashes among trauma health care workers in developing countries: True picture or tip of icebergInjury 2014 45:1470-78. [Google Scholar]
[16]. Guidelines for HIV testing. National AIDS Control Organisation website. http://nacoonline.org/About_NACO/Policy__Guidelines/Policies__Guidelines1/ [Google Scholar]
[17]. Shaghaghian S, Pardis S, Mansoori Z, Knowledge, attitude and practice of dentists towards prophylaxis after exposure to blood and body fluidsInt J Occup Environ Med 2014 5:146-54. [Google Scholar]
[18]. Yao WX, Wu YL, Yang B, Zhang LY, Yao C, Huang CH, Occupational safety training and education for needlestick injuries among nursing students in China: intervention studyNurse Educ Today 2013 33:834-37. [Google Scholar]