Trauma scoring systems are routinely used to evaluate and monitor traumatic injury outcomes. It is done in order to reduce number of preventable deaths [1]. Presently, illness severity scoring systems are important tools for studying patient outcomes and to measure the efficacy of trauma centres. Initially efforts were focused on assessing rates of preventable mortality. But with increasing incidence of trauma, many statistical models have been developed in an attempt to accurately predict outcomes for trauma patients [2]. Each scoring system has its own strengths and weaknesses. The choice depends on the system’s ease of use and its applicability for that particular intensive care unit (ICU) or patient group [3].
The origin of TRISS (Trauma and Injury Severity Score) can be traced to the MTOS (Major Trauma Outcome Study), which was conducted in the United States in 1980s, and provides a data- base for audit in the individual patient and allows for comparison of performance over time and between hospitals [4].
Knaus et al., introduced the “Acute Physiology and Chronic Health Evaluation” (APACHE) system in 1981 to classify disease severity and predict future events in the course of disease [5]. In 1985 data from 5815 medical and surgical ICU admissions at 13 hospitals was used to refine APACHE I into APACHE II. The APACHE II score constituted of 12 routine physiologic measurements plus the patient’s age and previous health status [6]. APACHE II scoring is based on the changes of normal function of major organ systems. It is relatively independent of therapeutic interventions prior to ICU admission and specific disease processes [7]. With the use of more recent cohorts new scoring systems have been developed but still APACHE II is used for research and clinical audit purposes. It is easier to use in comparison to APACHE III and so has been in use for a longer time which allows consistency [3].
Our objective was to evaluate the ability of commonly used trauma scores (TRISS) along with a more general ICU scoring system (APACHE II), to accurately predict mortality in critically injured orthopaedic polytrauma patients requiring extensive care in an ICU.
Materials and Methods
It is a retrospective study conducted at a tertiary care teaching hospital situated in a hilly terrain of Uttarakhand, India. After the approval of research committee of the institution, medical records of orthopaedic patients being admitted to ICU from emergency in between January 2012 to April 2015 were accessed for the required information.
Data Collection
The medical records of 535 polytrauma patients who needed ICU care from January 2012 to April 2015 were retrieved. After applying inclusion and exclusion criteria 440 patients were excluded and only 95 patients were included in the study.
The inclusion criteria were patients with blunt injuries (Road traffic accident), age more than 15 years, brought within 48 hours of trauma, ISS>15 and any one long bone or pelvis or spine fracture. On the other hand, patients with penetrating trauma, burn injury, died within 48 hours of ICU admission, missing data and one who left the hospital against medical advice were excluded.
Medical records were carefully reviewed for the following parameters to calculate APACHE score: demo- graphic and clinical data, systolic, diastolic and mean arterial blood pressure (mm Hg), heart rate, respiratory rate, body temperature, initial Glasgow Coma Scale (GCS) score, arterial blood gas analysis (pH, PaO2, PaCO2, oxygen saturation, and base excess), FiO2, laboratory data (white blood cell count, haematocrit, and serum levels of sodium, potassium, creatinine), presence of chronic diseases or immune-compromised state. Severe chronic illness included liver cirrhosis with portal hypertension, New York Heart Association class IV congestive heart failure, chronic respiratory disease, end-stage renal disease receiving dialysis, and an immune-compromised state (example: leukaemia, lymphoma, or AIDS).
Calculation Method
Step1 - Abbreviated Injury Scores (AIS) [8] is calculated for different body regions scoring 1-6 for individual injuries. These body regions were the head or neck, face, chest, abdomen or pelvic contents, extremities or pelvic girdle, and external.
Step2- The ISS (Injury Severity Score) [9] was calculated using the AIS. To calculate an ISS, the highest AIS severity code in each of the three most severely injured ISS body regions was needed. ISS= (1st AIS score) ^2+ (2nd AIS score) ^2+ (3rd AIS score) ^2.
The ISS greater than 15 is defined as major trauma. The ISS was calculated using the Abbreviated Injury Scales 2005.
Step3- Calculate Revised Trauma Score (RTS) [10] (coefficients from the MTOS were used).
Formula for RTS is: RTS=βRR×RR+βSBP×SBP+βGCS×GCS;
where βRR, βSBP, and βGCS are the coefficients associated with RR (respiratory rate), SBP (systolic blood pressure), and GCS (Glasgow coma scale).
Step4-Calculate probability of survival using TRISS [4] Ps=1/ (1+e^-b)
Where Ps is an estimate of a patient’s survival probability
b = b0 + b1 (RTS) + b2 (ISS) + b3 (AGE INDEX) and
The b0, b1, b2, b3 are regression coefficients derived from the MTOS in 1995 which are different for penetrating and blunt injuries.
AGE INDEX = 0 for age less than 55 years&
AGE INDEX = 1 for age greater than or equal to 55.
The popular TRISS method calculates the probability of survival (Ps) of a trauma patient. “TRISS fallouts”, or unexpected non-survivors are patients who meet death despite the probability of survival on admission of >0.5. Preventable death can be divided into three categories: 1) definitively preventable death (DP): deaths occurred with Ps>0.50, 2) possible preventable death (PP): deaths occurred with 0.25<Ps<0.50, 3) non-preventable death (NP): deaths occurred with 0.25<Ps [1].
An extensive chart and computer check for data completeness, accuracy, and consistency was carried out with help of SPSS 22. Square root transformation was used for data which was not distributed uniformly. Unpaired t-tests were used to compare different scores in survivors and non survivors. The ROC curve was performed using the trial version of MEDCALC to check specificity and sensitivity of different scores.
Results
During these 40 months, 95 patients which met the criteria were studied and analysed. Total 82 (86.3%) patients were male while 13 (13.7%) were female. Out of 95 patients studied, 32(33.3%) patients were in the age group 15-25 years. Mean age of non survivors was 43.5 years & survivor was 38.1 years [Table/Fig-1].
Distribution of patients according to age
| Age Groups | End result | Total |
|---|
| non survivor | survivor |
|---|
| 15-25 | 11 | 21 | 32 |
| 25-35 | 7 | 7 | 14 |
| 35-45 | 4 | 9 | 13 |
| 45-55 | 6 | 9 | 15 |
| 55-65 | 5 | 6 | 11 |
| 65-75 | 4 | 1 | 5 |
| 75-85 | 2 | 0 | 2 |
| 85-95 | 1 | 2 | 3 |
| Total | 40 | 55 | 95 |
Mean APACHE II score on the day of admission [Table/Fig-2] in non survivors predicted a mortality rate of 40 % while mean APACHE II score on the day 1 after admission in non survivors predicted a mortality rate of 55%.
Mean values of scores in survivors and non survivors with p-values
| Score | Survivors | Non Survivors | p-value |
|---|
| TRISS* | 82±5.37 | 50.77±28.86 | <0.001 |
| APACHE II score on admission | 18.53±6.787 | 23.90±6.823 | <0.001 |
| APACHE II score on Day 1 | 14.38±6.816 | 27.70±8.579 | <0.001 |
| RTS | 6.49 ±1.38 | 5.33± 0.8 | <0.001 |
*Probability of survival
AUROC- Area under receiver operating characteristic curve
According to ROC curve analysis, APACHEII score on day 1 of admission (88.5%, 95% Cl= 80.3 to 94.2) proved to be more reliable system than TRISS methodology (83.1%, 95% CI=74 to 90) though the difference was not statistically significant (p>0.001). Specificity, sensitivity and AUROC for different scores are as mentioned in [Table/Fig-3,4].
Different parameters of various scores
| Score | Sensitivity | Specificity | AUROC | Youden Index |
|---|
| RTS | 89.09 | 57.50 | 0.763 | 0.4659 |
| TRISS | 83.64 | 77.50 | 0.831 | 0.6114 |
| APACHE II on Admission | 63.64 | 70.00 | 0.706 | 0.3364 |
| APACHE II on Day 1 | 90.91 | 72.50 | 0.885 | 0.6341 |
ROC curve comparing the sensitivity and specificity of TRISS, APACHE II on Admission, APACHE II on Day 1 and RTS
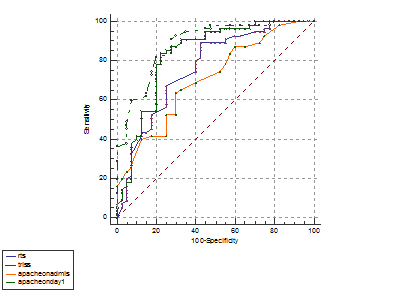
APACHE II on day 1 shows highest area under ROC Curve
Youden Index J was calculated to prove superiority of one scoring system over other. It was highest for APACHE II on Day 1 after admission followed by TRISS as shown in [Table/Fig-3].
The average time for the patient to reach the hospital was 7.5 hours for the survivors and 6.5 hours for non-survivors. Data was not uniformly distributed, so square root transformation was used and statistical significance of variable between survival and non-survival was done. It was found that there is no statistical significance in time taken by survivors and non survivors to reach emergency.
We had 4 unexpected survivor, these patients had survival probability of less than 50%.TRISS fallouts i.e. unexpected non survivors were 16 (survival probability of >50%).
Discussion
Indices of injury severity are integral part of triage, to outcome evaluation and quality assurance. As their application is gaining importance, severity scales are being more closely analysed for their accuracy and validity [11]. Thus data stratification has become very important. A possible implication for the increased precision required in risk stratification is that there is not “one size fits all” score, and this concept may be particularly true for the trauma population [12].
Trauma care systems in India are in their initial stages of development and there is an almost complete lack of organized trauma care [13]. It is an established fact that the mortality in serious injuries is six times worse in a developing country such as India compared to a developed country [14]. Zafar et al., and few others stated that present injury severity instruments using coefficients developed in western world do not accurately correlate with observed survival rates in a developing country [15].
Patients are often transported to the nearest hospital from the accident scene even though these hospitals may not have the resources to treat the patient. In our study, the low mean RTS of the non-survivors, as compared to the survivors, shows that the former were physiologically more deranged. The reason for this can be the delay in transporting a patient to the hospital. EMS (Emergency Medical services) is limited on account of remote locations in hilly terrain, few specialised hospital and longer duration of transport to specialised care centre. This leads to further deranged physiology when first seen in the hospital as compared to the developed world where the EMS is highly responsive and provision of level I/II trauma centres is present.
Non survivors had higher mean ISS than survivors which mean the former had more severe injuries. Impact of the accident can be reduced by using seatbelts, helmets and airbags. These would prevent serious injuries from happening [16]. Though the injury severity score which is commonly used for audit of collected trauma cases may be subjected to considerable observer variation. The ISS does not account for multiple injuries to the same body region or fatal damage to internal organs. In fact, two severe injuries to the same body region may have lowered the calculated score than two moderate injuries to different body regions [1].
Pre-hospital care is virtually non-existent in remote areas of hilly terrain, and ‘golden hour’ concept in such circumstances is questionable as it’s evident in our study too. The mean of time taken to reach emergency by survivors is more than non survivors and it was not statistically significant. The mean time from injury to arrival in hospital of patients dying with major injuries was 6.5 hours; details of pre-hospital treatment, airway management, and resuscitation were not retrievable in this group. The delays in definite treatment had a considerable negative impact on the outcome in our setting. The time interval of non survivors was lesser than survivors because badly injured patients are shifted first to higher centres without proper primary care. It may also be due to improper triage carried out at field level.
In our study of critically injured patients requiring greater than 48 hours of ICU care, APACHE II score on day 1 after admission was found to be relatively better score than TRISS in predicting mortality. This difference undoubtedly lies in the greater incorporation of physiologic and biochemical data into APACHE II. The system of APACHE II on admission underestimated mortality in our study. This could be explained by differences in patient population, coefficients used in study and referral criteria between the western world and our centre especially in hilly regions. Also because the APACHE-II does not consider pre-ICU management, which can restore a patient’s altered physiology. This lowers the points assessed and thus under estimates a patient’s true risk when taken into account just on admission to ICU [6]. Though in a study carried out by Jorge et al., it was seen that APACHE II score is a good prognostic marker of trauma patients in Emergency Department as well as 24 hours after admission to the ICU [17].
REMS (Rapid Emergency Score) an attenuated version of APACHE II was used in trauma patients though originally derived from medicine people. It was found to have good predictive mortality [17]. Abbreviated versions of the APACHE II score have been found to have similar prognostic values for trauma patients but it’s insisted that better designed studies are needed to validate abbreviated APACHE II scores in the trauma population [18].
Effectiveness of APACHE II has been proved even in neurosurgical ICU patients to predict in hospital mortality [19]. In a study carried out by Zali et al., [20] GCS was compared to APACHE II for predicting mortality in neurosurgical ICU patients. They concluded that, the GCS score provides simple, rapid and effective assessment in head injury patients but for the prediction of mortality in patients with multiple trauma APACHE II is superior to GCS since it includes multiple physiologic systemic parameters in these patients.
A study analysed different scoring systems (ISS,NISS and APACHE II) along with prothrombin time as independent predictors of the early mortality in polytrauma patients. It was seen that APACHE II and prothrombin time had the highest prognostic quality in polytrauma patients who had poor outcomes [21].
TRISS score for probability of death also shows observer variation, which is less at the extremes of probabilities but potentially very large between p= 0.05 and p= 0-95. Comparisons between groups, hospitals, and countries must be treated with circumspection and great care and attention paid to collection of injury severity score data to reduce observer variation [22]. TRISS allows for a reasonably effective mechanism by which anatomy, physiology, age and mechanism of injury can be taken into account as to their influence on outcome when some other independent variable is being studied [11]. Cayten et al., identified some limitations of TRISS methodology. They revealed: i) the inability of TRISS to account for multiple severe injuries to a single body part; ii) The inability to predict survival in low falls; iii) The lack of distinction between gunshot and knife injuries and the inability to take into account pre-existing conditions and underestimation of the effects of age and head injuries [23]. Since then, physicians have attempted to improve TRISS, and revised the coefficients as well as introduced new or modified variables in 1995 and 2010.
Challenges found during study were: i) Data Analysis: It is particularly difficult to measure the GCS in patients who are intubated or paralysed; ii) Missing data: It is difficult to get accurate and complete data of the early phases of care of the acutely injured individuals both in the pre-hospital and in hospital phases of care from medical records.
The ability to anticipate trauma complications based on these scoring systems could improve the survival rate in polytrauma patients [21].
Limitations of the Study
It was a retrospective study. Comparison and integration of data were not conducted with other trauma centres. A period 40 months of data collection may not be sufficient and small sample sizes can result in a lack of power. The accuracy of the predicted survival rate will be improved with cumulative patient data.
Conclusion
Our study demonstrates that general ICU scoring systems with a strong physiologic basis such as APACHE II are beneficial in orthopaedic polytrauma patients requiring greater than 48 hours of intensive care. It is a better predictor of clinical outcome than other trauma scores.
*Probability of survival