Psammomatoid Juvenile Ossifying Fibroma Involving Upper Jaw: A Rare Case Report
Ramlal Gantala1, Arjun Yadav Vemula2, Jithender Reddy Kubbi3, MS Muni Sekhar4, Dinesh Jhawar5
1Associate Professor, Department of Oral Medicine and Radiology, SVS Institute of Dental Sciences, Appanapalli, Mahabubnagar, Telangana, India.
2Post Graduate Student, Department of Oral Medicine and Radiology, SVS Institute of Dental Sciences, Appanapalli, Mahabubnagar, Telangana, India.
3Reader, Department of Oral Medicine and Radiology, SVS Institute of Dental Sciences, Appanapalli, Mahabubnagar, Telangana, India.
4Professor and HOD, Department of Oral and Maxillofacial Pathology, SVS Institute of Dental Sciences, Appanapalli, Mahabubnagar, Telangana, India.
5Associate Professor, Department of Oral and Maxillofacial Surgery, SVS Institute of Dental Sciences, Appanapalli, Mahabubnagar, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arjun Yadav Vemula, 1-1-652/C, Gandhi Nagar, Hyderabad – 500080, Telangana, India.
E-mail: arjunvemula2@gmail.com
Juvenile ossifying fibroma (JOF) is a fibro-osseous neoplasm, rare in occurrence and usually seen in young children. JOF is locally aggressive spreads quickly and is defined as a variant of ossifying fibroma. There are two types of ossifying fibroma depending on histopathology and classified as Psammomatoid juvenile ossifying fibroma (PJOF), Trabecular juvenile ossifying fibroma (TJOF). Both the types affect skull bones with the trabecular type being more common in the jaws- maxillofacial region and the psammomatoid type being more common in the paranasal sinuses, ethmoid sinuses- craniofacial region. Complete excision is mandatory because JOF’s have an extremely high rate of recurrence. A rare case of PJOF involving right maxilla sparing paranasal sinuses in a 15-year-old male patient with clinical, radiographic and histopathological features is discussed.
Fibrous Dysplasia, Maxilla, Odontogenic tumour
Case Report
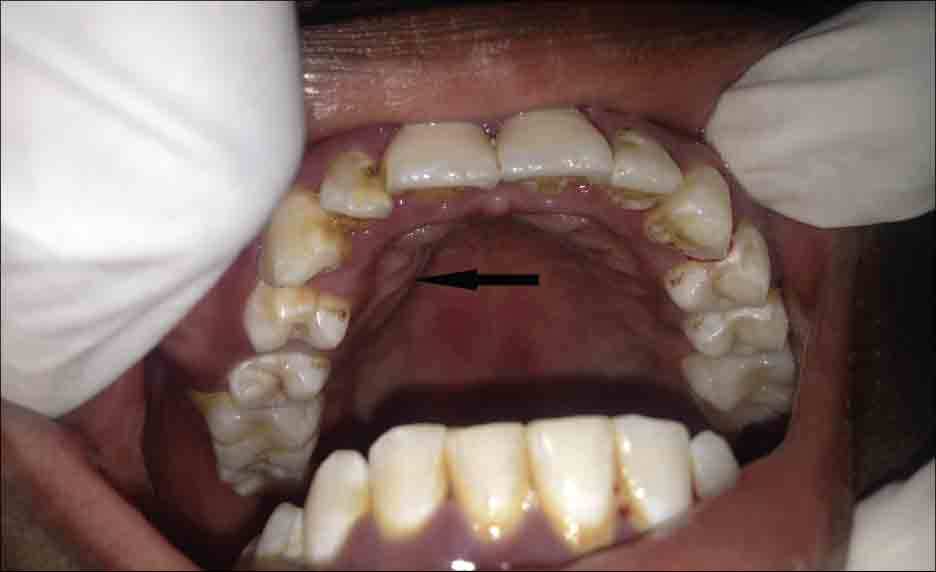
A 15-year-old male patient, presented to the Department of Oral Medicine and Radiology with a six months history of swelling on the right upper jaw showing mild asymmetry in mid face [Table/Fig-1]. The swelling was initially small which gradually increased to a size approximately 2.5 X 2 cm. Swelling was dome shaped with normal mucosal covering and it extended from distal of 13 to mesial of 16 anterioposteriorly and from upper buccal vestibule causing its obliteration, extending inferiorly to the level of attached gingiva superioinferiorly [Table/Fig-2] Swelling was well defined and asymptomatic pertaining to anaesthesia or paraesthesia of the upper lip, cheek or jaw. The swelling was bony hard in consistency with no signs of compressibility and fluctuation. No orbital or nasal deformity was observed. Palatally, the extension of the swelling covered by normal mucosa about 2 x 2 cm approximately, oval in shape seen extending from 11 to 15[Table/Fig-3]. Firm in consistency on palpation palatally with absence of tenderness and the teeth in affected area were vital when tested. Teeth in effected area were with grade I mobility (w.r.t) 13, 15 and grade III mobility (w.r.t) 14. No lymphadenopathy was detected and mouth opening was normal. Considering clinical presentation and age of the patient a provisional diagnosis of ‘Adenamatoid Odontogenic Tumor of right maxilla’ was given. Differential diagnosis of fibrous dysplasia and ossifying fibroma were considered.
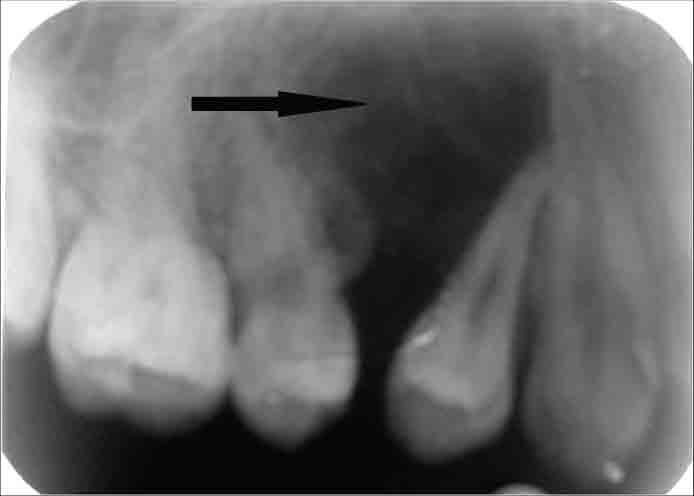
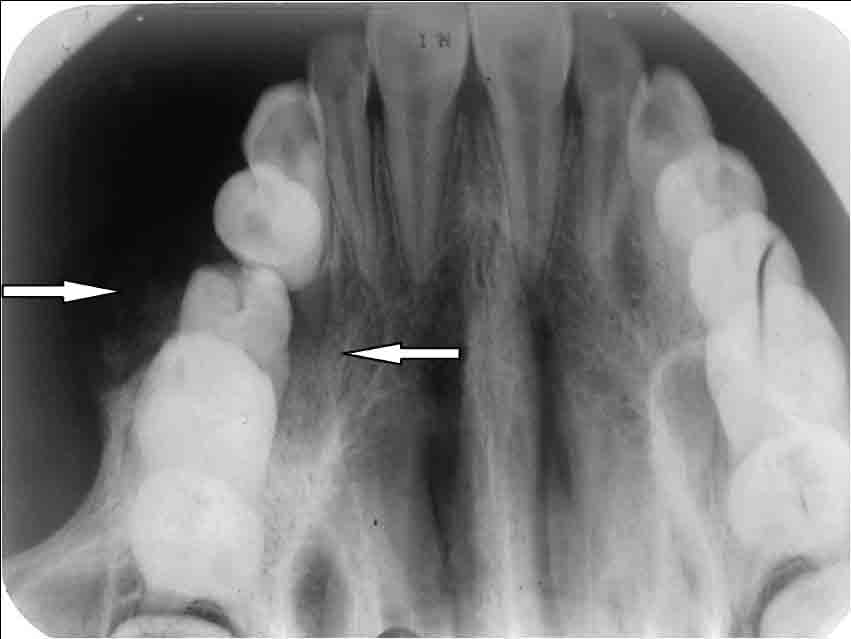
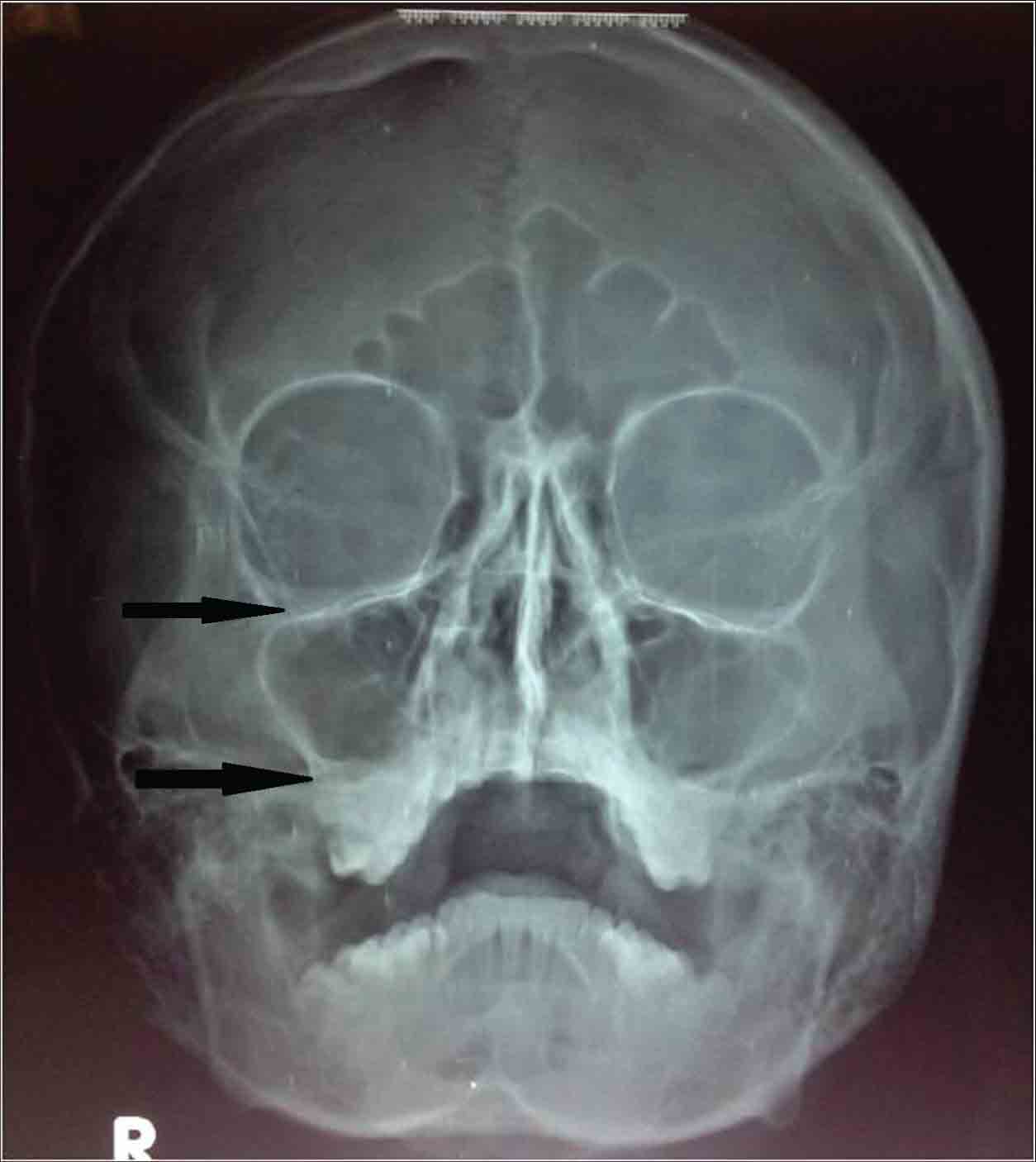
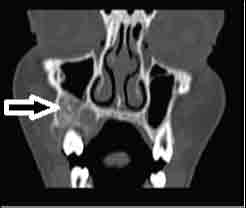
Intraoral periapical [Table/Fig-4] and occlusal [Table/Fig-5] radio-graphic examination revealed a lesion displaying mixed radiodensity in the 14, 15 region causing root divergence. Orthopantomogram examination revealed an image showing displacement of teeth 14 and 15 with no evidence of root resorption [Table/Fig-6]. The centre of the lesion appeared radiolucent with the margins relatively defined. The lesion extended from the bone crests of 14, 15 and fanning out laterally to approximately 1 cm above the apical level of adjacent teeth. Paranasal sinus (PNS) view of skull radiograph [Table/Fig-7] and Computed tomography (CT) of the facial bones demonstrated a relatively circumscribed lesion on the right maxilla with no involvement of nasal septum, maxillary sinus invasion and right orbital floor [Table/Fig-8-9]. Aspiration yielded air thereby a negative result, ruling out any cystic lesion. As the lesion was asymptomatic and locally fast growing, with no associated neurological symptoms, the diagnosis was concluded to be a benign neoplastic process. Keeping differential diagnosis of ossifying fibroma, cemento-ossifying fibroma and mixed odontogenic tumours as these mostly occur in younger patients and present as mixed density mass lesions in the tooth bearing portions of the jaws.
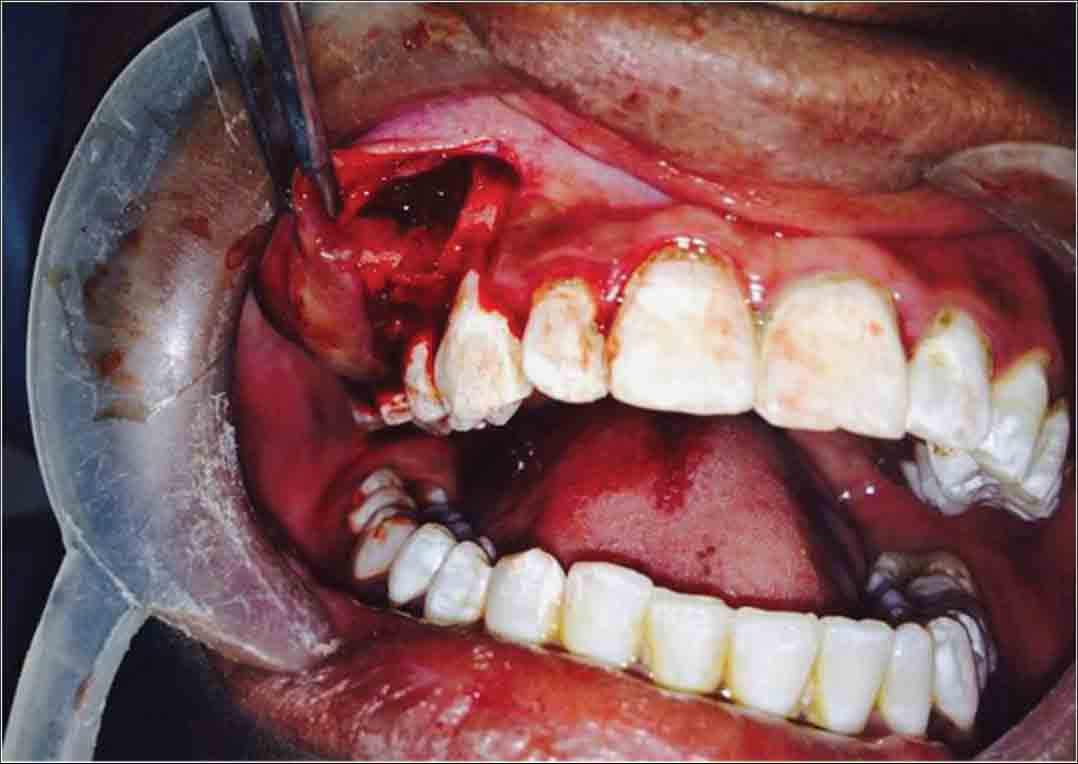
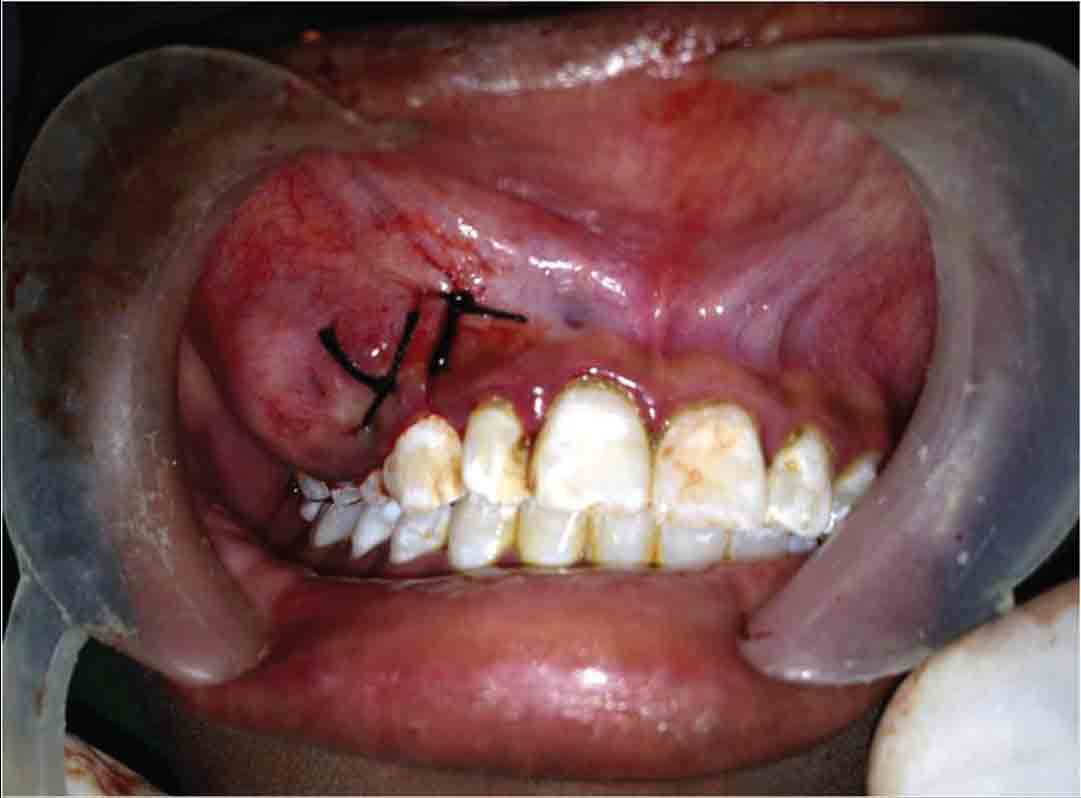
An incisional biopsy was performed under local anaesthesia and resultant tissue was sent for histopathologic evaluation [Table/Fig-10,11].
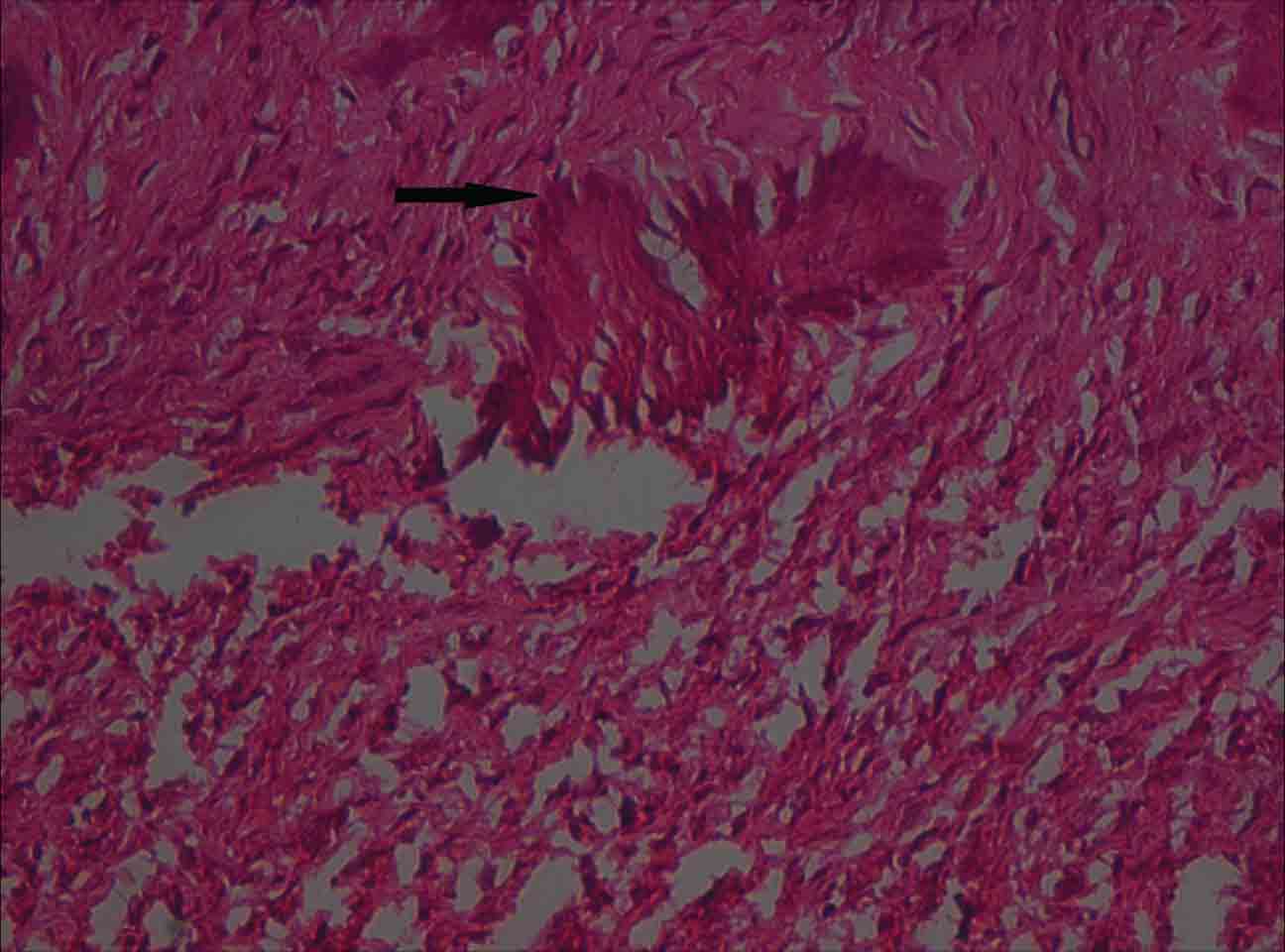
Histopathological examination revealed that the tumour sections show a highly cellular connective tissue stroma. The connective tissue exhibits numerous active plump fibroblasts showing little pleomorphism predominantly arranged in streaming fascicles while in few areas the connective tissue is hypocellular with dense collagen fibers. Within the tumour tissue are scattered psammoma like ossicles with peripheral brush border [Table/Fig-12,13].
Under general anaesthesia, the tumour was exposed and enucleation done [Table/Fig-14] in toto [Table/Fig-15]. Tooth 14 was found to be mobile, extracted along with the lesion [Table/Fig-16]. Bony margins were smoothened with a clear demarcation evident between tumour and healthy bone. Patient was on regular recall visits with a monthly interval and there were no signs of recurrence [Table/Fig-17]. Healing of surgical site with normal trabecular pattern can be appreciated [Table/Fig-18] and noticeable diminished periapical radiolucency seen in radiographs exposed during the eighth month recall visit [Table/Fig-19].
Discussion
A fibro osseous lesion is one in which bone is replaced by cellular fibrous tissue with amorphous mineralization. Juvenile Ossifying Fibroma (JOF) is an uncommon lesion that has been distinguished from the larger group of ossifying fibromas on the basis of age of the patients, most common site of involvement and clinical behaviour [1]. Johnson et al., reported that JOF occurs mostly in children and adolescents though infrequently seen in adult population. Psammomatoid Juvenile Ossifying Fibroma (PJOF) is reported more frequently in adults than Trabecular Juvenile Ossifying Fibroma (TJOF) showing wider age range from 3 months to 72 years but TJOF is seen more commonly in young patients ranging from 2 years to 33 years [2]. Malathi N et al., reported two cases of PJOF in adults as it can occur at any age such as in a 31-year-old female or a 46-year-old female [3]. The case report discussed here is PJOF in a 15-year-old male patient. Guruprasad R et al., discussed PJOF case in a 12-year-old female patient with recurrence after excision; presented with huge swelling involving right maxillary sinus, frontal sinus, ethmoidal sinus, inferior orbital ridge, right side of palate [4] showing that PJOF has a tendency towards paranasal sinuses and orbit accounting 75% of cases reported, the case discussed in this article showed lesion involving right maxilla with buccal palatal cortical expansion showing slight obliteration of right maxillary sinus without invasion which is quite rare accounting only 25% of the reported cases of PJOF involving gnathic areas of craniofacial region.
Radiographically JOF’s have characteristic pattern such as round, relative to well defined corticated margins with a cyst like appearance and in computed tomography (CT), when image is viewed in a bone window setting the lesions appear less dense than normal bone. A study conducted by Owosho et al., stated that “Juvenile Ossifying Fibroma has two histologic variants with distinct imaging characteristics that can help differentiate between these variants in order to provide an accurate diagnosis”. The study revealed CT of PJOF’s show ground glass radiopaque appearance of the lesion as an outer thick mantle with central radiolucent area, a solitary ground glass mural nodule or as a solid radiopacity and TJOF’s show primarily radiolucent area with irregular and scattered calcifications [5]. Contrary to this study our case showed unique characteristic of TJOF with background radiolucency exhibiting irregular and scattered calcifications while histopathology report confirmed the lesion as PJOF.
Microscopically PJOF’s presents as eosinophilic spherical structures scattered in fibrous stroma, Golg named these spherical structures as ‘psammoma- like bodies’. These particles vary in appearance such a concentric lamellated to irregular both having central basophilic area and a peripheral eosinophilic fringe. Ultra structure of psammoma- like bodies manifest with a dark rim of crystals. From these crystals spicules and needle-like crystalloids project toward the periphery resembling brush border [6] the latter form was seen in our case.
Management should ideally be done by block resection followed by bone grafting in large lesions because of its high recurrence rate 30%-58%. As JOF’s are treated like locally aggressive neoplasm, thorough curettage following enucleation is advised in small lesions if there is a clear demarcation between the lesion and normal bone.
Rai et al., reported two cases where they performed block resection [7] where as in our case we performed enucleation and curettage asthere was a clear demarcation between the tumour tissue and the surrounding normal bone.
Extra oral view of patient showing mild obliteration of right nasolabial fold

Intra oral view of buccal aspect with arrows showing anterior and inferior margins of the swelling

Intra oral view of palatal extension of the lesion shown with an arrow
Intraoral periapical radiograph showing mixed radiodensity marked with an arrow, 14, 15 teeth show root divergence
Occlusal radiograph marked with arrows showing buccal palatal extension of lesion with ossifications
Orthopantomograph showing relatively defined radiolucent lesion apical to 14, 15 marked with arrows

Paranasal Sinus view of skull radiograph marked with arrows show no involvement of right maxillary sinus, right orbit
CT coronal view marked with an arrow show borders of lesion, primarily radiolucent with irregular and scattered calcifications
CT axial view showing margins of lesion, arrows indicating a relatively circumscribed lesion on the right maxilla

Intraoral image showing incisional biopsy site
Intraoral image showing sutures placed at incision biopsy site
Photomicrograph (10X) H&E stained sections showing ossicles indicated with an arrow, resembling psammoma- like bodies
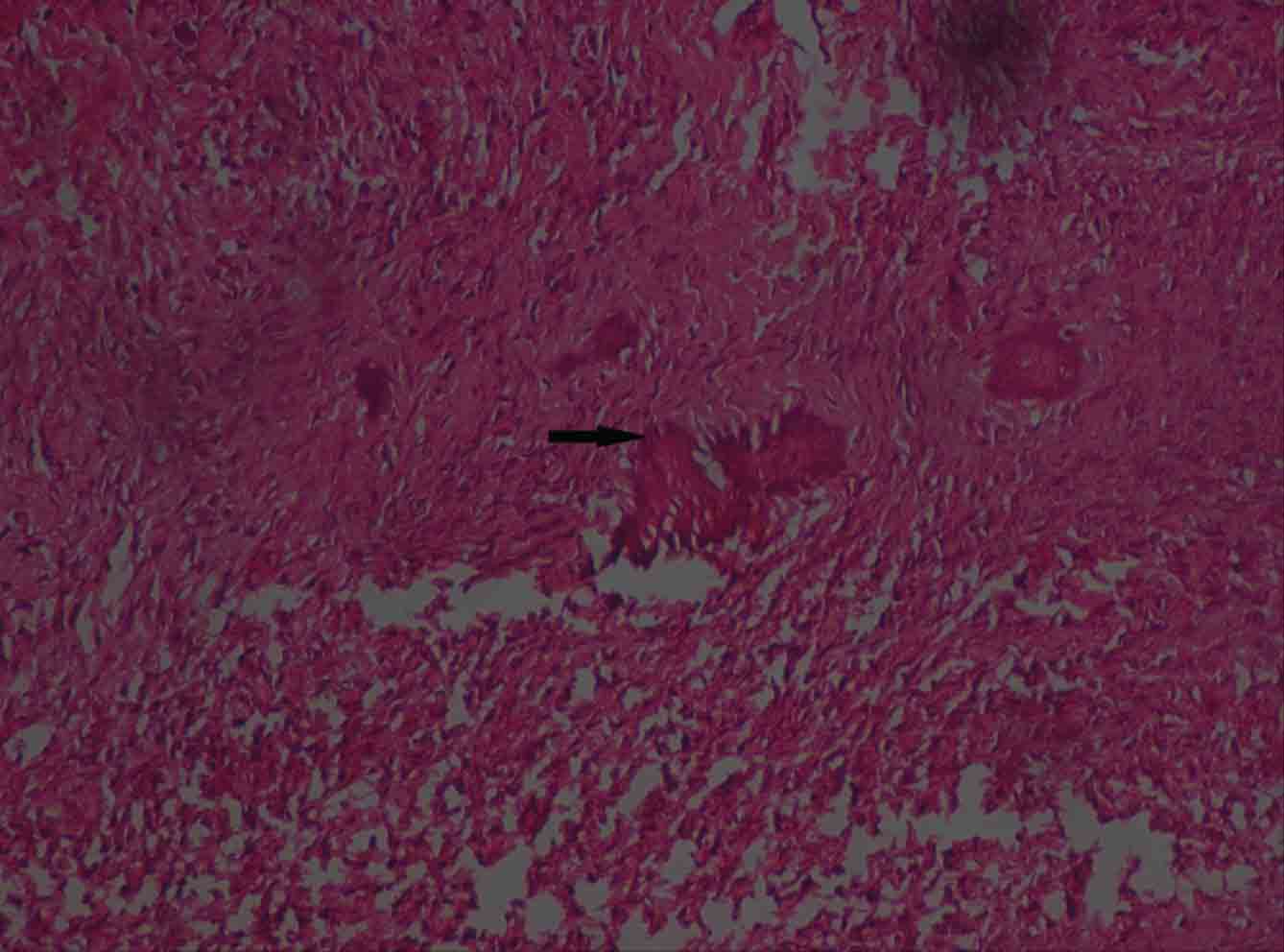
Magnified photomicrograph (40X) of psammoma- like bodies, indicated with an arrow showing peripheral brush border appearance
Intraoperative image showing surgical enucleation
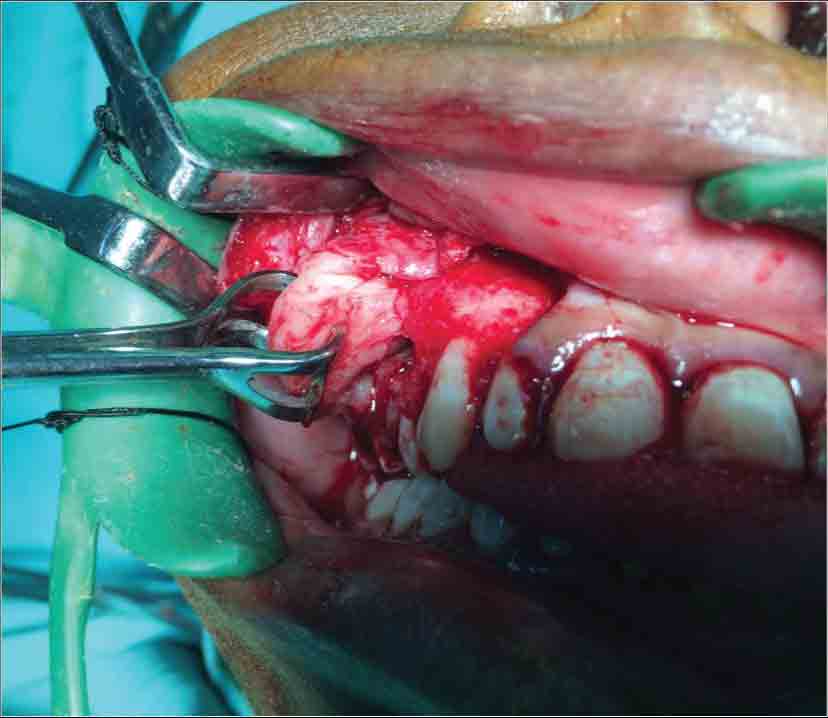
Image showing volume of gross specimen

Immediate postoperative intraoral image after excision of lesion and extraction of 14
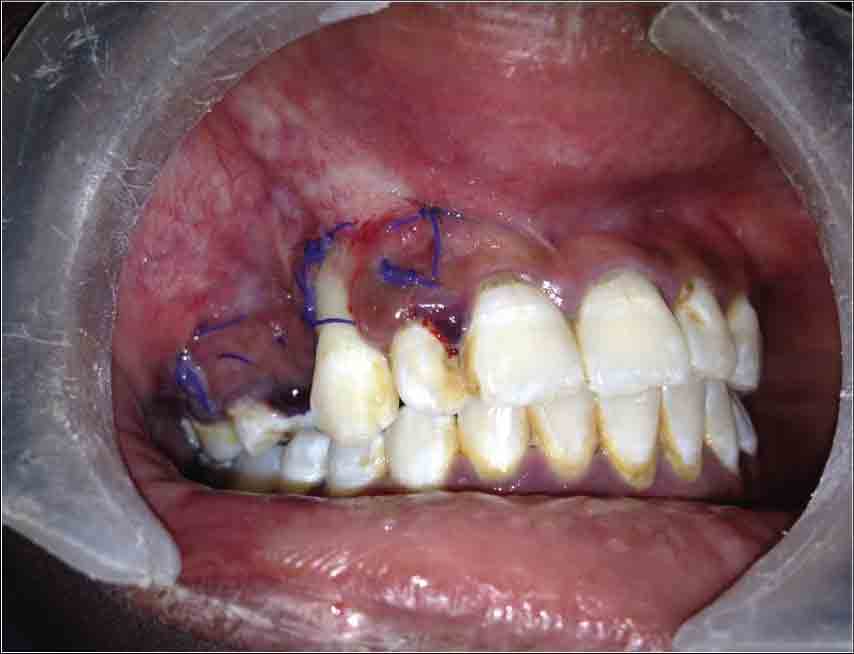
Eighth month postoperative intraoral image showing no signs of recurrence at enucleated site indicated with an arrow

Eighth month postoperative IOPA showing normal trabecular pattern indicated with an arrow at the site of excised lesion

Eighth month postoperative OPG showing diminished radiolucency apical to 13, 15 indicated with an arrow

Conclusion
Juvenile Ossifying Fibroma is a benign fibro-osseous lesion which show high recurrence rate and locally aggressive behaviour warranting early detection and proper surgical management along with long term follow up. Clinical, radiological and histological correlation before diagnosis is very important because PJOF’s and TJOF’s show variations which explains the demand for some more studies, case reports to compare differences between these two types.
[1]. MS Kamal, MAA Bahar, MA Latif, Juvenile ossifying fibroma of the maxilla:a case reportAKMMC J. 2013 4(1):42-44. [Google Scholar]
[2]. LC Johnson, M Yousefi, TN Vinh, Juvenile active ossifying fibroma: its nature, dynamics and originActa Otolaryngol Supple 1991 488:1-40. [Google Scholar]
[3]. N Malathi, T Radhika, H Thamizhchelvan, C Ravindran, S Ramkumar, G Giri, Psammomatoid juvenile ossifying fibroma of the jawsJ Oral Maxillofac Pathol 2011 15(3):326-29. [Google Scholar]
[4]. R Guruprasad, SD Gupta, N Dua, R Mehta, Juvenile psammomatoid ossifying fibroma – a case reportPeople’s Journal of Scientific Research 2011 4(1):31-34. [Google Scholar]
[5]. AA Owosho, MA Hughes, JL Prasad, A Potluri, Branstetter B. Psammomatoid and trabecular juvenile ossifying fibroma: two distinct radiologic entitiesOral Surg Oral Med Oral Pathol Oral Radiol 2014 118:732-38. [Google Scholar]
[6]. A Badri, S Shirafkan, M Razavi, SA Moghadam, A novel treatment of aggressive psammomatoid juvenile ossifying fibroma: a case reportJentashapir J Health Res 2014 5(4):e21888. [Google Scholar]
[7]. R Shalu, K Mandeep, G Sumit, M Prabhat, Trabeculae type of juvenile aggressive ossifying fibroma of the maxilla: report of two casesContemp Clin Dent 2012 3:S45-50. [Google Scholar]