Introduction
Several congenital malformations affect developing fetuses, among which Neural tube defect (NTD) is most common. Folic acid supplementation brought decline in the incidence of NTDs. The present study aims at finding the incidence of NTDs in a tertiary care hospital and compares the results with the similar Indian studies published earlier.
Materials and Methods
The study was done at Chettinad Hospital & Research Institute (CHRI), Kelambakkam. The total number of deliveries was recorded for a period of five years from 2009 to 2013. Fetuses which were still born with neural defect were collected and observed in detail externally for the sex, type of NTD and other associated anomalies. Indian studies published between 1987 and 2014 reporting the incidence of NTDs among the births occurred were retrieved from the Internet and their various observations were used for comparison.
Results
The number of deliveries conducted between 2009 and 2013 at CHRI was 3220. Of these, babies born with NTDs were nine (5 males and 4 females). The incidence of fetuses with meroanencephaly, holoanencephaly, craniorachischisis, encephalocele and myelocele were 0.62, 0.62, 0.93, 0.31 and 0.31 per 1000 births respectively. Overall incidence of NTDs in the present study was 2.79/1000 births. Fetuses with NTDs also had the following anomalies – Club foot, cleft lip and palate and exomphalos.
Conclusion
Comparing the results with the previous studies it is clearly evident that the incidence of NTDs have significantly reduced from 11.42/1000 births to 2.79/1000 births. In most of the previous studies NTDs had a female preponderance whereas present study has a male preponderance.In older studies, spina bifida was the most common NTDs followed by anencephaly. But in the present study anencephaly was the common NTD than spina bifida. Incidence of NTDs has reduced due to various reasons like prenatal screening for fetal anomalies and folic acid supplementation.
Introduction
Neural tube defects (NTD) are anomalies of neurulation during fetal development. The NTDs are broadly classified into cranial and spinal defects. The cranial defects are further classified into encephalocele, anencephaly and inencephaly. The anencephaly is further subdivided into meroanencephaly and holoanencephaly. The spinal defects are classified into open and closed neural defects. Open variety includes myelocele and meningomyelocele. Closed variety includes meningocele and spina bifida occulta [1].
NTDs are the most common malformations having an incidence of 1-5 per 1000 live births [2]. The two most common neural tube defects are spina bifida and anencephaly [3]. In spina bifida, the fetal spinal column does not close completely. In anencephaly, there is absence of parts of brain and the overlying skull.
NTDs are usually diagnosed before the infant is born, through lab or imaging tests. Among the NTDs, anencephaly is not compatible with life and the fetuses are still born or die few hours after birth. While depending on the severity, the child with spina bifida can survive with permanent disability. The exact causes of neural tube defects are not known. Low intake of folic acid before getting pregnant and in early pregnancy increases the risk of having a fetus affected by NTDs, including anencephaly. When United States started folic acid supplementation and fortification of food grains with folic acid the incidence of pregnancies with NTD (spina bifida and anencephaly) declined by 27% [4]. The present study aims at finding the incidence of NTDs in a tertiary care hospital and compares the results with the similar Indian studies published earlier.
Materials and Methods
The study was done at Chettinad Hospital & Research Institute (CHRI), Kelambakkam, which is a tertiary care teaching hospital. The total number of deliveries was recorded for a period of five years from 2009 to 2013. During this period, the fetuses which were still born with neural defect were collected after getting the consent of the parents. Fetuses died or terminated due to other causes were excluded from the study. They were stored in 10% formalin solution. The fetuses were observed in detail externally for the sex, type of NTD and other associated anomalies and the findings were documented. The approximate crown rump length (CRL) was measured and the probable gestational age of the fetuses were calculated. The fetuses were not dissected to find other internal anomalies.
Indian studies published between 1987 and 2014 reporting the incidence of NTDs among the births occurred in tertiary care hospitals and rural areas were retrieved from the Internet and their various observations like number of deliveries, number and types of NTDs observed and male/female ratio were used for comparison. Studies reporting NTDs from prenatal diagnosis were not included for comparison.
Results
The number of deliveries conducted between 2009 and 2013 at CHRI is given in [Table/Fig-1]. The total number of deliveries conducted during this period was 3220. Of these deliveries, the number of babies born with NTDs was nine (5 males and 4 females) and the details are given in [Table/Fig-2]. The incidence of NTDs in the present study is nine out of 3220 deliveries. The gestational age of the fetuses ranges from 11 weeks to 19 weeks.
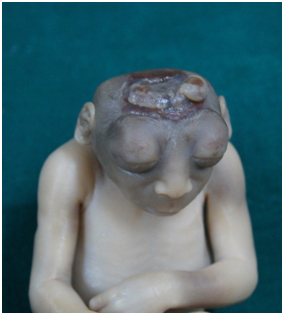
The types of NTD observed in the present study with their incidences are given in [Table/Fig-3].The anencephalic fetuses were of meroanencephalic [Table/Fig-4] and holoanencephalic [Table/Fig-5] types with equal incidences (0.62/1000 birth each).There was one fetus with rachischisis along with anencephaly [Table/Fig-6]. The fetus with myelocele had the defect at the lumbar region [Table/Fig-7]. There were four fetuses with other anomalies along with NTDs. There were two fetuses with club foot deformity [Table/Fig-6,7], one fetus with cleft lip and palate [Table/Fig-5] and one fetus with exomphalos [Table/Fig-8] along with NTD.
In the present study, Anencephaly is the common type of NTD (44.4%) followed by Craniorachischisis (33.3%). The defects like occipital encephalocele [Table/Fig-9] and myelocele [Table/Fig-7] were less common (11.1%).
[Table/Fig-10] shows the data about the NTDs from various Indian studies conducted during different time periods and from different parts of the country.
Discussion
Neurulation is the process by which neural tube is formed during stage 10 of embryogenesis that takes place around 22-23 days [5]. In mammals, neurulation occurs in two phases: primary and secondary neurulation. Primary neurulation occurring at 3rd and 4th week of development forms the entire neural tube cranial to the caudal neuropore. Secondary neurulation occurrs at tail bud region [6]. Earlier it was proposed that the fusion of neural tube starts from a single initiation site and progresses both cranially and caudally towards the cranial and caudal neuropores. Later multiple sites of neural tube fusion were proposed and extensive studies were made in rats and mice. According to Sakai [7] in mice there are four sites at which fusion of neural tube takes place. Site 1 appears in the cervical region at the caudal part of hindbrain and proceeds bidirectionally. Site 2 appears at the junction of prosencephalon and mesencephalon and proceeds bidirectionally. Site 3 appears at the cranial end of neural plate and proceeds caudally. Site 4 appears at the caudal end of neural plate and proceeds cranially.
Van Allen et al., [8] proposed multisite closure model of neural tube with five sites of closures in humans based on the observation of types and occurrence of NTDs. Of the five sites 3 are present in the cranial region and 2 are present in the spinal region. According to this model the various types of NTDs observed in this study can be explained due to failure of closure at these different sites. Meroanencephaly occurs due to error in closure at site 2, holoanencephaly due to error at sites 2 and 4, craniorachischisis due to error at sites 2, 4 and 1 and spina bifida cystic or myelocele due to error at site1.
Anencephaly occurs in 3 phases: First the cranial part of the neural tube fails to close, second the developed brain parts protrude and are exposed to the amniotic fluid and at last degeneration of the exposed part results in anencephaly [2].
Occipital encephalocele occurs when the surface ectoderm does not separate from the developing neural tube at the occipital region. This leads to defects in the formation of occipital bone. Encephalocele is associated with the following syndromes: Meckel – Gruber syndrome, Walker – Warburg syndrome, Dandy – Walker syndrome, Joubert syndrome, Trisomy 13 and Amnion rupture sequence [2].
NTD is a multifactorial disorder occurs due to the influence of both genetic and environmental factors. If more than one close relative is affected then the risk of NTD for future siblings is higher. Monogenic inheritance of NTD shows that the disease may be produced by single genes, particularly genes present in the X gene. Anencephaly is more common among females and lumbosacral spina bifida is more common in males. Environmental factors such as socio-economic status, nutritional deficiency, hypothermia, gestational diabetes, use of anticonvulsant drugs and insulin are well known risk factors [5].
Deficiency of vitamins B12, B6 and folate cause hyperhomo-cysteinaemia, which is implicated in the occurrence of NTDs in Indian babies [9].
Every year 3-4 lacs babies are born with NTDs. In United States the incidence of NTDs is 1/1000 live births [3] and it is higher in white population than black and female are more affected than males [10].The incidence of NTDs reported in India ranges from 0.5 to 11 per 1000 live births [11]. The northern states like Punjab, Haryana, Rajasthan and Bihar had higher prevalence when compared to the southern states [12]. In 1973 the incidence of NTDs in Madras and Pondicherry were 2.3/ 1000 births and 1.9/ 1000 births which was far less than the northern states of India like Amritsar, Chandigarh, Jaipur, Ajmer, Udaipur and Delhi [12].
[Table/Fig-10] shows the comparison between the present study and the data of NTDs from similar Indian studies. All these studies were done at urban setting in tertiary care teaching hospitals except the study by Anil et al., which was done in a rural setting of Balrampur in Uttar Pradesh [9]. Studies done by Kulkarni et al., [13] Kulkarni et al., [14], Sharada [17] and Suresh & Dhananjay [18] were from different places of Karnataka. Whereas studies done by Shanta Kumari et al., [19], Mahadevan & Vishnu Bhat [16] and Mini et al., [15] were from Odisha, Pondicherry and Delhi respectively. Of these, study done by Mahadevan & Vishnu Bhat [16] is the longest and reports 310 cases of NTDs.
It is clearly evident from the [Table/Fig-10] that the incidence of NTDs have significantly reduced from 11.42/1000 births to 2.79/1000 births. In the present study the incidence of NTDs is 2.79 per 1000 births. This is in accordance with the rates as found by Creasy and Alberman [20], which is 2.8 per 1000 births.
The present study has few observations which were different from the previous studies. In most of the previous studies NTDs had a female preponderance whereas present study has a male preponderance (55.5%) [Table/Fig-3].
In older studies, spina bifida was the most common NTDs followed by anencephaly. But in the present study anencephaly was the common NTD (44.4%) than spina bifida (11.1%) [Table/Fig-3]. This observation was similar to the observations of Kulkarni et al., [13], Kulkarni et al., [14] and Mini et al., [15].
Iniencephaly, a rare defect with an incidence of 0.1 in 10,000 live births to 1 in 65,000 live births [1] were reported in three earlier studies [Table/Fig-10]. But it was not observed in the present study.
In all the above studies the occurrence of encephalocele among NTDs was constant ranging between 8% and 11% except the study by Mini, Neera, Shashi & Bhargava [15] reporting occurrence to be 1.5%. All these data show that there is a decline in the occurrence of NTDs which is in accordance with worldwide decline in occurrence of NTDs. Factors which had led to the decline in the incidence of NTDs are genetic counseling, proper prenatal diagnosis and nutritional supplementation with folate [21]. Though NTDs are multifactorial in origin, prenatal and perinatal folic acid supplementation has reduced the risk of NTDs in women with or without a history of NTD affected pregnancies [1].
Medical Research Council vitamin study research group in a study done between 1983 and 1991 revealed preconceptional daily use of 4mg folic acid reduced by 70% recurrence of NTDs among women having previous pregnancy affected with NTDs in UK and other countries [22]. In a study done in China between 1993 and 1996 showed 40% and 80% reduction in risk of NTDs in areas having low and high frequency of NTDs respectively, among women who consumed 400 microgram of folic acid periconceptionally [23]. Similarly a study done in Nuevo Leon in Mexico showed the overall incidence of NTDs declined by 43% from 1.04/1000 live births in 1999 to 0.58/1000 live births in 2001 following the use of folic acid preconceptionally [24]. In 1998, United States made fortification of every 100grams of cereal products with 140 micrograms of folic acid mandatory. After mandatory fortification of cereals with folic acid, the prevalence of NTDs reduced by 28% immediately and thereafter remained stable between 1991 and 2011. It is estimated that folic acid fortification averts occurrence of NTDs in 1300 live births annually [25].
In India there are no randomized control trials on effect of folic acid on NTDs. Still Indian women are advised to take folic acid periconceptionally. There are no national programs advocating folic acid fortification of food products for prevention of NTDs, available in India [11]. The current recommendation to reduce the chances of NTDs is daily supplementation of 0.4 mg of folic acid prior to pregnancy and during pregnancy. 4-5 mg per day should be taken by women who have a high risk of NTDs [1]. Still 0.7 – 0.8 per 1000 pregnancies are affected by some form of NTD even after folic acid supplementation [26]. So, folic acid supplementation alone is not enough to eradicate NTDs.
Number of deliveries conducted at CHRI between 2009 and 2013
| Year | Number of deliveries |
|---|
| 2009 | 574 |
| 2010 | 622 |
| 2011 | 628 |
| 2012 | 666 |
| 2013 | 730 |
| Total | 3220 |
Sex, Gestational age, NTD and Associated malformations observed in fetuses
| S.No | Sex | CRL (cm) | Gestational Age (weeks) | Cranial defect | Spinal defect | Associated malformations |
|---|
| 1 | Female | 20 | 19 | Anencephaly (Meroanencephaly) | | |
| 2 | Male | 17 | 18 | Anencephaly (Meroanencephaly) | | |
| 3 | Female | 19 | 19 | Anencephaly (Holoanencephaly) | | Cleft lip and palate |
| 4 | Female | 18 | 18 | Anencephaly (Holoanencephaly) | Rachischisis | Club foot deformity |
| 5 | Female | 14 | 17 | Craniorachischisis | |
| 6 | Male | 11 | 15 | Craniorachischisis | |
| 7 | Male | 5 | 11 | Craniorachischisis | Exomphalos |
| 8 | Male | 15 | 17 | Occipital Encephalocoele | | |
| 9 | Male | 11 | 15 | | Myelocele | Club foot deformity |
Types, Number, Incidence of NTD and sex of the fetuses observed in the present study
| NTD | Number of fetuses (%) | Incidence /1000 births | Male | Female |
|---|
| Anencephaly | | | | |
| i. Meroanencephaly | 2 (22.2) | 0.62 | 1 | 1 |
| ii. Holoanencephaly | 2 (22.2) | 0.62 | | 2 |
| Craniorachischisis | 3 (33.3) | 0.93 | 2 | 1 |
| Encephalocoele | 1 (11.1) | 0.31 | 1 | |
| Myelocele | 1 (11.1) | 0.31 | 1 | |
| Total | 9 (100) | 2.79 | 5 | 4 |
Meroanencephaly in an 18-week-old male fetus
Holoanencephaly in a 19-week-old female fetus with cleft lip and palate

Holoanencephaly and rachischisis in an 18-week-old female fetus with club foot

Lumbar myelocele in a 15-week-old male fetus with club foot

Craniorachischisis in an 11-week-old male fetus with examphalos

Occipital encephalocele in a 17-week-old male fetus

Indian studies on NTDs from 1985 to 2013
| S.No. | Authors | Study area | Study period | No. of deliveries | No.of cases with NTD s | Incidence (/1000 births) | Male | Female | Anencephaly | Encephalocele | Spina bifida | Iniencephaly |
|---|
| 1 | Kulkarni et al., [13] | Urban | Mar-Aug 1984 | 5500 | 62 | 11.3 | * | * | 31 | 5 | 24 | 2 |
| 2 | Kulkarni et al., [14] | Urban | 1985-1987 | 3500 | 40 | 11.42 | 17 | 23 | 19 | 4 | 15 | 2 |
| 3 | Mini et al.,[15] | Urban | Jan 1988-Aug 1990 | 9220 | 65 | 7 | 19 | 46 | 36 | 1 | 24 | - |
| 4 | Anil et al., [9] | Rural | 2002-2003 | 1218 | 10 | 8.2 | 4 | 6 | 3 | 1 | 6 | - |
| 5 | Mahadevan & Vishnu Bhat [16] | Urban | 1998-2004 | 54738 | 310 | 5.7 | 120 | 190 | 98 | 36 | 170 | - |
| 6 | Sharada [17] | Urban | May-Sep 1999 | 3000 | 32 | 10.66 | 20 | 10 | 12 | - | 16 | - |
| 7 | Suresh & Dhananjay [18] | Urban | 2004-2009 | 4125 | 13 | 3.15 | 7 | 6 | 4 | - | 4 | - |
| 8 | ShantaKumari et al., [19] | Urban | 2008-2013 | * | 167 | 4.47 | * | * | 53 | 19 | 76 | 9 |
| 9 | Present study | Urban | 2009-2013 | 3220 | 9 | 2.79 | 5 | 4 | 4 | 1 | 1 | - |
* – Not Available
Limitation of the study
The limitation of this present study is that having been conducted in tertiary care teaching hospital, it doesn’t represent the true incidence of NTDs at the community level. Detailed demographic study of the mothers’, who have given birth to fetuses with NTDs analysed in this study, has not been attempted. Being a retrospective study the folic acid status of women and the data regarding whether they took prenatal or perinatal folic acid supplementation could not be presented.
Conclusion
The present study shows there is a decline in the incidence of NTDs when compared to the older studies due to various reasons like prenatal screening of fetal developmental anomalies and folic acid supplementation before and during pregnancy. It also points out that NTDs were more common in males and anencephaly is more common than spina bifida in contrast to the earlier studies.
* – Not Available
[1]. AL Jorge, Neural Tube Defects. Singapore: World scientific publishing Co Pvt. Ltd 2011 [Google Scholar]
[2]. JTD Hans, L Martin, H Akira, Clinical Neuroembryology: Development and Developmental Disorders of the Human Central Nervous System 2014 2nd EditionHeidelbergSpringer [Google Scholar]
[3]. JD Cragan, HE Roberts, LD Edmonds, Surveillance for anencephaly and spina bifida and impact of prenatal diagnosis in United States. 1985-1994Mortal Morb Wkly Rep 1995;44 44:113 [Google Scholar]
[4]. Spina Bifida and Anencephaly Before and After Folic Acid Mandate --- United States, 1995-1996 and 1999-2000Mortal Morb Wkly Rep 2004 53(17):362-5. [Google Scholar]
[5]. KL Moore, TVN Persaud, The Developing Human 2008 8th EditionSaundersElsevier:43-48. [Google Scholar]
[6]. RD Eric, MG Timothy, CE Heather, RG John, V Michel, CS Marcy, Human Neural Tube Defects: Developmental Biology, Epidemiology, and GeneticsNeurotoxicol Teratol 2005 27(3):515-24. [Google Scholar]
[7]. Y Sakai, Neurulation in the mouse: manner and timing of neural tube closureAnat Rec 1989 223:194-203. [Google Scholar]
[8]. MI Van Allen, DK Kalousek, GF Chernoff, D Juriloff, M Harris, BC Mc Gillivray , Evidence for multi-site closure of the neural tube in humansAm J Med Genet 1993 47:723-43. [Google Scholar]
[9]. C Anil, S Siju, K B Robyn, CA A´sok, Incidence of neural tube defects in the leastdeveloped area of India: a population-based studyLancet 2005 366:930-31. [Google Scholar]
[10]. JM Larry, LD Edmonds, Prevalence of spina bifida at birth United States 1983- 1990. A comparison of two surveillance systemsMortal Morb Wkly Rep 1996 45:1526 [Google Scholar]
[11]. G Koumudi, S Urmila, Y Chittaranjan, Nutri-genetic Determinants of Neural Tube Defects in IndiaIndian Pediatrics 2009 46:467-75. [Google Scholar]
[12]. IC Verma, Burden of genetic disorders in IndiaIndian J Pediatr 2000 67:893-98. [Google Scholar]
[13]. ML Kulkarni, MA Mathew, B Ramachandran, High incidence of neural-tube defects in South India.Lancet 1987 1:1260 [Google Scholar]
[14]. ML Kulkarni, A Mathew, V Reddy, The range of neural tube defects in southern IndiaArchives of Diseases in Childhood 1989 64:201-04. [Google Scholar]
[15]. S Mini, A Neera, V Shashi, SK Bhargava, Neural tube defects in an East Delhi HospitalIndian Journal of Pediatrics 1991 58:363-65. [Google Scholar]
[16]. B Mahadevan, B Vishnu Bhat, Neural tube defects in PondicherryIndian Journal of Pediatrics 2005 72:557-59. [Google Scholar]
[17]. BM Sharada, A study of neural tube defectsJ Anat Soc India 2010 59(2):162-67. [Google Scholar]
[18]. NM Suresh, Dhananjay Neural Tube DefectsAnatomica Karnataka 2011 5(1):61-64. [Google Scholar]
[19]. B Shanta Kumari, P Rajalaxmi, R Sadananda, Neural Tube Defect: Epidemiologic and Demographic ImplicationIOSR Journal of Dental and Medical Sciences 2014 13(1):1-4. [Google Scholar]
[20]. MR Creasy, ED Alberman, Congenital malformation of the central nervous system in spontaneous abortionJ Med Genet 1976 13:9-16. [Google Scholar]
[21]. LJ Williams, SA Rasmussen, A Flores, RS Kirby, LD Edmonds, Decline in the prevalence of spina bifida and anencephaly by race/ethnicity: 1995-2002Pediatrics 2005 116(3):580-86. [Google Scholar]
[22]. MRC Vitamin Study Research Group. Prevention of neural tube defects: results of the Medical Research Council Vitamin StudyLancet 1991 338:131-37. [Google Scholar]
[23]. RJ Berry, Z Li, JD Erickson, S Li, CA Moore, H Wang, Prevention of neural tube defects with folic acid in China N Engl J Med 1999 341:1485-90. [Google Scholar]
[24]. X Martinez, JM Perez, PA Vazquez, RH Herrera, MR Campos, RA Lopez, Decline of neural tube defects cases after a folic acid campaign in Nuevo Leon, MexicoTeratology 2002 66:249-56. [Google Scholar]
[25]. W Jennifer, TM Cara, M Joe, I Jennifer, JF Timothy, E Mary, F Barbara, Updated Estimates of Neural Tube Defects Prevented by Mandatory Folic Acid Fortification — United States, 1995–2011CDC Morb Mortal Wkly Rep 2015 64(1):1-5. [Google Scholar]
[26]. HB Heseker, JB Mason, J Selhub, IH Rosenberg, PF Jacques, Not all cases of neural-tube defect can be prevented by increasing the intake of folic acidBr J Nutr 2009 102:173-80. [Google Scholar]