Introduction
Erectile dysfunction (ED) has been defined as the inability to achieve/ maintain penile erection which leads to unsatisfactory sexual intercourse [1]. Its incidence increases drastically from about 6% in the age group 20-29 years, to 50-70% in the age group 40-79 years [2]. Its incidence has been projected to increase significantly to over 320 million by the year 2025 [3]. India has been dubbed as the impotence capital of the world due to the high incidence of the life style diseases and probably the largest population of males in the world.
ED therapy utilization rates are still very low and the compliance to therapy is poor [4]. Drug utilization studies (DUS) in ED, in India, are lacking. Given the increasing incidence and prevalence of ED, it is important to have a consensus in the management paradigms for ED and encourage utilization of pharmacological and non-pharmacological therapy for ED.
With above in mind we conducted the study to describe the prevalence pattern of ED, conduct a drug utilization analysis and to find discrepancies between the actual and the recommended management paradigms for ED.
Materials and Methods
Study Design and Ethical Considerations
A retrospective cross-sectional observational study, including a drug utilization analysis (DUA), was conducted after approval of the Patel5Institutional Ethics Committee (IEC). ‘Strengthening the Reporting of Observational Studies in Epidemiology’ (STROBE) guidelines were used in the preparation of protocol and the manuscript.
Study Procedure
Prescriptions of males suffering from ED were selected after obtaining a written informed consent. The patient identification details were kept confidential. The data of the patients attending an andrology clinic, from January 2012 to March 2014, were recorded in structured case record forms. In all, 606 prescriptions were analysed. The sample size was as per the WHO recommendations on conducting a retrospective DUS from medical databases [5].
Data Analysis
The following data were collected:
General patient details like age, gender and marital status.
Patient diagnosis.
Prescription details like date, number of drugs, names of individual drugs (generic/brand), any Fixed Dose Combination (FDC) prescribed, dose, dosage form, dosing schedule, and duration of treatment.
Non pharmacological methods advised.
Assessment of prescription patterns was conducted as per the WHO-INRUD drug use indicators. The pattern of drug used for ED was described as per the DUS metrics as shown below:
The prescribed drugs were classified according to the ‘Anatomical Therapeutic Chemical– Defined Daily Dose’ (ATC/DDD) classification. The Prescribed Daily Dose (PDD) was calculated by taking the average of the daily doses of the drugs prescribed for ED as the PDD. The PDD to DDD ratio was then calculated.
Statistical Analysis
Significant p-value was < 0.05. Statistical calculations were carried out with Open Epi: A Web-based Epidemiologic and Statistical Calculator.
Results
The characteristics of the study subjects are shown in [Table/Fig-1]. The mean age was 42.4 years with a standard deviation (SD) of 10.8 years and the age range of 19 to 72 years.
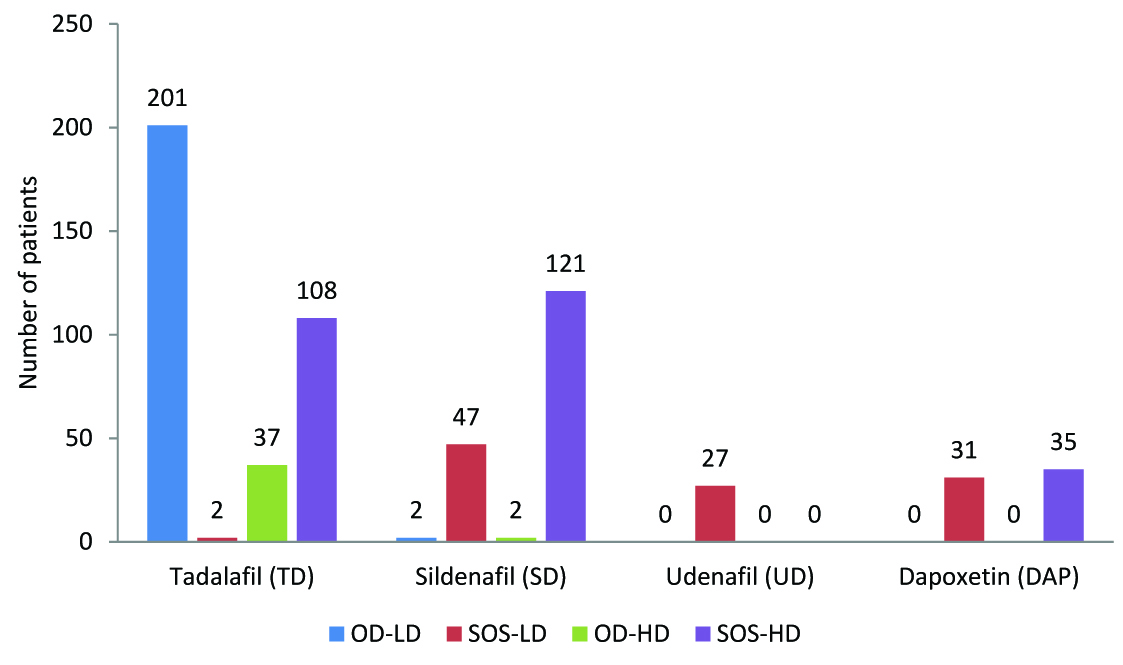
The distribution of various forms of ED as per the age and marital status is given in [Table/Fig-2]. The various modalities of treatment used in different forms of ED are shown in [Table/Fig-3]. The pattern of use of each of the four drugs, Tadalafil, Sildenafil, Udenafil and Dapoxetine, in the form of either once daily dosing (high or low dose) or as an ‘on-demand’ medication (high or low dose), is depicted in the [Table/Fig-4].
Analysis of the prescription pattern as per the WHO-IN RUD drug use indicators: The average number of drugs per prescription was 2.4 ± 1.01 (SD). The average number of drugs for ED per prescription was 2.1 ± 0.8 (SD). There were no prescriptions with more than five drugs. Injections were prescribed in 77/606 (12.7%) of the prescriptions. The fixed dose combination of ‘Sildenafil + Dapoxetine’ and ‘Tadalafil + Dapoxetine’ were prescribed to 15/606 (2.5%) and 20/606 (3.3%), respectively. The fixed dose combinations of various nutritional/ herbal supplements [Table/Fig-3], were prescribed to 126/606 (20.8%) of the patients as supportive therapy. None of the drugs prescribed, except chlorpromazine, were from the National List of Essential Medicines (India).
Drug utilization metrics: The ATC/DDD classification and the PDD are as shown is [Table/Fig-5].
Discussion
Most of the patients in our study were from the age group 30-39 years probably because they opt for treatment more often due to the distress caused by in ED. On the contrary, above 50 years, ED might be considered as a physiological accompaniment and hence they might not visit a doctor [6]. A similar age distribution has been seen in other similar studies [7,8]. The number of cases of grade I ED, as per the Erection Hardness Scoring scale [9], was more than twice the number of cases with grade II ED. Again, the reason could be that only those individuals with very severe ED opt to get treatment. These factors contribute to the low utilization of therapy for ED.
A significant number of individuals with ED had various addictions. The odds having ED were higher in them. Thus, de-addiction will play a big role in the management of ED. The most common co-morbid disorders were urological. Alpha-1 adreno-receptor antagonists (a1RB) and/or 5-alpha reductase inhibitors (RI) are the treatment of choice for lower urinary tract symptoms (LUTS) due to BPH. The RIs may cause ED, ejaculatory disorders and hypoactive sexual disorder (HSD), whereas the 1RBs can induce ejaculatory disorders, but do not lead to HSD or ED. Since, ED is considered more troublesome and significantly affects the quality of sexual performance, first line therapy of BPH induced LUTS should be the a1RBs [10].
The risk factors for cardiovascular disorders and ED are common - atherosclerosis, hypertension, obesity, impaired glucose tolerance, etc. It has been recommended that appropriate screening for and management of cardiovascular disorders be conducted in individuals who present with ED. Use of PDE-5 inhibitors may lead to severe hypotension in individuals on multiple anti hypertensive drugs, especially, α adreno-receptors blockers, and is contraindicated for those on nitrates in any form for angina [11]. Sildenafil, in a dose of 50 or 100 mg should not be taken within 4 hours of α-blocker administration. The same is not true for 25mg dose of Sildenafil and it may be taken at any time in relation to an α-blocker. Tadalafil is contraindicated in patients taking α-blockers except for 0.4 mg Tamsulosin since it is a selective α1A blocker [11]. It is recommended that nitrates be avoided for 24 hours and 48 hours after an individual has taken Sildenafil or Tadalafil, respectively, in order to avoid a precipitous fall in the blood pressure [11].
Drugs like Atenolol and most other antihypertensive drugs can cause sexual dysfunction and/or ED as a side effect [12]. In our study ‘drug induced’ ED was seen in 7.3%. A study conducted by Cordero et al., states that, patients treated with the beta blocker Nebivolol had a lower incidence of ED [13]. Nebivolol has been shown to have a beneficial effect in ED [14] because it has an additional nitric oxide potentiating effect.
In our study, various psychological co-morbidities were seen. Psychotherapy is a powerful tool in the management of ED and often counseling is extremely effective in treating such cases [15].
We found that organic ED (O.ED) was much more common above 40 years, whereas, psychogenic ED (P.ED) was more common below 40 years. Other studies have reported similar findings [16].
All of the prescriptions were complete in all aspects. There was no evidence of polypharmacy, which is defined as the use of more than six drugs per prescription. The use of FDCs containing PDE-5 inhibitors was very miniscule. One of the main constituents of the nutritional/ herbal supplement FDCs was L-arginine. L-arginine is a precursor for endothelial nitric oxide and a defect in this pathway is said to be involved in the pathogenesis of ED and coronary artery disease [17]. But clinical trials of arginine in ED have given mixed results [18]. Another ingredient was pine bark extract containing oral pycnogenol (oligomeric proanthocyanidins), which are said to have a beneficial and synergistic role along with arginine in ED [19].
None of the drugs used for ED were present in the NLEM. They constitute important group of drugs and hence they should be incorporated in the NLEM. There were no potential interactions observed in the prescribed medicines. As per the WHO/ INRUD drug use criteria, overall, the pharmacotherapy was rational [20].
The most commonly prescribed PDE-5 inhibitor drug was Tadalafil, and the least commonly prescribed was Udenafil. Vardenafil was not prescribed to any patient due to its unavailability in India. As far as the utilization of various forms of pharmacotherapy is concerned, there was no statistically significant difference related to the type of ED, except in the case of Udenafil and the combination of Papaverine and Chlorpromazine (Intracavernossal injection of vasoactive drugs – ICIVAD). The guidelines for management of ED don’t promulgate the use of one particular PDE-5 inhibitor over another for the different types of ED [12]. The choice of a particular PDE-5 inhibitor depends more on the pharmacokinetic properties as per one’s individual needs, cost and patient acceptance [11]. Sildenafil is rapidly absorbed and acts within 30 min to one hour; it has a short plasma half-life of approximately four hour and its absorption is decreased by up to 30% and time to peak levels increased by one hour when given with food [21]. Tadalafil on the other hand, reaches peak levels in about two hours; has a half life of about 17 hours and it is negligibly affected by food [22]. It has been observed that Tadalafil has a much lesser propensity to cause a fall in the blood pressure when given in healthy individuals and also when given along with Amlodipine in hypertensive patients [11]. This explains the pattern of use of these drugs observed in our study. The reason for not using Udenafil on a daily basis was its high cost. Udenafil was prescribed only in patients not responding adequately to other PDE-5 inhibitors.
Studies have shown that ED and premature ejaculation often coexist and treatment of both of them simultaneously might lead to better outcomes [23]. Dapoxetine, a selective serotonin reuptake inhibitor, was specifically developed for the treatment of premature ejaculation [24]. Dapoxetine undergoes rapid absorption and elimination resulting in minimal accumulation and is unaffected by multiple dosing. The time required for peak concentration is about 1.4–2.0 hours following oral administration. Its absorption is not affected by food [25]. Hence, it is possible to administer it on an ‘as and when required’ basis, thereby minimizing the potential adverse effects of continuous therapy.
The combination of Papaverine, Chlorpromazine ± Alprostadil, was used as ICIVAD therapy. In our study, the intracavernosal injection of PAP+CPZ was used more often in cases of O.ED compared to P.ED. ICIVAD therapy is tried in individuals not responding adequately to oral drugs or in those who have significant contraindications to PDE-5 inhibitors [26]. We did not use Phentolamine in combination with Papaverine, but instead used Chlorpromazine, because of the high cost and unavailability of Phentolamine and since their efficacies in treating ED are comparable [27]. Studies have shown that ICIVAD therapy may be superior to vacuum assisted erection therapy [28]. Papaverine was initially used as monotherapy, but due its side-effects such as prolonged erection, priapism, and corpus cavernosum fibrosis, solo use was abandoned. As per the current practice, papaverine is given in combination with other vasoactive drugs. This helps to reduce the dose of papaverine to 10-15 mg from the high doses (80-120 mg) used initially. This is due to the synergistic effect of the combination [29].
There were no other studies with which we could compare our results for PDD/DDD ratios. The PDD/ DDD ratio may indicate under (ratio less than one) or over utilization (ratio more than one) of therapy. But before interpretation of PDD/DDD ratios it is very important to have national DDD values based on indigenous data [30].
Overall, the data presented in our study is generalizable as there is concurrence with other similar studies describing the prevalence pattern of ED mentioned above. Being a retrospective DUA, we could not measure the consumed daily dose (actual use) and could not assess the comparative clinical effectiveness and adverse effect profile of various drugs prescribed for ED.
Characteristics of patients (n=606) suffering from erectile dysfunction, visiting an Andrology, clinic, Mumbai 2012-14.
| Sr. No | Characteristics | Grades of Erection Hardness Score* | Total | p-value |
|---|
| Grade I (%) | Grade II (%) |
|---|
| 1 | Age (years) | 18-29 | 76 | 54 | 130 | <0.001 |
| 30-39 | 160 | 89 | 249 |
| 40-49 | 94 | 26 | 120 |
| 50-59 | 56 | 15 | 71 |
| ≥60 | 36 | 0 | 36 |
| 3 | Marital Status | Married | 350 | 126 | 476 | 0.004 |
| Unmarried | 52 | 40 | 92 |
| Widower | 10 | 8 | 18 |
| Divorced | 12 | 8 | 20 |
| 4 | Addictions † | No addictions | 134 | 84 | 218 | 0.001 |
| Addictions | 288 | 100 | 388 |
| 5 | Comorbidity | Cardiovascular | 108 | 46 | 154 | <0.001 |
| Diabetes | 64 | 8 | 72 |
| Urological | 121 | 65 | 186 |
| Psychological | 58 | 44 | 102 |
| Others | 21 | 11 | 32 |
| None | 50 | 48 | 98 |
* There were no patients with EHS above grade 2. † For Addictions, the Conditional Maximum Likelihood Odds ratio is – 0.6 with the upper and lower confidence interval limits being: 0.4 and 0.8(Calculated using Mid P exact test) Addictions: Consumption of tobacco in all forms, alcohol, recreational drug abuse
Distribution of various forms of erectile dysfunction as per age and marital status in a sample of prescriptions of patients (n=606) attending an Andrology clinic, Mumbai 2012-2014.
| Patient Characteristic | Type of ED | p-value |
|---|
| Organic ED (n=276) | Psychogenic ED (n=280) | Mixed ED (n=50) |
|---|
| Age (years) | 18-29 | 21 | 104 | 5 | <0.001 |
| 30-39 | 73 | 151 | 25 | <0.001 |
| 40-49 | 81 | 21 | 18 | <0.001 |
| 50-59 | 67 | 3 | 1 | <0.001 |
| ≥60 | 34 | 1 | 1 | <0.001 |
| Marital status | M | 240 | 200 | 36 | <0.001 |
| U | 21 | 62 | 9 | <0.001 |
| W | 11 | 5 | 2 | 0.3 |
| D | 4 | 13 | 3 | 0.06 |
M - Married; U - Unmarried; W - Widower; D – Divorced
Different modalities of treatment used in various forms of erectile dysfunction in a sample of prescriptions of patients (n=606) attending an Andrology clinic, Mumbai 2012-2014.
| Treatment modality | Erectile dysfunction | Total | p-value |
|---|
| Organic ED (n=276) | Psychogenic ED (n=280) | Mixed ED (n=50) |
| Sildenafil (SD) | 82 | 80 | 10 | 172 | 0.4 |
| Tadalafil (TD) | 168 | 152 | 28 | 348 | 0.3 |
| Udenafil | 22 | 4 | 1 | 27 | 0.001 |
| Dapoxetine (DAP) | 35 | 25 | 6 | 66 | 0.4 |
| SD+DAP | 5 | 7 | 3 | 15 | 0.2 |
| TD+DAP | 12 | 7 | 1 | 20 | 0.4 |
| Inj. Papaverine + Chlorpromazine | 58 | 12 | 1 | 71 | 0.001 |
| Inj. Papaverine + Chlorpromazine + Alprostadil (PGE1) | 4 | 1 | 1 | 6 | 0.3 |
| Enlarge forte | 24 | 31 | 9 | 64 | 0.1 |
| Ignitor | 14 | 18 | 5 | 37 | 0.4 |
| Cavenor | 4 | 8 | 1 | 13 | 0.5 |
| Enlarge | 3 | 9 | 0 | 12 | 0.1 |
Enlarge forte: L-arginine 3gm, pine bark extract 120mg, safed musli 3gm; Enlarge: L-arginine 500 mg, ginseng 42.5 mg, ginkgo biloba extract 20 mg, pinus pinaster bark extract 5 mg; Ignitor: Fenugreek extract 300mg, magnesium 16mg, zinc 15mg, pyridoxine 5mg; Cavenor: L-arginine 1000 mg, proanthocyanidins 20 mg
Pattern of use of various drugs to treat erectile dysfunction in a sample of prescriptions of patients (n=606) attending an Andrology clinic, Mumbai 2012-2014. OD- Once a day; SOS- Whenever required; LD- Low dose; HD- High dose. Tadalafil: LD-5mg, HD-10 & 20mg; Sildenafil : LD-50mg, HD- 100mg; Udenafil: LD- 100mg, HD-200mg; Dapoxetine: LD-30mg, HD-60mg
ATC/DDD classification, PDD values and PDD/DDD ratio of various drugs used to treat erectile dysfunction in a sample of prescriptions of patients (n=606) attending an Andrology clinic, Mumbai 2012-2014
| S No. | Drug | ATC code | DDD(mg) | PDD (mg) | PDD /DDD |
|---|
| 1 | Sildenafil | G04BE03 | 50 | 66.7 | 1.3 |
| 2 | Tadalafil | G04BE08 | 10 | 11 | 1.1 |
| 3 | Udenafil | - | - | 30 | - |
| 4 | Dapoxetine | G04BX14 | 30 | 46.2 | 1.5 |
| 5 | Papaverine | G04BE02 | - | 42.9 | - |
| 6 | Chlorpromazine | N05AA01 | 100 | 19.6 | 0.2 |
| 7 | PGE1/ Alprostadil | G04BE01 | 0.02 | 0.008 | 0.4 |
Summary and conclusion
Drug utilization for ED was less in age groups above 40 years and in those with a milder form of ED. Our study showed that the odds of having ED increased with addictions. Hence, measures for deaddiction will play a very important role. The most common comorbid disorders were urological (BPH, LUTS). In our study, organic ED was much more common above 40 years and psychogenic ED was common below 40 years. Tadalafil was the most commonly prescribed drug for ED. The main factor in the selection of aparticular PDE5 inhibitor was its pharmacokinetics and cost. Udenafil, being the costliest, was the least prescribed. Dapoxetine was used in a significant number of individuals having PE with ED. For ICIVAD therapy, the combination of Papaverine, Chlorpromazine ± Alporstadil was used in patients not responding to oral drugs. Over all, rational pharmacotherapy was observed.
* There were no patients with EHS above grade 2. † For Addictions, the Conditional Maximum Likelihood Odds ratio is – 0.6 with the upper and lower confidence interval limits being: 0.4 and 0.8(Calculated using Mid P exact test) Addictions: Consumption of tobacco in all forms, alcohol, recreational drug abuse
M - Married; U - Unmarried; W - Widower; D – Divorced
Enlarge forte: L-arginine 3gm, pine bark extract 120mg, safed musli 3gm; Enlarge: L-arginine 500 mg, ginseng 42.5 mg, ginkgo biloba extract 20 mg, pinus pinaster bark extract 5 mg; Ignitor: Fenugreek extract 300mg, magnesium 16mg, zinc 15mg, pyridoxine 5mg; Cavenor: L-arginine 1000 mg, proanthocyanidins 20 mg
[1]. National Institutes of Health. Consensus statement on impotenceInt J Impot Res 1992 10:1-33. [Google Scholar]
[2]. EO Laumann, A Nicolosi, DB Glasser, A Paik, C Gingell, E Moreira, Sexual problems among women and men aged 40-80 y: prevalence and correlates identified in the Global Study of Sexual Attitudes and BehaviorsInt J Impot Res17:39-57. [Google Scholar]
[3]. IA Ayta, JB McKinlay, RJ Krane, The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequencesBJU Int. 1999 84:50-56. [Google Scholar]
[4]. H-M Tan, WY Low, CJ Ng, K-K Chen, M Sugita, N Ishii, Prevalence and correlates of erectile dysfunction (ED) and treatment seeking for ED in Asian Men: the Asian Men’s Attitudes to Life Events and Sexuality (MALES) studyJ Sex Med 2007 4:1582-92. [Google Scholar]
[5]. World Health Organization. How to investigate drug use in health facilities: selected health use indicatorsEDM Resear 1993 1(87) [Google Scholar]
[6]. R Shabsigh, Epidemiology of Erectile Dysfunction. In: Mulcahy JJ (ed) Male Sex. Funct. A Guid. to Clin. Manag 2006 2nd EditionTotowa, NJHumana Press:47-59. [Google Scholar]
[7]. SK Gupta, S Dayal, VK Jain, U Kataria, V Relhan, Profile of male patients presenting with psychosexual disorders.Indian J Sex Transm Dis 2004 25:33-37. [Google Scholar]
[8]. R Verma, S Mina, S Ul-Hassan, YPS Balhara, A descriptive analysis of patients presenting to psychosexual clinic at a tertiary care centerIndian J Psychol Med 2013 35:241-47. [Google Scholar]
[9]. I Goldstein, JP Mulhall, AG Bushmakin, JC Cappelleri, K Hvidsten, T Symonds, The erection hardness score and its relationship to successful sexual intercourse.J Sex Med 2008 5:2374-80. [Google Scholar]
[10]. FC Lowe, Treatment of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: sexual functionBJU Int 2005 95(4):12-18. [Google Scholar]
[11]. RA Kloner, Cardiovascular effects of the 3 phosphodiesterase-5 inhibitors approved for the treatment of erectile dysfunctionCirculation. 2004 110:3149-55. [Google Scholar]
[12]. S Kalra, YP Balhara, M Baruah, D Jumani, K Kochhar, S Majumdar, G Makker, A Saxena, H Zaveri, N Agrawal, Consensus guidelines on male sexual dysfunction.J Med Nutr Nutraceuticals 2013 2(5) [Google Scholar]
[13]. A Cordero, V Bertomeu-Martínez, P Mazón, L Fácila, V Bertomeu-González, P Conthe, Erectile dysfunction in high-risk hypertensive patients treated with beta-blockade agentsCardiovasc Ther. 2010 28:15-22. [Google Scholar]
[14]. K Brixius, M Middeke, A Lichtenthal, E Jahn, RHG Schwinger, Nitric oxide, erectile dysfunction and beta-blocker treatment (MR NOED study): benefit of nebivolol versus metoprolol in hypertensive men.Clin Exp Pharmacol Physiol 2007 34:327-31. [Google Scholar]
[15]. . Bagadia, A Study of 258 Male Patients With Sexual ProblemsIndian J Psychiatry 1972 14(143.) [Google Scholar]
[16]. LA Panser, T Rhodes, CJ Girman, HA Guess, CG Chute, JE Oesterling, Sexual function of men ages 40 to 79 years: the Olmsted County Study of Urinary Symptoms and Health Status Among MenJ Am Geriatr Soc 1995 43:1107-11. [Google Scholar]
[17]. FC Tanner, G Noll, CM Boulanger, TF Lüscher, Oxidized low density lipoproteins inhibit relaxations of porcine coronary arteries. Role of scavenger receptor and endothelium-derived nitric oxideCirculation. 1991 83:2012-20. [Google Scholar]
[18]. D McKay, Nutrients and botanicals for erectile dysfunction: examining the evidence.Altern Med Rev 2004 9:4-16. [Google Scholar]
[19]. DF Fitzpatrick, B Bing, P Rohdewald, Endothelium-dependent vascular effects of PycnogenolJ Cardiovasc Pharmacol 1998 32:509-15. [Google Scholar]
[20]. F Sjöqvist, D Ph, D Birkett, Drug Utilization 2003 76(84) [Google Scholar]
[21]. DJ Nichols, GJ Muirhead, JA Harness, Pharmacokinetics of sildenafil after single oral doses in healthy male subjects: absolute bioavailability, food effects and dose proportionalityBr J Clin Pharmacol 2002 53(1):5S-12s. [Google Scholar]
[22]. ST Forgue, BE Patterson, AW Bedding, CD Payne, DL Phillips, RE Wrishko, Tadalafil pharmacokinetics in healthy subjectsBr J Clin Pharmacol 2006 61:280-88. [Google Scholar]
[23]. EA Jannini, AM Isidori, A Aversa, A Lenzi, SE Althof, Which is first? The controversial issue of precedence in the treatment of male sexual dysfunctionsJ Sex Med 2013 10:2359-69. [Google Scholar]
[24]. L Sorbera, J Castaner, R Castaner, Dapoxetine hydrochlorideDrugs Futur. 2004 29:1201-05. [Google Scholar]
[25]. NB Modi, MJ Dresser, M Simon, D Lin, D Desai, S Gupta, Single- and multipledose pharmacokinetics of dapoxetine hydrochloride, a novel agent for the treatment of premature ejaculation.J Clin Pharmacol. 2006 46:301-09. [Google Scholar]
[26]. BJ De Boe, AA Lycklama a Nijeholt, HA Kleinjans, [Intracavernous auto-injection therapy with papaverine phentolamine via an auto-injection pen for patients with an erectile dysfunction: similar results achieved in family practice and urology].Ned Tijdschr Geneeskd 2001 145:783-87. [Google Scholar]
[27]. R Shamloul, M El-Dakhly, H Ghanem, A Gadallah, H Mokhtar, Intracavernous chlorpromazine versus phentolamine: a double-blind clinical comparative study.J Sex Med 2004 1:310-13. [Google Scholar]
[28]. DW Soderdahl, JB Thrasher, KL Hansberry, Intracavernosal drug-induced erection therapy versus external vacuum devices in the treatment of erectile dysfunction.Br J Urol 1997 79:952-57. [Google Scholar]
[29]. H Hedlund, P Hedlund, Pharmacotherapy in erectile dysfunction agents for selfinjection programs and alternative application modelsJ Urol Nephrol Suppl 1996 179:129-38. [Google Scholar]
[30]. KB Thakkar, MM Jain, G Billa, A Joshi, AA Khobragade, A drug utilization study of psychotropic drugs prescribed in the psychiatry outpatient department of a tertiary care hospitalJ Clin Diagn Res 2013 7:2759-64. [Google Scholar]