Anesthesia for a Rare Case of Uncorrected Pentalogy of Fallot Undergoing Craniotomy and Drainage of Brain Abscess
Vinay Marulasiddappa1, B.S. Raghavavendra2
1Associate Professor, Department of Anaesthesia, Bangalore Medical College and Research Institute, Bengaluru, India.
2Assistant Professor, Department of Anaesthesia, Bangalore Medical College and Research Institute, Bengaluru, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vinay Marulasiddappa, Associate Professor, Department of Anaesthesia, Bangalore Medical College and Research Institute, Fort, KR Road, Bengaluru 560002, India.
E-mail: drvinaym@gmail.com
Children with uncorrected cyanotic congenital heart diseases can present for non cardiac surgeries. They pose several challenges to the Anaesthesiologist, especially when they are posted for emergency surgery, due to the complex haemodynamic changes secondary to the heart disease. Pentalogy of Fallot (POF) is a rare form of congenital heart disease characterized by the association of Tetralogy of Fallot (TOF) with an atrial septal defect (ASD). TOF is the leading cause of intracardiac right to left shunt and is the commonest type of cyanotic congenital heart disease to cause a brain abscess. Children with POF presenting with brain abscess pose several challenges to the anaesthesiologist due to the altered haemodynamics and warrant a meticulous anaesthetic plan. There are very few case reports of Anaesthesia management of a child with Pentalogy of Fallot (POF) presenting for non cardiac surgery. We report the anaesthetic management of a rare case of a 5-year-old child with uncorrected POF, who presented to our Superspeciality hospital with a brain abscess and underwent an emergency craniotomy with drainage of the brain abscess successfully.
Cyanotic congenital heart disease, Intracardiac shunt, Intracerebral abscess, Neurosurgery
Case Report
A 5-year-old male child weighing 10 kg presented to the Neurosurgery Department of our Superspeciality hospital in December 2014 with 15 days history of fever, headache, vomiting and two episodes of generalized tonic-clonic seizures. Child had been diagnosed with heart disease at the age of one year and also had history of squatting episodes for the last two years. Although parents had been advised further evaluation at a cardiac centre, no evaluation had been undertaken due to financial constraints and child was not on any treatment for his cardiac condition. There were no past medical reports available. General physical examination revealed clubbing of fingers, growth impairment and poor general condition. Examination of cardiovascular system revealed a pan systolic murmur heard all over the precardium. Respiratory system was normal. Electro cardiogram (ECG) showed right axis deviation with sinus rhythm. Blood tests revealed a Haemoglobin level of 14.9 g/100ml and a raised Total Count (TC) of 22,500 cells/cumm. Other serum biochemical parameters were within normal limits. Computed Tomography (CT) scan of the brain revealed a well defined thin walled rim enhancing lesion in the left temporo-parietal lobe region with mass effect, probably pyogenic/tubercular abscess with ventriculitis [Table/Fig-1].
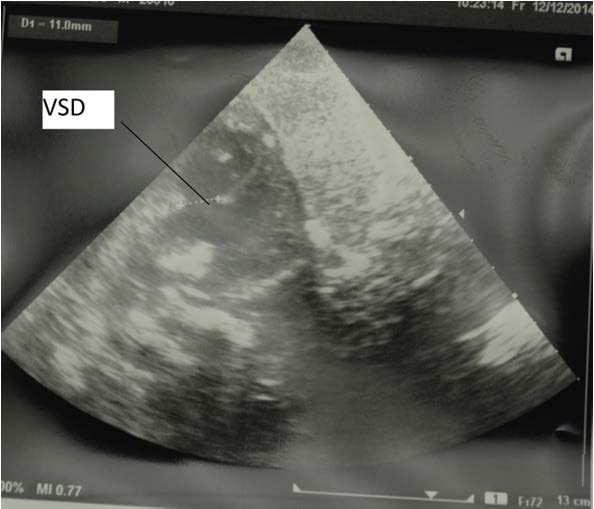
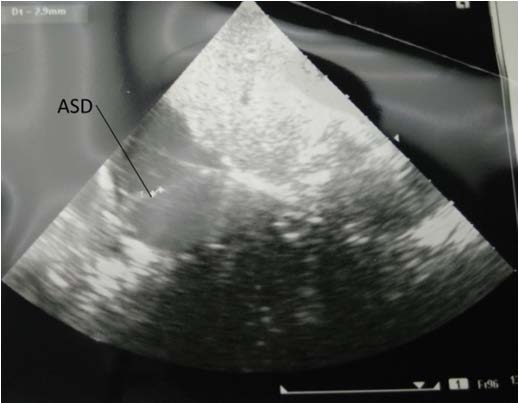
2D Echocardiography [Table/Fig-2,3] showed: Congenital Heart Disease, Pentology of Fallot (Ostium Secundum type atrial septal defect with Left-Right shunt, Sub-Aortic Ventricular Septal Defect with bidirectional shunt, Inter ventricular septum over-riding of Aorta, Right ventricular hypertrophy, pulmonary valve stenosis). Normal biventricular function. Severely increased trans-pulmonic valve velocity and pressure gradients. Patient was started on IV Antibiotics, anticonvulsants and anti-oedema treatment. After obtaining informed consent from parents, child was posted for emergency craniotomy and drainage of left Temporo-parietal lobe abscess. Ceftriaxone 200 mgs IV was given as prophylaxis against Infective Endocarditis one hour prior to surgery.
In the operating theatre, patient was connected to standard monitors such as ECG, Non-invasive blood pressure (NIBP), Pulse oximetry (SpO2) and End-Tidal CO2 (EtCO2). Two large bore peripheral IV cannulae (20 gauge) were inserted. After pre-oxygenation, patient was induced with Fentanyl 20 mcgs and Ketamine 20 mgs. Patient was intubated with size 5 endotracheal tube after Vecuronium 2 mgs. Arterial line was secured with 22 gauge cannula inserted into the left radial artery to monitor arterial blood pressure (ABP).Central venous pressure (CVP) was monitored by inserting double lumen CVP catheter into the right subclavian vein.
Foley catheter was also inserted to monitor urine output. Anaesthesia was maintained with Isoflurane, Oxygen, air along with intermittent bolus doses of Vecuronium and fentanyl.Craniotomy was performed and abscess was completely drained. Patient remained stable thouroughout the procedure with heart rate between 100-120/ min, Systolic BP between 80-100 mm Hg, SpO2 between 98 to 100 % and EtCO2 was maintained between 30-33. Surgery lasted nearly two hours with blood loss estimated at 150 mls which was replaced. At the end of the surgery, residual neuro-muscular block was reversed and patient was extubated when fully awake in the operating theatre. Patient was then shifted to Neurosurgical ICU for observation, shifted to the ward 24 hours later. Child was successfully discharged from the hospital after making a full recovery.
Discussion
Pentalogy of Fallot (POF) is the association of Tetralogy of Fallot (TOF) with an atrial septal defect (ASD). The most common type of ASD found with POF is ostium secundum (OS), followed by the primum ASD [1]. Our patient had an ostium secundum type of ASD. Tetralogy of Fallot is the most common congenital heart disease causing intracardiac right–left shunts. Ventricular septal defect (VSD), Overriding of the aorta, Pulmonary artery outflow obstruction and right ventricular hypertrophy are the characteristic features of this condition [2,3]. It is well recognized that patients with cyanotic CHD are prone to develop brain abscesses. Right to left shunting bypasses the filtering process of the pulmonary capillaries and thereby leads to higher incidence of systemic infections such as brain abscesses. TOF is the most common cyanotic CHD associated with intracranial suppuration [4].
These patients suffer from chronic hypoxia, resulting in polycythaemia, which in turn can lead to thrombotic complications coagulopathies, occasionally congestive heart failure and perioperative cyanotic spells. One of the most important factor that determines the amount of blood that is shunted thorough the VSD in POF is the ratio of systemic vascular resistance (SVR) to Pulmonary vascular resistance (PVR). Greater the SVR and lesser the PVR, lesser will be the shunt. An important factor determining pulmonary blood flow is the presence of infundibular or valvular pulmonary stenosis [5].
It is crucial to avoid perioperative cyanotic spells due to spasm of the hypertrophied pulmonary infundibulum, as this will severely increase PVR and worsen the right to left shunt. Tachycardia and increased myocardial contractility can lead to infundibular spasm. Another mechanism for such hyper cyanotic episodes is decreased SVR increasing right to left shunting through VSD. Systemic blood pressures less than 60 mmHg can trigger hyper cyanotic episodes [5].
The Anaesthetic goals are 1) to avoid hypoxemia; 2) ensuring adequate hydration; 3) maintaining systemic arterial blood pressure by maintaining SVR; 4) minimizing additional resistance to pulmonary blood flow (minimizing PVR); and 5) avoiding sudden increase in systemic oxygen demand (cry, inadequate level of anesthesia, seizure). Achieving these Anaesthetic goals will ensure prevention of worsening right to left shunting, but ensuring adequate perfusion to the already hypertrophied right ventricle and at the same time maintain collateral circulation into the lungs [6].
Induction of Anaesthesia can cause vasodilatation and the resultant fall in SVR can worsen the right to left shunt. We used Ketamine as the induction agent as it has been found to be an excellent induction agent in such cases as it improves the oxygenation by decreasing the right to left shunt as a result of increase in SVR [7]. Neurosurgical requirements such as lax brain and maintenance of adequate cerebral perfusion pressure (CPP) are important. However, cautious use of diuretics such as mannitol is warranted to prevent dehydration. CPP can be maintained by maintaining adequate systemic blood pressure. Adequate measures to prevent air embolism such as avoiding air bubbles in the IV lines is crucial as there is a high risk of paradoxical air embolism due to right to left shunt [3,8]. In many ways, the Anaesthetic management of children with POF is similar to TOF, sharing similar concerns. However, there are very few case reports on anaesthesia management of POF due to its rare occurrence.
CT scan of the brain showing a well defined, thin walled lesion in the left temporo-parietal lobe region, probably an abscess with ventriculitis

2D Echocardiography showing a large sub-aortic VSD
2D Echocardiography showing ASD
Conclusion
Anaesthesia management of children with POF presenting for neurosurgery requires a thorough understanding of the pathophysiology of this condition and the altered haemodynamics. A successful outcome in such cases requires a meticulous preoperative assessment of the patient to assess the severity of the underlying heart disease and the associated complications. It is crucial to optimize the condition of the patient with appropriate treatment as we did in our case with antibiotics, anticonvulsants and anti-oedema treatment before surgery. A cautious and meticulous anaesthetic plan to maintain haemodynamic stability along with anaesthetic goals such as avoiding hypoxia, ensuring adequate hydration, maintaining SVR, minimizing PVR and avoiding increases in oxygen demand along with due considerations for neurosurgery is crucial for a successful outcome.
[1]. SP Singh, S Chauhan, S Talwar, Sinus venosus atrial septal defect in a patient with Pentalogy of FallotAnn Card Anaesth 2012 15:166-68. [Google Scholar]
[2]. K Sandhya, S Shivanna, CA Tejesh, N Rathna, Labour analgesia and anaesthetic management of a primigravida with uncorrected Pentology of FallotIndian J Anaesth 2012 56:186-88. [Google Scholar]
[3]. K Dilesh, K Cheran, GG Kumar, IP Chandy, Anaesthetic Management of Tetralogy of Fallot Coming for non-Cardiac Surgery: A Case ReportJournal of Evolution of Medical and Dental Sciences 2015 4(23):4029-32.DOI: 10.14260/jemds/2015/579 [Google Scholar]
[4]. JD Pandian, NV Moosa, PJ Cherian, K Radhakrishnan, Brainstem abscess complicating tetralogy of Fallot successfully treated with antibiotics aloneNeurol India 2000 48:272-75. [Google Scholar]
[5]. I Naqash, B Ahad, J Zargar, A Kirmani, M Wani, Anaesthetic Management Of A Case Of Tetrology Of Fallot For Drainage Of Brain Abscess: A Case ReportThe Internet Journal of Anesthesiology 2002 7(1) [Google Scholar]
[6]. F Fazeli, H Baharvahdat, S Mashhadi, Hypercyanotic spell after general anesthesia in Tetralogy of FallotThe Internet Journal of Anesthesiology 2006 13(1) [Google Scholar]
[7]. MS Kurdi, KA Theerth, RD Deva, Ketamine: Current applications in anesthesia, pain, and critical careAnesth Essays Res 2014 8(3):283-90. [Google Scholar]
[8]. DK Baidya, BR Ray, PM Singh, Labour analgesia and anaesthetic management of a primigravida with uncorrected pentalogy of fallot: Few concernsIndian J Anaesth 2013 57:102-03. [Google Scholar]