Puerperal infection is a common complication of labour. It occurs universally and is usually responsive to first line antibiotics. However, resistance to first line antibiotics and even second line antibiotics is becoming more wide spread. We report a case of puerperal infection caused by carbapenem resistant organisms leading to prolonged fever and hospitalisation. A 28-year-old primigravida, following caesarean section done elsewhere, for elevated blood pressure presented with high grade fever. The patient was treated with antibiotic to which she failed to respond. She underwent laparotomy twice and only improved after Colistin was combined with Meropenam, based on urine and pus culture reports.
Drug resistance, Fever, Laparotomy, Puerperal infection
Case Report
A 28-year-old primigravida underwent a caesarean section, at term, elsewhere, for pre-eclampsia. She underwent a laparotomy on the second postoperative day for suspected intraperitoneal haemorrhage during which she was transfused 2 units of blood. She was admitted to Christian Medical College Hospital in December 2014 with history of fever since the 12th postoperative day (of the caesarean section) and swelling of the legs. Notes from her previous admission showed she had pleural effusion, hepatomegaly, moderate ascites and gross right sided hydronephrosis on imaging. Analysis of the pleural and ascitic fluid showed an elevated leukocyte count with neutrophilic predominance. The ascitic fluid culture showed extended spectrum beta lactamase (ESBL) producing organisms for which she was given Amoxycillin/Clavulanic acid combination. As her fever persisted, she was referred here for further management. On admission, she had low grade fever with tachycardia and tachypnoea. Clinically there was no evidence of endometritis, peritonitis or surgical site infection. Pelvic examination revealed bogginess in the Pouch of Douglas. After sending blood counts, Cultures, renal and liver function tests, she was empirically started on Meropenam.
Ultrasound and CT scan done showed fluid collection of 85x57mm (approximately 260cc) in the upper pelvis, between the uterus and rectum, tracking anteriorly on the left side, to form loculated fluid pockets with enhancing walls deep to the parietal wall in lower abdomen, on both sides of the midline. A left sided pleural effusion and an obstructing right renal calculus with gross right hydronephrosis and parenchymal thinning were also noted. As she continued to have fever, a culdocentesis and CT guided drainage of the collection were attempted but both yielded only small amounts of purulent fluid. As the attempts to drain the collection non-surgically were unsuccessful and her fever persisted, she underwent laparotomy on the 31st day after the initial caesarean section. The findings were that the uterus was enlarged to about 14 week’s size. The posterior aspect of the uterus was covered with densely matted bowel loops. The cornual ends of the uterus were adherent to the anterior abdominal wall. The uterine incision was open and the edges were necrotic. There was 50-60 ml of pus in the pouch of douglas. Upper abdomen was walled off by adhesions. The necrotic edges of the LSCS incision were debrided and peritoneal lavage was done.
Urine culture grew E. coli and pus culture grew E. coli and Enterococcus. The E. coli was resistant to all first line and second line drugs and was susceptible to only Tigicyline and Colistin. E.coli was isolated from pus sample of the patient and followed up for the complete characterization of the isolate for antibiotic susceptibility testing profile. Antibiotic susceptibility testing was done for the following antibiotics cefpodoxime (10 μg/ml), gentamicin (10 μg/ml), augmentin (20/10μg/ml), trimethoprim-sulfamethoxazole (1.25/23.75μg/ml), chloramphenicol (30 μg/ml), amikacin (30 μg/ml), piperacillin/tazobactam (100/10 μg/ml), imipenem (10 μg/ml), meropenem (10 μg/ml), colistin (10 μg/ml) and Tigicyline (15 μg/ml). Antibiotic susceptibility testing revealed, isolated E.coli strain was resistant to the entire antibiotics tested except colistin, tigicyline and chloramphenicol. ESBL characterization was carried out for this strain, using cefotaxime with and without Clavulanic acid was indeterminate. Carba NP assay which is a confirmatory test for carbapenemase producers (as per CLSI guidelines, M100-S25) showed the presence of carbapenemase. Additionally, synergism testing of meropenem with EDTA disk synergy for metallo-β-lactamase detection showed positive (>5mm in diameter).
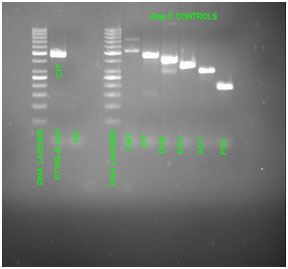
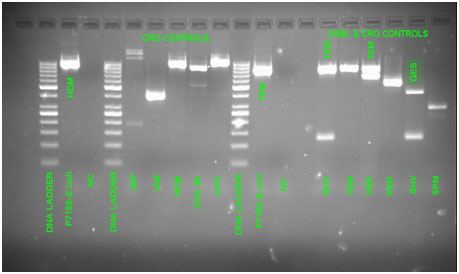
Molecular characterization of the isolate was carried out for AmpC (CMY,CIT,DHA,ACC,ACT,FOX), ESBL (SHV,TEM,VEB,PER,GES,SPM) and CRO (IMP,VIM,NDM,OXA-48,KPC) genes. The tested profile showed the presence of following genes CIT, TEM, and NDM [Table/Fig-1,2]. As the complete characterization showed, the E.coli strain harboured AmpC, Extended Spectrum and carbepenemase genes and exhibited multidrug resistant profile. Interestingly, E.coli isolated from urine and pus tissue samples of the same patient showed thesame antibiotic susceptibility and gene profile.
In accordance to the microbiological culture work up the patient was initiated on Colistin in addition meropenem. Meropenem was given parenterally for 22 days (1 gm IV q Q8H) for a total of 22 days and Colistin administered parenterally for 17 days (3 million units Q8H). Gradually her fever subsided and she was discharged in good condition.
Discussion
The WHO Technical Working Group for Management and Prevention of Maternal infections defines puerperal sepsis as “Infection of the genital tract occurring at any time between the onset of the rupture of membranes or labour and the 42nd day postpartum in which two or more of the following are present- pelvic pain, fever, abnormal vaginal discharge, abnormal odour of discharge or delay in the rate of reduction of size of the uterus (<2cm during the first two days)” [1].
Puerperal sepsis is responsible for about 15% of all ICU admissions [2]. Across the world it is responsible for 2.1%-13.2% of maternal deaths with the higher range being seen in Asia [3,4]. One study showed that there was a mortality rate of 41.7% in patients admitted to ICU with postabortal or puerperal sepsis [5]. The aetiology of puerperal sepsis is polymicrobial with the most common organisms being Group A streptococcus, Staphylococcus, Escherichia coli, Enterobacteriaceae including Klebsiella pneumonia, Pseudomonas, Enterobacter and others like Bacteroides and mycoplasma [6].
Predisposing factors are also many and include medical conditions like anaemia, HIV, diabetes mellitus, prolonged rupture of membranes and subsequent prolonged labour with multiple pelvic examinations, caesarean section, retained products and postpartum haemorrhage. Broad spectrum antibiotics should be initiated as early as possible along with supportive care. A combination of clindamycin with ampicillin and gentamycin is a reasonable choice. Alternatives include piperacillin/tazobactam or carbapenems with clindamycin. Failure to respond to this treatment regime by 48-72 hours warrants a change in antibiotics and a search for other sources of infection. Antibiotic resistance rates vary between 20 and 25 %. In a study done by Kankuri et al., it was found that most of the organisms were susceptible to first or second generation cephalosporins. They suggested narrower spectrum antibiotics based on the culture reports to prevent resistance [2].
Injudicious use of antibiotics has led to extensive antibiotic resistance. Extended spectrum beta lactamase producing organisms (ESBL) and more recently carbapenem resistant organisms (CRO) are causing significant mortality and morbidity worldwide. These infections are common in intensive care settings, with prolonged hospitalisation, long standing use of indwelling catheters/devices and immunocompromised patients. Recognition of CRO’s requires knowledge of these risk factors as well as need for appropriate laboratory facilities for microbial isolation and identification. Members of the Enterobacteriaceae family such as Escherichia coli, Klebsiella spp., and Enterobacter spp are among the common organisms responsible for puerperal sepsis and resistance to the carbopenem class of drug, mediated primarily by plasmid-mediated carbapenemases, is becoming widespread in many areas [7]. This means that obstetricians need to be aware of this entity in order to take appropriate action when the problem arises.
The patient who presented to our hospital was febrile with tachycardia. In some cases with Group A streptococcus infection can present with various symptoms such as fever with chills and hypotension. In addition they may present with abdominal pain [8] or even myocardial dysfunction [9].
To treat patients with carbopenem resistant organisms there is a need for better treatment options and adequate infection control Measures to prevent of spread of CROs include proper hand washing, asepsis during delivery/surgery, judicious use of antibiotics, isolation of cases and education of healthcare personnel and the public. To our knowledge there are few, if any cases of puerperal sepsis in which causative organism was conclusively proven to be a carbopenem resistant organism. In the case we report the diagnosis was dependent on prompt and accurate antibiotic susceptibility patterns provided by the microbiology laboratory in our hospital. Failing which; appropriate antibiotics would not have been initiated and the patient may have had a less than satisfactory outcome.
Gel Profile for AmpC genes
Gel profile for ESBL and Carbapenemase genes
Conclusion
In patients who fail to respond to first and second line antibiotics it would be wise to anticipate the possibility of a carbopenem resistant organism.
[1]. World Health Organization, Department of Making Pregnancy Safer, International Confederation of Midwives. Education material for teachers of midwifery: midwifery education modules. 2008 Geneva [Switzerland]World Health Organization : International Confederation of Midwives [Google Scholar]
[2]. E Kankuri, T Kurki, P Carlson, V Hiilesmaa, Incidence, treatment and outcome of peripartum sepsisActa Obstet Gynecol Scand 2003 82(8):730-35. [Google Scholar]
[3]. BR Ganatra, KJ Coyaji, VN Rao, Too far, too little, too late: a community-based case-control study of maternal mortality in rural west Maharashtra, IndiaBull World Health Organ 1998 76(6):591 [Google Scholar]
[4]. KS Khan, D Wojdyla, L Say, AM Gülmezoglu, PF Van Look, WHO analysis of causes of maternal death: a systematic reviewThe Lancet 2006 367(9516):1066-74. [Google Scholar]
[5]. DR Karnad, V Lapsia, A Krishnan, VS Salvi, Prognostic factors in obstetric patients admitted to an Indian intensive care unit.Crit Care Med 2004 32(6):1294-99. [Google Scholar]
[6]. D Maharaj, Puerperal pyrexia: a review. Part I.Obstet GynecoSurv 2007 62(6):393-99. [Google Scholar]
[7]. E Bilavsky, MJ Schwaber, Y Carmeli, How to stem the tide of carbapenemaseproducing Enterobacteriaceae?: proactive versus reactive strategiesCurr Opin Infect Dis 2010 23(4):327-31. [Google Scholar]
[8]. MT Busowski, M Lee, JD Busowski, K Akhter, MR Wallace, Puerperal Group A Streptococcal Infections: A Case Series and Discussion.Case Rep Med 2013 :2013-751329. [Google Scholar]
[9]. MA Mazzeffi, KT Chen, Severe postpartum sepsis with prolonged myocardial dysfunction: a case reportJ Med Case Reports [Internet 2015 Mar 31 4:318. [Google Scholar]