Radicular cyst is one of the most commonly occurring cyst in the oral cavity it is usually preceded by trauma or an infectious condition which is followed by enlargement. In recent times there are several treatment procedures that are being applied in order to improve the postoperative condition and to accelerate the process of healing and regeneration in the affected site. A 22-year-old patient reported to our OPD with the chief complaint of swelling on the left side of the face since 2-3 months, on investigating it was diagnosed as Radicular cyst which was initially treated by endodontic treatment of the involved tooth followed by enucleation of the cyst further an apicoectomy was done. Finally a PRF and iliac crest graft was placed for aesthetic rehabilitation with 21.
Apicoectomy, Aesthetic rehabilitation, Enucleation, Regeneration, Repair
Case Report
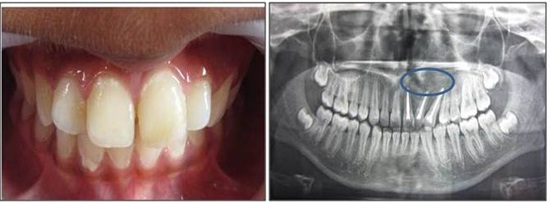
A 22-year-old male patient reported to the Out Patient Department at Sharad Pawar Dental College, Wardha with the chief complaint of swelling on the left side of the face since 2-3 months. There was history of fractured 21 due to bicycle accident. The patient was fine initially, after one month he experienced pain and sensitivity which increased on taking cold beverages and relived on its withdrawal; after which he noticed pea sized swelling on the palatal surface and then reported for the same to our hospital. On extra oral examination a diffuse swelling was observed which was ill-defined in nature [Table/Fig-1]. On intraoral examination Ellis class II fracture was seen in relation to 21 [Table/Fig-2].

Intraoral view showing factured 21

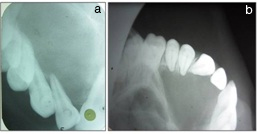
A swelling was seen on the bucco-gingival area extending upto the palatal surface in relation with 21 which was approximately 0.5x0.5cm, oval in shape having colour same as that of adjacent mucosa [Table/Fig-3]. On the basis of clinical evaluation we arrived to a provisional diagnosis of Radicular cyst with 21. Several investigations were carried out in order to obtain a confirmatory diagnosis namely, IOPA which was suggestive of a well-defined radiolucent line involving 21,22,23,24,25 appearing radiolucent in nature & an occlusal radiograph suggestive of the same [Table/Fig-4a,b].
Intraoral view showing site of lesion

Radiographic view showing site of lesion in an IOPA and occlusal view which appears as radiolucent area
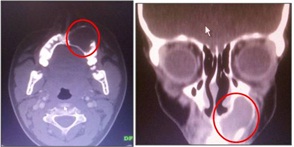
OPG confirmed our diagnosis and supplemented by showing deviation of 23,24 in order to accommodate the radiolucent mass which was a typical finding in present case [Table/Fig-5]. On performing Fine Needle Aspiration Cytology (FNAC) it showed straw coloured fluid was collected and cytology confirmed presence of paucicellular cells like polymorphs, macrophages and few squamous epithelial cells. CT scan in axial and coronal view suggested radiolucent growth in relation to left side of maxilla involving 21,22,23,24 [Table/Fig-6].
An orthopentogram showing radiolucency in relation 21,22,23,24

CT scan in an axial and coronal section showing radiolucent lesion on apical area of maxillary anteriors
Electric Pulp Test with 21,22,23, showed negative result which was same for hot as well as cold vitality tests performed clinically. On the basis of clinical, radiological and cytological investigations Radicular Cyst was diagnosed.
On the basis of above diagnosis further treatment was planned. Written consent was taken from the patient and was informed about the procedure to be carried out. Root canal therapy followed by surgical enucleation of the cystic lesion [Table/Fig-7] and apicoectomy with 21, 22 ,23 was carried out under general anaesthesia. Steps in Preparation of platelet rich fibrin (PRF) [Table/Fig-8].
Enucleation of the cyst under ga, excised cystic specimenalong with syringe containing cystic fluid

Steps preparation of platelet rich fibrin (prf)
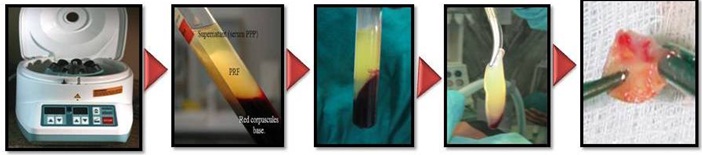
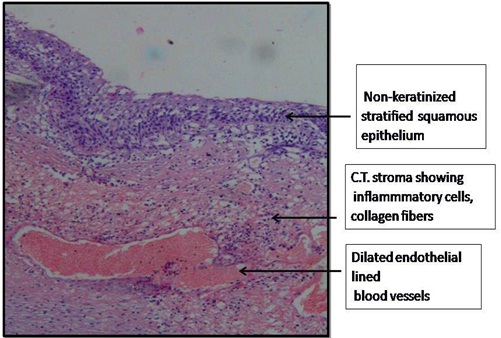
Nearly 5 ml of whole venous blood was collected in two sterile vacutainer tubes of 6 ml capacity without anticoagulant. The vacutainer tubes were then placed in a centrifugal machine at a speed of 3000 revolutions per minute (rpm) for 10 minutes. After centrifugation collected blood settled into the following layers: red lower fraction containing red blood cells, upper straw coloured cellular plasma and the middle fraction containing the fibrin clot as shown in [Table/Fig-8]. The upper straw coloured layer was removed and middle fraction was collected, 2 mm below lower dividing line, known as PRF. Mechanism of formation: fibrinogen reacts with circulating thrombin to form fibrin between red corpuscles at the bottom and acellular plasma at top. Platelets were trapped avidly in the fibrin meshes. PRF and iliac bone graft was placed in defect followed by suturing [Table/Fig-9]. Finally aesthetic rehabilitation with 21 was accomplished by tooth coloured restorative material. The obtained specimen was then grossed for histopathological diagnosis that showed features suggestive of Radicular Cyst [Table/Fig-10]. On patient’s evaluation after 3 months, OPG showed increased radiopacity as compare to earlier radiograph and good amount of regeneration, repair at the site of injury was also appreciated which could be subjected to the use of PRF and Iliac bone graft [Table/Fig-11].
Apicoectomy followed by PRF & iliac bone graft placement followed by suturing

Histopathological view showing features of radicular view under 10x
Postoperative evaluation of patient clinically and radiographically to evaluate healing and regenerative process 3 months later
Discussion
Radicular cysts are those which arise from epithelial residues in the periodontal ligament as a consequence of inflammation, usually following death of dental pulp. They are the most common odontogenic cyst affecting Maxilla more than three times the mandible. The process of pathogenesis of a cyst begins by initiation which gradually progresses to cyst formation and then enlarges to involve the adjacent bone and other vital structures in its surrounding. The toxins from necrotic pulp present here exit at the apex of the tooth, leading to periapical inflammation [1]. There are several treatment options to treat the cyst such as endodontic treatment followed by enulecation and marsupi alization [2].
The postsurgical process involves two main factors Regeneration and Repair (In a study by Ross, Platelets have regenerative potential) [3]. Regeneration has been defined as the reproduction or reconstitution of a lost or injured part to restore the architecture and function of the periodontium [4]. It is possible with growth factors and bone grafts. Need for biological modulators resulted in development of Platelet Rich Plasma (PRP) by Whitmen et al.
Platelet rich factor has given new revolutionary step in the platelet gel therapeutic concept. Attempts to accumulate platelets and released cytokines in a fibrin clot [5]. Platelet rich fibrin (PRF) is a fibrin matrix in which platelet cytokines, growth factors, and cells are trapped and released after a certain time that can serve as a resorbable membrane. Autologous PRF is considered to be a healing biomaterial. Present studies have shown its application in various disciplines of dentistry.
Ross et al., introduced platelets regenerative potentiality described a growth factor from platelets [3]. After activation of the platelets which are trapped within fibrin matrix, growth factors release and stimulate the mitogenic response in the bone periosteum during normal wound healing for repair of the bone. Better understanding of physiologic properties of platelets in wound healing since last two decades led to increase its therapeutic applications in the various forms showing varying results [3]. PRF has several advantages such as it does not require any biochemical handling of blood and also economic. Slow polymerization which is observed during PRF processing leads to the intrinsic incorporation of platelet cytokines and organic chains in the fibrin mesh to bring about efficient cell migration. This result implies that PRF, unlike the other platelet concentrates would be able to release more cytokines during fibrin matrix remodelling. Such a mechanism might explain clinically observed healing properties of PRF. PRF has a supportive effect on the immune system [6,7]. Several types of bone grafts are used such as autogenous graft, allogeneic graft, alloplastic graft and xenogeneic graft. There are several bone grafts that are used for the purpose of osteoinduction, osteoconduction and osteoproliferation. Bone grafts alone without a blood clot or angiogenic factors are unlikely to promote sufficient periapical wound healing. PRF in the form of a platelet gel can be used in conjunction with bone grafts [1]. Besides promoting wound healing, bone growth & maturation, PRF with bone graft has advantages of graft stabilization, wound sealing, haemostasis and improved handling properties [4]. The success of spontaneous bone healing is directly related to the size of bony defects, the anatomical location, the patient’s age and other parameters. Many researches advocated the filling of the remaining cystic cavities with bone grafts [8].
In various bone reconstruction procedures Choukroun's PRF can provide a possible new bone. Mazor et al., stated that use of PRF as the sole filling material during a simultaneous sinus lift and implantation procedure has stabilized a good amount of regenerated bone in the subsinus cavity up to the tip of implants in a case series through a radiological and histological evaluation after six months from the surgery [9]. Also, they advocated that Choukroun's PRF, which is a simple and inexpensive biomaterial in systematic use during a sinus lift seems as an acceptable option [10]. Bone Grafts perform osteoinduction followed by osteoconduction and osteoproliferation which is in accordance with Ellegaard et al., & Nielsen et al., Early publications and clinical experience indicate that PRF improves early wound closure, maturation of bone, and the final aesthetic result of the periodontal soft tissues. Production of a dense, cross-linked, physically robust PRF made of intact platelets and fibrin by high-speed centrifugation in the absence of exogenous thrombin, yields an ideal scaffold for use in tissue repair [11]. It requires around one year for complete healing to occur after the periapical surgery while with the use of PRF, healing is fastened and requires approx six months for complete regeneration of bone [12]. The application of autologous platelet-rich fibrin along with bone graft present new possibilities for enhanced healing and functional recovery. It could be more effective and economical than any other available regenerative materials.
Limitations of this Procedure
Only radiographic evaluation can be done, histological studies are required to examine the nature of newly formed tissue in the defect. Long-term, controlled clinical trials will be required to ensure its effective repair and regeneration [13]. Although PRF belongs to a new generation of platelet concentrates, the biologic activity of fibrin molecule is enough to account for significant cicatricial capacity of the PRF [14]. The slow polymerization mode confers to PRF membrane as a particularly favourable physiologic architecture to support the healing process [15]. The major drawback of its use is the risk of transmitted serological disease from pooled and single-donor blood donors. The safest preparations use the patient's own blood to prepare fibrin glue [16]. Tissue damage and vascular exposure result in platelet activation which secretes platelet-α-granules that is fused with Platelet cell membrane that transforms secretory protein into bioactive state proteins (PDGF, TGF-β, VEGF, EGF and IGF-1. These protein bind to transmembrane receptor of target cell which activates intracellular signaling proteins that results in expression of gene sequence directs cellular proliferation, collagen synthesis, and osteoid production [17]. The first surgical additives to be used were fibrin sealants which were commercially available in Europe since late 1970s. It was also known as fibrin glue or fibrin tissue adhesive [18]. The anterior iliac crest provides abundant cancellous bone & is ideal for condensing into bony defects, such as alveolar cleft and cystic cavities [18,19]. The application of autologous platelet-rich fibrin along with bone graft presents new possibilities for enhanced healing and functional recovery [20,21].
Conclusion
With the present case report it can be confirmed that PRF along with bone graft had presented regenerative benefits along with good functional recovery. It could be more effective and economical than any other available regenerative materials. Hence, being the choice of treatment economically, functionally with easy availability.
[1]. Schwartz Z, Somers A, Mellonig TJ, Carnes DL Jr, Dean DD, Cochran DL, Ability of commercial demineralized freeze-dried bone allograft to induce new bone formation is dependent on donor age but not genderJ Periodontol 1998 69:470-8. [Google Scholar]
[2]. Gassling VL, Açil Y, Springer IN, Hubert N, Wiltfang J, Platelet-rich plasma and platelet-rich fibrin in human cell cultureOral Surg Oral Med Oral Pathol Oral Radiol Endod 2009 108:48-55. [Google Scholar]
[3]. Ross R, Glomset J, Kariya B, Harker L, A platelet-dependent serum factor that stimulates the proliferation of arterial smooth muscle cells in vitroProc Natl Acad Sci U S A 1974 71:1207-10. [Google Scholar]
[4]. Gassling V, Douglas T, Warnke PH, Açil Y, Wiltfang J, Becker ST, Platelet-rich fibrin membranes as scaffolds for periosteal tissue engineeringClin Oral Implants Res 2010 21:543-49. [Google Scholar]
[5]. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolutionOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101:e37-44. [Google Scholar]
[6]. Saluja H, Dehane V, Mahindra U, platelet rich fibrin: A second generation platelet concentrate and new friend of oral and maxillofacial surgeonsAnn Maxillofac Surg 2011 1(1):53-7. [Google Scholar]
[7]. Carlson ER, Bone grafting the jaws in the 21 st century: The use of platelet-rich plasma and bone morphogenetic proteinAlpha Omegan 2000 93:26-30. [Google Scholar]
[8]. Garg AK, The use of platelet-rich plasma to enhance the success of bone grafts around dental implantsDental Implantol Update 2000 11:17-21. [Google Scholar]
[9]. Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR, Platelet-rich plasma: Growth factor enhancement for bone graftsOral Surg Oral Med Oral Pathol Oral Radiol Endod 1998 85:638-46. [Google Scholar]
[10]. Sunitha Raja V, Munirathnam Naidu E, Platelet-rich fibrin: Evolution of a second-generation platelet concentrateIndian J Dent Res 2008 19:42-6. [Google Scholar]
[11]. Nevins M, Giannobile WV, McGuire MK, Kao RT, Mellonig JT, Hinrichs JE, Platelet-derived growth factor stimulates bone fill and rate of attachment level gain: Results of a large multicenter randomized controlled trialJ Periodontal 2005 76:2205-15. [Google Scholar]
[12]. Nair PNR, New perspectives on radicular cysts: do they heal?International Endodontic Journal 1998 31(3):155-60. [Google Scholar]
[13]. Shear M, Radicular and residual cysts. in Cysts of the Oral Region 1992 3rd editionBristol, UKWright:136-162. [Google Scholar]
[14]. Choukroun J, Diss A, Simonpieri A, Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healingOral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology 2006 101(3):E56-E60. [Google Scholar]
[15]. Naik B, Karunakar P, Jaidev M, Marshal Rahul V, Role of platelet rich fibrin in wound healing. A critical reviewJ Conserv Dent 2013 16(4):284-93. [Google Scholar]
[16]. Thompson DF, Letassy NA, Thompson GD, Fibrin glue. A review of its preparartion ,efficacy and adverse effects as a topical hemostatDrug Intell Clin Pharm 1988 22(12):946-52. [Google Scholar]
[17]. Brugnami F, Then PR, Moroi H, Leone CW, Histologic evaluation of human extraction sockets treated with demineralized freeze-dried bone allograft (DFDBA) and cell occlusive membraneJournal of Periodontology 1996 67(8):821-5. [Google Scholar]
[18]. Hoen MM, LaBounty GL, Strittmatter EJ, Conservative treatment of persistent periradicular lesions using aspiration and irrigationJournal of Endodontics 1990 16(4):182-6. [Google Scholar]
[19]. Danin J, Linder LE, Lundqvist G, Ohlsson L, Ramsköld LO, Strömberg T, Outcomes of periradicular surgery in cases with apical pathosis and untreated canalsOral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 1999 87(2):227-32. [Google Scholar]
[20]. Cohen J, Lacroix P, Bone and cartilage formation by periosteum, assay of experimental autogenous graftsJournal of Bone and Joint Surgery 1955 37(4):717-30. [Google Scholar]
[21]. Toffler M, Toscano N, Holtzclaw D, Corso MD, Dohan E, Hrenfest DM, Introducing Choukroun's platelet rich fibrin (PRF) to the reconstructive surgery milieuJ Implant Adv Clin Dent 2009 1:21-30. [Google Scholar]