Generally tooth extraction often results in alveolar ridge resorption or collapse. Insertion of implants at the time of extraction might contribute to alveolar bone preservation [1]. The primary advantage of immediate implant placement is the reduction of the healing time and preservation of the bone tissue which generally occurs within the extraction site and around the implant [2,3]. This bone forming activity may enhance the bone-to-implant contact as compared with an implant placed in a less osteogenically active site. Early implantation could lead to favourable implant/crown ratio, better aesthetics and a favourable interarch relationship [4] and may preserve the alveolar anatomy, and the placement of a fixture in a fresh extraction socket helps to maintain the bony crest. The aims and objectives of this study were to placement of implants in freshly extracted sockets of anterior teeth and to evaluate the implant stability, peri-implant radiolucency and gingival inflammation around implant over a short period of 30 months.
Materials and Methods
A total of 12 patients (8 male and 4 female), form the outpatient Department of Periodontics faculty of Dental Sciences, Chhatrapati ShahuJi Maharaj Medical University Lucknow UP India, ranging in the age from 20 to 50 years, from March 2007 to June 2007, were evaluated for immediate implant placement into 22 fresh extraction sockets. Preoperative assessment of bone was done by intraoral periapical radiograph of selected site and orthopantomogram (OPG). Only maxillary and mandibular anterior teeth/roots (central incisors, lateral incisors and canines) were considered for replacement with implants. Immediate implants were placed only in those sites which are indicated for extraction [Table/Fig-1].
Figure shown preoperative view of implant site. Maxillary right central and left lateral incisors are candidate for implant placement in immediate extraction sockets

One piece implant with integrated abutment and integrated surface, non-submerged, threaded and tapered at apical 5 mm, sand-blasted and acid etched surfaced implants* were used. These are one stage screw type single implants, made of commercially pure titanium. The total length of the implants used was 20.5 mm and the diameters were ranging from 3.7 mm to 4.5 mm. Implant diameter was selected based on extraction socket diameter at the crest level. These implants were divided into 13 mm threaded portions, 2 mm collar and 5.5 mm trans-gingival inbuilt abutment. Implants were placed in immediate extraction sockets [Table/Fig-2] to observe their survival over a short period of 30 months [Table/Fig-3]. The following criteria were used to determine suitability for immediate implant placement at the time of extraction.
Figure shown immediate postoperative view after implant placement

Figure shown implants after three months postoperatively

Patients having anterior teeth with two or three degree mobility, root fracture/perforation, root stump (s)/residual root, non-restorable caries and failed root canal treatment, have been included for the study. It was ensured that all selected cases had sufficient bone (equal to or more than 3 mm) beyond the tooth socket apex. Those with uncontrolled diabetes, smoking, radiation therapy in orofacial region, drug/alcohol abuse, patients on steroid treatment and chemotherapy, acute illness, pregnancy, severe intermaxillary skeletal discrepancy, severe clenching and bruxism/any history of bruxism, sockets after traumatic extraction, old patients (geriatric patients), and patients with unrealistic expectations and psychological problems, were excluded from the study.
Radiographic assessments of peri-implant radiolucency were performed by postoperative Dentascan [Table/Fig-4,5] and Intraoral Periapical (IOPA) radiographs at subsequent visits.
Dentascan radiograph of implant in place after six months postoperatively
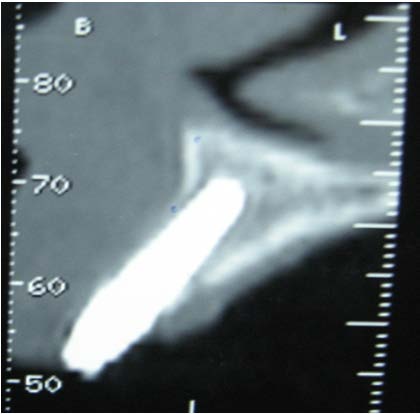
Dentascan radiograph of same implant after thirty months

Procedure
After case selection, medical and dental history of patient was recorded and written informed consent from all the patients was obtained before performing the procedure. The implants were placed immediately after atraumatic extraction of tooth/root. No incision and no flap [5] were performed. Access was gained through extraction socket. Bone drilling was performed with sharp instruments in progressively increasing diameters throughout the drilling process and with maximum use of bone apical to the extraction sockets. During bone drilling a finger was placed over the thin buccal mucosa, enabling close contact with the labial bony plate, thus preventing bone perforation. After removing debris from the socket a stepped 2.2 mm internal irrigation twist drill (XTD 2.2) was used to deepen the preparation beyond the apex of the socket first in the sequence and later on progressively increasing diameter of twist drills were used according to the length and diameter of implant to be placed. The twist drill was used at a speed of 800 to 1200 rpm with copious external and internal irrigation with normal saline. It was of great importance to drill gently, in a straight, precise, up and down motion with low pressure, low speed with sufficient internal irrigation, to avoid overheating and thus necrosis of alveolar bone.
The depth and angulation was checked continuously with the help of depth gauge paralleling pins which has depth markings of 8 to 14 mm. The markings corresponding with the selected implant length (threaded portion), had to disappear just below the alveolar crestal bone level. The socket was thoroughly irrigated with sterile saline solution. Before implant placement, a bone curette was used to palpate and reassure the integrity of the labial plate. The implant was then placed into the prepared socket with the implant mount with implant head parallel to the incisal edge of the adjacent tooth and implant was inclined palatally/lingually. When the implant was stable in the site, the mount (implant holder) was pulled out and the fixture insertion tool (XOT or TIT) was engaged to the implant and with the gentle pressure (40-55 Newton- cm) by hand or Hex ratched the implant was tightly screwed into the bone till the threaded portion of the implant disappears into the alveolar bone and collar of the implant came in alignment with the crest of alveolar bone. To ensure primary stability has been achieved, the implant should not rotate when a reverse torque less than 20N-cm is applied. The wrench must break in the reverse mode at this torque. The snug fitting of the implant was ensured to prevent any mobility. Implants were determined to be clinically stable by palpation and percussion. A distance of not less than 3 mm from the adjacent cementoenamel junction was maintained to achieve a normal emergence profile. After implant placement, the mucosa (buccal and lingual soft tissue edges) was adapted to the abutment and sutured with 3-0 black silk to enable maximal approximation [6]. It is essential for achieving full bone growth around the implant. Patients were then advised to follow postoperative instructions, which include soft high nutrient diet, postoperative medications which consisted of Amoxicillin 1.5 g/day for 5 to 7 days, Ibuprofen 600 mg three times a day for 3 days. Mouth wash, chlorhexidine gluconate (0.2%) twice a day for seven days was advised. The patients were then called for the subsequent postoperative follow ups. The sutures were removed seven days after the surgery. The patients were then called for follow-up postoperatively at 1st week, 4th week and 12th week, six month, twelve month, eighteen month and thirty month.
The stability of the implants was recorded at subsequent follow-up visits [Table/Fig-6]. The stability was determined by tactile perception and Fremitus test (the implant was held firmly between the handles of two metallic instruments or with one metallic instrument and one finger and an effort is made to it in all directions. Mobility of implants was graded as follows:
0 – Mobility absent in either direction.
1 – Mobility present in either direction.
Table showing mobility of implants at subsequent follow up visits.
| Duration (months) | Implant mobility | Total (no. of implants) |
|---|
| Absent (no. of implants) | Present (no. of implants) |
|---|
| 6 | 22 | 0 | 22 |
| 12 | 22 | 0 | 22 |
| 18 | 22 | 0 | 22 |
| 30 | 22 | 0 | 22 |
(χ2 =0.04544, df = 3)
Peri-implant radiolucency around implant at subsequent visits was observed and recorded on dentascan and intraoral peri-apical radiographs as follows:
0 – Radiolucency absent at any bone to implant contact site.
1 – Radiolucency present at any bone to implant contact site.
Gingival inflammation around implant was observed and recorded by noninvasive gingival index using Modified Gingival Index (MGI) Loben et al., [7].
A set of criteria for success was defined to evaluate the treatment outcome of the endosseous implants. Criteria for the success of the implants were adopted from the Buser et al., [8] as follows:
Criteria of Success
Absence of persistent subjective complaints, such as pain, foreign body sensation, and/or dysaesthesia.
Absence of a recurrent peri-implant infection with suppuration.
Absence of mobility.
Absence of a continuous radiolucency around the implant.
Statistical Analysis
Appropriate statistical analysis was performed using Chi-square test for qualitative data.
Results
The results were appropriately tabulate and interpreted along with description of one case with figures. The mobility was not present in any of the implants at all the follow up visits.
[Table/Fig-7] has show the peri-implant radiolucency at any bone to implant contact site at different time intervals. Peri-implant radiolucencies were found transient and considered as part of normal bone healing and remodeling. Severe gingival inflammation was not observed in any of the implant site. Mild to moderate gingival inflammation was found as a consequence of plaque accumulation at the gingival margin. Patients were then advised to perform meticulous oral hygiene preventive procedures.
Table showing peri-implant radiolucency at any bone to implant contact site.
| Duration (months) | Peri-implant radiolucency | Total (no. of implants) |
|---|
| Absent (no. of implants) | Present (no. of implants) |
|---|
| 6 | 20.00 | 2.00 | 22.00 |
| 12 | 21.00 | 1.00 | 22.00 |
| 18 | 21.00 | 1.00 | 22.00 |
| 30 | 22.00 | 0.00 | 22.00 |
(χ2 = 3.33, df = 3, p>0.10 at 10% level of significance)
At every follow-up visit, every implant met the criteria of success and none was found to be failed over a 30 months duration i.e. 100% success rate was achieved by implants in immediate extraction socket.
Discussion
Missing teeth and supporting oral tissues have traditionally been replaced with dentures and bridges permitting restoration of functions such as chewing, speech and aesthetics. Branemark et al., introduced the concept of osseo-integration and since then it became possible to achieve successful placement of implants in edentulous and partially edentulous patients [9]. The initial long term retrospective studied yielded the concept that the root form dental implants and osseo-integration into supporting bone could be used to replace teeth in edentulous and partially edentulous patients.
It has been a common experience that patients with recent tooth extraction are hesitant to have their adjacent teeth grinded for purpose of making fixed partial denture. Also after loss of teeth, loss of bone occurs both in width and height, resulting into various functional and aesthetic complications. It has been observed that immediate placement of implants into fresh extraction sockets has the advantage of decreasing healing time, reducing resorption of alveolar bone (preservation of bone tissue) and achieving optimal aesthetics. These were the main reasons to replace diseased and nonrestorable teeth with immediate implants. Furthermore, immediate implants also fulfilled the patient’s desire in terms of earlier restoration of functions and aesthetics without any psychological trauma. The high success rate of dental implants has change the quality of life for many patients. Histological, it was confirmed that immediately loaded implants placed in soft spongy bone after healing can present mineralized tissue at the interface by Degidi M et al., [10].
The aims and objectives of this study were to place implants in freshly extracted sockets of anterior teeth and to evaluate the implant stability, peri-implant radiolucency and gingival inflammation around implant over a short period of 30 months. In this study, some of the defined criteria for implant success were in common to which were applied universally to any dental implant patient, whereas others were modified accordingly. Outcomes such as the absence of persistent infection, neurologic signs and symptoms, implant mobility, peri-implant radiolucency, and the absence of gingival inflammation were the fundamental objectives of implant treatment.
The questions of how to define implant success and how to perform uniform analysis of long-term results remain the subject of controversy [11,12]. According to Naert et al., an implant must be free of inflammation and clinically firm [13], whereas according to the criteria proposed by Jahn and d’Hoedt [12], additional parameters are also considered. Stability of implants and absence of mobility in all the cases at 6th, 12th, 18th and 30th month of recall visits after placement of the implants was in confirmation with the results found by Backer et al., [14]. The results of this study also fulfiled the Albrektsson et al., [15], criteria for implant success.
Albrektsson T and Pillar et al., suggested that there must be an absence of movement or limited micromovement between an implant and bone, for osseo-integration to occur [16,17]. Excessive micromotion results in scar type fibrous healing owing to scaffold disruption by Brunski JB [18].
In the present study, there was no evidence of consistent peri-implant radiolucency in any case at 6st month, 12th month 18th month and 30th month after implant placement. The peri-implant radiolucency at some focal sites at bone to implant contact sites was noticed around two implants at 6th month, one implant at 12th month and one implant at 18th month of follow-up visits. It has observed that this focal peri-implant radiolucency at implant to bone contact point was appeared and disappeared at different time intervals and not even a single implant carried it forward to the subsequent follow-up visits. It means that the focal peri-implant radiolucency that was present around one implant at 6th month was not observed at further subsequent visits. It was proposed that this focal peri-implant radiolucency might be a part of normal bone remodeling process and not pathological. These observations were matched with the observations of Mauricio G et al., who studied ridge alteration following implant placement in fresh extraction sockets and observed that the placement of an implant in the fresh extraction sites obviously failed to prevent the remodeling that occurred in the walls of the socket [19]. He also suggested that the resorption of the socket walls following tooth removal must be considered in conjunction with implant placement in fresh extraction sockets.
D E Smith et al., proposed that there should be no peri-implant radiolucency on undistorted radiograph for success of implant [20]. The results of this study are comparable with this study.
Dentascan was done in all the cases for assessment of peri-implant radiolucency on different surfaces of implants. It has been observed that dentascan provides an outstanding view of jaws with or without implants and it has a better edge enhancement for the assessment of bone changes and peri-implant radiolucency. Yeung KM A et al., observed that dentascan is not only used for pre-implant assessment but also in the diagnosis of lesions affecting the jaw [21]. Mupparapa M et al., observed that the dentascan usually provides a complete and comprehensive report commenting on the bone density, general health of the maxilla and the mandible, status of the dentition and measurements pertaining to the alveolar process [22]. Three-dimensional reconstruction images are available with most Dentascan protocols Wyatt CC, Pharoah M [23]. It is the most permanent and the most reliable technique in the peri-implant evaluation. It allows a precise anatomical study without any distortion. It positions anatomical obstacles (nasal cavities, sinus, mandibular canal), and allows a lifesize morphological study of the jaw, available bone height, labio-lingual thickness, and jaw obliquity.
Esposito M et al., and Dover MS considered the act of probing the peri-implant gingiva as an invasive procedure that disturbed the soft tissue cuff around the implant, so that bleeding on probing might reflect an injury of the tissues caused by undue force on using a periodontal explorer [24,25]. For this reason, in this study, assessment of peri-implant gingival tissue was done by Modified Gingival Index (MGI) Loben et al., which is noninvasive gingival index [7].
The status of peri-implant gingival tissue of the 22 implants was considered satisfactory [Table/Fig-8] and compatible with the findings reported in other studies [15,26]. The maintenance of the peri-implant hygiene by the patients was facilitated, as these patients were able to maintain a reasonable hygiene standard, as almost all the implants were free from severe inflammation. This may illustrate the importance of regular recalls and motivation of these patients. Although, the gingival tissues around the implants were characterized by mild inflammation but it did not hinder maintenance of gingival health.
Table showing severity of gingival inflammation around implant at subsequent follow-up visits.
| Duration (months) | Gingival inflammation | Total (no. of implants) |
|---|
| Mild (no. of implants) | Moderate (no. of implants) | Severe (no. of implants) |
|---|
| 6 | 20.00 | 2.00 | 0.00 | 22.00 |
| 12 | 19.00 | 3.00 | 0.00 | 22.00 |
| 18 | 19.00 | 3.00 | 0.00 | 22.00 |
| 30 | 20.00 | 2.00 | 0.00 | 22.00 |
(χ2 = 0.9026, df = 3)
The implant loading was done after three months in all the cases and it was observed at every recall visits that there was no change in stability, and peri-implant radiolucency. At the day of loading there was slight discomfort in the gingival tissue which was subsided after three days. The success rate of implant survival in this study was found 100% [Table/Fig-9]. These implants have fulfilled all the criteria of implant success and based on the defined criteria, the success rate of implants placed in immediate extraction sockets of anterior teeth compared favourably with the conventional implants.
Table showing Implant success rate at different time interval
| Implant success rate | Duration of subsequent follow-up visits |
|---|
| 6 month (%) | 12 month (%) | 18 month (%) | 30 month (%) |
|---|
| Success | 100.00 | 100.00 | 100.00 | 100.00 |
| Failure | 0.00 | 0.00 | 0.00 | 0.00 |
Conclusion
The early results of the present study showed that high survival rates with the implants in immediate extraction sockets can be achieved. The minimal surgery used in this study enabled slight postoperative discomfort, and uneventful healing. The complications were mild and statistically non-significant. All implants were immobile and asymptomatic and no implant was failed and lost. This study confirmed that endosseous implants could be successfully placed in immediate extraction sockets of anterior teeth.
(χ2 = 3.33, df = 3, p>0.10 at 10% level of significance)
(χ2 = 0.9026, df = 3)