Introduction
Surgical wounds heal by primary intention in all the elective and emergency surgical procedures. Current practice is to place dressing over the closed wound before the patient leaves the sterile environment of the operating theatre. The aim of the dressing is to prevent wound infection. It had been and is the practice in most of the hospitals to repeatedly dress surgical wound until stitches are removed. This practice assumes that the risk of Surgical Site Infections (SSIs) is reduced by providing a barrier to environmental contamination. Moreover, dressing’s helps to manage wound exudates, protects wounds and their staples or sutures, and decreases patients’ anxiety by 'hiding' the wound.
Methods of dressing ranges from the wound being completely covered by adhesive plaster to sterile gauze. Dressing is a material applied to protect a wound and it favours wound healing. However, to leave wound open in direct contact to environment following any procedure by just applying some ointment on it, the so called open wound treatment is still controversial one.
Although studies in the past have demonstrated the safety of exposure of surgical wounds [1,2], but there are studies which didn’t support this practice [3-5]. It is still common practice to dress wounds postoperatively, a procedure which involves expense in both materials and nursing time. Hence, it is important to assess whether wound dressings have a potential role in reducing the risk of SSI. Such information can inform allocation of resources to appropriate treatments. In the present study we have compared open wound treatment vs occlusive dressings in elective surgical cases with respect to surgical site infections in 100 patients admitted for elective surgery.
Materials and Methods
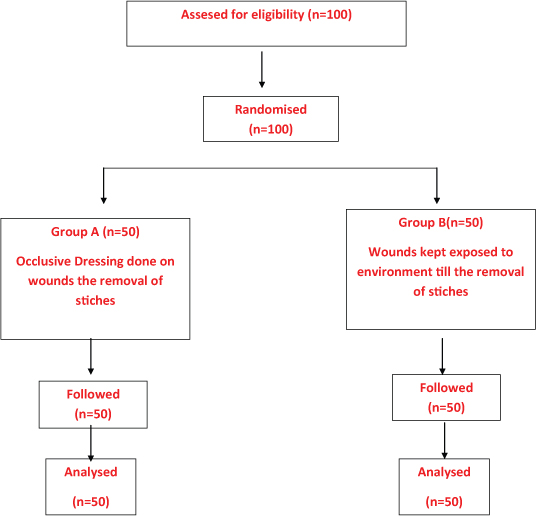
The present study was conducted on 100 patients admitted for elective general surgery in surgical wards of Guru Gobind Singh medical college and hospital, from April 2010 to April 2011, over a period of one year, after taking written informed consent. The minimum sample size for the present study was calculated using 11.1% as infection rate after referring the study by A Asnake. The sample size was calculated in such a manner to maintain a power of 67%, assuming atleast 90% reduction in the infection rate in the exposed group and with 5% level of significance i.e. type-I error. It was calculated to be 50 cases in each group. Therefore, the total sample size was 100.9 [Table/Fig-1]. Patients were divided randomly into two equal groups each comprising of 50 patients using computer generated random list. In group A, patients had occlusive dressing till removal of stitches and in group B, patients wounds were kept exposed to environment after the surgical procedure. However, the drain sites were covered with sterile gauze dressing.
Patients having age <10 years or >65 years, with history of systemic diseases like diabetes, anaemia, coagulopathy, hypoprotenemia or patients who were Immunocompromised due to malignancy, Acquired Immunodefficiency disease, patients on steroids or having burn wounds or drain sites with excessive drainage were excluded from the study.
In all the cases detailed history, general physical examination and local examination was done and type of procedure performed were recorded. Classification of surgical wound contamination was done based on the nature of surgical procedure (Clean, Clean Contaminated, Contaminated, Dirty). Surgical site swab from the site of supposed incision was taken just before preoperative preparation of the patient and sent for culture and sensitivity. Hairs at the incision site were removed only when their presence interfered with intended procedure. After taking swab, preparation of the operative area was done with povidine iodine solution. Umbilicus was cleaned separately in cases of abdomen. Administration of prophylactic 1g intravenous injection of ceftriaxone was given just prior to incision in every case and was repeated after 6 hours of the surgical procedure. During the surgical procedures, stress was given on minimal and gentle tissue handling, a good haemostasis, obliteration of all dead spaces and all aseptic precautions. All skin wounds were closed with silk. After closure of the wound length of incision was measured and duration of operation was recorded.
In group A patients, the wound was completely covered by sterile gauze and that was held by a few tape strips and this was done till removal of stitches. However, in group B patients, wound was kept exposed to the environment after the procedure, but the drain sites were covered with sterile gauze. Dressing in case of group A was done with sterile gauze after cleaning the wound with 5% povidine iodine and changed when required. However in group B, 5% povidine iodine solution was applied on the wound daily.
All the patients were observed in ward daily and discharged with healthy wounds on ambulatory conditions with advice to come after one week or if there was any sign of surgical site infection like persistent local pain, tenderness, hyperemia, discharge, seroma, bleeding, abscess formation etc at the surgical site. During the course of follow up, culture swab was taken and was sent for culture and sensitivity when there was any sign of infection. Antibiotics were given as per need and depending upon culture and sensitivity. Stitches were removed on the 8th postoperative day, if the wounds remained healthy and clean. Severity of infection was graded according to Burton’s Criteria [6]. Further follow up was taken after one week, two weeks, four weeks, or whenever required to see any delayed complications.
Results
The present study was undertaken to compare open wound treatment vs occlusive dressings in elective surgical cases with respect to surgical site infections. In the present study mean age of patients in years was 39.98±13.63 in group A and 40.56±14.2 in group B. [Table/Fig-2] shows the age in years, sex distribution, and distribution of clean and contaminated wounds, duration of surgery and length of incision in both the groups. In the present study, overall rate of SSI was 7%. However, group wise incidence of SSI is shown in [Table/Fig-3]. Mean duration of all the operative procedures performed in the study was 47 minutes. However, group wise duration of all the operative procedures and its link with SSI is shown in [Table/Fig-4].[Table/Fig-5] shows the relation of length of incision and its link with SSI. [Table/Fig-6] shows SSI linked to postoperative stay. In all the 100 patients observed in this study, the mean postoperative stay was 4.57 days. Mean postoperative stay in Group A was 4.76 days with standard deviation of 2.925 and mean postoperative stay in Group B was 4.38 days with standard deviation of 2.934. The statistical difference, in mean postoperative stay (days) in both groups was not significant (p-value=.518.) [Table/Fig-2].
Discussion
Although the wound healing is topic of research since ages but it is still a mystery as highlighted by the famous saying by Ambroise Paré "I dressed the wound. God healed it" [7].
Historically, a dressing usually consisted of a piece of material, sometimes cloth, but the cowdung, honey and leaves have been used. However, modern dressings include gauzes, films, gels, foams, hydrocolloids, hydrogels and polysaccharide pastes, granules and beads. Dressings can be impregnated with antiseptic chemicals to prevent infections.
In the present study we have compared open wound treatment vs occlusive dressings in elective surgical cases with respect to surgical site infections. All wounds were divided in to Clean and Clean Contaminated types on the basis of a widely used definition describing the contamination classification of surgical procedures [8].
The infection rates noted in this study are comparable to the previous studies. Infection rates in the four surgical classifications (Clean, Clean-Contaminated, Contaminated and Dirty wounds) have been studied extensively but the work of Cruse and Foord is a usually held a standard for infection rates [9-10]. Standard infection rates in their study were 1-2% or less for Clean wounds, 6-9% for Clean-Contaminated wounds, 13-20% for Contaminated wounds and about 40% for Dirty wounds. Difference in each class is due to type of surgery being performed [11].
Law and Ellis in their study on non contaminated elective surgical cases, found postoperative 5.42% infection rate in overall cases of their study and they noticed 7.07% wound infection rate in patients on whom dressings were done whereas in the patients whose wounds were exposed, infection rate was 1.88% [1]. Similarly in another study on clean and clean contaminated elective surgical wounds, found 10.8% infection rate in all cases he studied. He reported 13.09% infection rate in patients whom dressings were done and 8.69% infection rate in patients who had their wound exposed [2]. In present study we observed total 7% of postoperative wounds were infected of all the clean and clean contaminated wounds we studied. In Group A, patients had occlusive dressing and these patients had 8% infection rate whereas in Group B patients, wounds were kept exposed to environment and these patients had 6% infection rate. A meta-analysis also showed no difference in surgical-site infection rates between surgical wounds covered with different dressings and those left uncovered [12].
Moreover dressings may also increase hypoxia to the wounds and dressed wounds have shown decreased tensile strength when compared to undressed wounds [13].
These results indicated that healing was not impaired by exposure of 'Clean and Clean Contaminated ' postoperative wounds. This might be because the wounds developed a coagulum made up of blood and fibrin which did not allow the inoculated organisms to go deeper. In dressed wound, however, moist environment may delay coagulum formation and can allow organism to penetrate into wounds [1].
Mean duration of operative procedures in the present study was 47 minutes. The procedures which took longer time had more infection rates with maximum in procedures that took >60 minutes (22.22%) and no infection was found in any patient on whom the operative procedure took less than 30 minutes [Table/Fig-4]. Even if we compare our two Groups of our study, procedures that took >60 minutes in both Groups had higher infection rates. The infection rates in these procedures were 25% and 20% respectively in both the Groups.
In the present study, the increased rate of infections in the procedures who took longer time is supported by many studies. It has been seen that the rate of wound infection increased for longer procedures, roughly doubling with every hour of the procedure [9,10]. The factors responsible for increase in infection during surgery having longer duration could be exposure of the wound to operation theatre environment for longer period, prolonged retraction and increased manipulation resulting in local devitalization of tissues that becomes more favourable for infection. Moreover there are increased chances of systemic insult by increased blood loss, which may cause diminished general resistance to infection.
Mean length of incision in this study was 6.58±3.342 cm in group A and 6.26±2.46 cm in Group B [Table/Fig-2]. Maximum rate of infection was found in incisions >10 cm (16.67%) and no infection were seen in incisions up to 5 cm [Table/Fig-5]. Incisions which were between 6-10 cm had infection rate of 10.71%. The cause of more infection rate in lengthier incisions of present study may be due to more tissue injury and greater area for contamination and increased chances of systemic insult because of more blood loss [9,10].
In the present study, postoperative hospital stay was prolonged in infected cases [Table/Fig-6]. There were only four patients in whom the postoperative stay exceeded than 10 days out of which three were infected cases. One patient remained admitted due to his respiratory disorders. In these three infected cases two belonged to Group A and 1 belonged to Group B. This is a well known fact that patient with surgical site infection have longer hospital stay and require more nursing care and readmission [14].
The most useful point noticed in the present study was that the wounds that were left open could easily and anytime be examined by the surgeon, leading to earlier detection of signs of infection in them. That gave these wounds an extra advantage to their counterparts which were dressed.
NW Law and H Ellis reported that the total dressing costs for the basic wound contact-dressed group were GBP (Great Britain Pound) 6.60 compared to GBP 0.80 in the exposed group [1]. In the present study, expenditure of single basic dressing was about 25 INR and it took about 10 minutes in each time to do a dressing of the patient. On an average 5 times dressings were changed in the patients in Group A. So if we take this in account, in all the 50 patients of Group A, total cost of dressings was 6250 INR and total time consumed was 41.67 hours till removal of stitches. On the other hand, expenditure of application of daily 5% povidine iodine solution only and then leaving the wound open was about 3 INR and it took about one minute in each time to apply the 5% povidine iodine solution. So, considering this amount of expenditure and time to treat the wound till removal of stitches in all the 50 patients of Group B, the total expenditure was 1200 INR and total time consumed was 6.67 hours.
So in the present study, had all the wounds been left open, about 4050 INR and 35 hours could have been saved. Moreover, this present study tells us about only the 100 patients and there are thousands of elective surgeries being done across the whole nation, thus we can very well imagine the amount of extra burden we are carrying both in terms of the money and time. Thus simply by changing one practice of treating the postoperative wounds, from dressing to leaving them open and exposed to air, millions of rupees and a lot of time can be saved that may be used for some other purpose. Moreover keeping the wound undressed also saves time of nursing.
On the basis of these observations, present study clearly indicates that there is no harm in leaving the elective surgical wounds open and exposed to the air after application of 5% povidine iodine on them, as treating these wounds by this method does not increase the rate of infections rather, it is economically better than to dress them. One more factor which highlights the importance of leaving the wound open is that examination of the wound by the surgeon is very easy in this method leading to earlier detection of signs of infection and other complications with a chance to arrest them at lower stage only. However being a small group monocentric study is the major limitation of study. As wound healing is effected by multiple factors like general health or nutritional status of patient, obesity, age, comorbid conditions and local factors like site of surgery, type of health center and type of caregiver so a large group polycentric study is needed to confirm the results of present study.
Participant flow chart for the study
Shows the age in years, sex distribution, distribution of clean and contaminated wounds, duration of surgery, length of incision and mean postoperative stay (in days) in Group A & B
| Group A | Group B | p-value |
|---|
| N= 50 | N= 50 |
|---|
| Age in years | 39.98±13.63 | 40.56±14.2 | 0.834 |
| Sex (Male/Female) | 28/22 | 23/27 | 0.317 |
| Clean/clean contaminated wounds | 32/18 | 22/28 | 0.045 |
| Duration of surgery (in minutes) | 46.20±16.523 | 47.20±14.63 | 0.834 |
| Length of incision (in centimeters) | 6.58±3.342 | 6.26±2.46 | 0.585 |
| Mean postoperative stay (in days) | 4.76±2.925 | 4.38±2.934 | 0.518 |
p-value <0.05 – significant (S), > 0.05 – Non significant (NS)
Showing incidence of surgical site infection
| Surgical contamination | No. of cases | No. of infected cases | %age | p-value |
|---|
| A | B | A | B | A | B |
|---|
| Clean | 32 | 22 | 2 | _ | 6.25 | _ | 0.154 |
| Clean Contaminated | 18 | 28 | 2 | 3 | 11.11% | 10.71% | 0.695 |
| Contaminated | _ | _ | _ | _ | _ | _ |
| Dirty | _ | _ | _ | _ | _ | _ |
| Total | 50 | 50 | 4 | 3 | 8 | 6 |
p-value > 0.05 – Non significant (NS)
Incidence of SSI related with duration of procedure
| Duration of procedure(minutes) | No. of cases | No. of infected cases | %age |
|---|
| A | B | A | B | A | B |
|---|
| Up to 30 | 10 | 7 | _ | _ | _ | _ |
| 31-60 | 32 | 33 | 2 | 1 | 6.25% | 3.03% |
| >60 | 8 | 10 | 2 | 2 | 25% | 20% |
| Total | 50 | 50 | 4 | 3 | 8% | 6% |
Incidence of SSI related to length of incision of procedure done
| Length of incision (cm) | No. of cases | No. of infected cases | %age |
|---|
| A | B | Total | A | B | Total | A | B | Total |
|---|
| Up to 5 | 18 | 20 | 38 | _ | _ | _ | _ | _ | _ |
| 5-10 | 27 | 29 | 56 | 3 | 3 | 6 | 11.11% | 10.34% | 10.71% |
| >10 | 5 | 1 | 6 | 1 | _ | 1 | 20% | _ | 16.67% |
| Total | 50 | 50 | 100 | 4 | 3 | 7 | 8% | 6% | |
Incidence of SSI related to postoperative stay
| Post-operative stay (Days) | No. of cases | No. of infected cases | %age |
|---|
| A | B | A | B | A | B |
|---|
| Up to 5 | 33 | 37 | _ | _ | _ | _ |
| 5-10 | 15 | 11 | 2 | 2 | 13.33% | 18.18% |
| >10 | 2 | 2 | 2 | 1 | 100% | 50% |
| Total | 50 | 50 | 4 | 3 | 8% | 6% |
Conclusion
It is hereby concluded that in the elective surgical cases there is no harm in leaving the wounds open postoperatively. These wounds can be better managed by leaving the wound exposed to air by application of 5% povidine iodine solution daily on them. This method not only helps in arresting the infective pathology at a lesser stage but also saves surgeon’s time and patient’s money.
p-value <0.05 – significant (S), > 0.05 – Non significant (NS)
p-value > 0.05 – Non significant (NS)
[1]. NW Law, H Ellis, Exposure of the wound: Safe economy in the NHSPostgrad Med J 1987 63:27-28. [Google Scholar]
[2]. A Asnake, A comparison of exposed with closed method of management of clean abdominal surgical woundsECAJS 2001 6(2):21-24. [Google Scholar]
[3]. O Katakura, N Morimoto, Y Iwasaki, K Akiyoshi, S Kasugai, Evaluation of 2-methacryloyloxyethyl phosphorylcholine (MPC) polymer-coated dressing on surgical woundsJ Med Dent Sci 2005 52(2):115-21. [Google Scholar]
[4]. OM Alvarez, PM Mertz, WH Eaglstein, The effect of occlusive dressings on collagen synthesis and re-epithelialization in superficial woundsJ Surg Res 1983 35:142-48. [Google Scholar]
[5]. D Demetriades, G Psaras, Occlusive versus semi-open dressings in the management of skin graft donor sitesSA fr Surg 1992 30(2):40-41. [Google Scholar]
[6]. RC Burton, Postoperative wound infection in colonic and rectal surgeryBr J Surg 1973 60(5):363-65. [Google Scholar]
[7]. AK Deodhar, RE Rana, Surgical physiology of wound healing: a reviewJ Postgrad Med 1997 43(2):52-56. [Google Scholar]
[8]. LM Mioton, SW Jordan, PJ Hanwright, KY Bilimoria, JY Kim, The Relationship between Preoperative Wound Classification and Postoperative Infection: A Multi- Institutional Analysis of 15,289 PatientsArch Plast Surg 2013 40(5):522-29. [Google Scholar]
[9]. PJ Cruse, R Foord, A five-year prospective study of 23,649 surgical woundsArch Surg 1973 107:206-10. [Google Scholar]
[10]. PJ Cruse, R Foord, The epidemiology of wound infection: a 10-year prospective study of 62,939 woundsSurg Clin North Am. 1980 60:27-40. [Google Scholar]
[11]. EM Ferraz, TS Bacelar, JL Aguiar, AA Ferraz, G Pagnossin, JE Batista, Wound infection rates in clean surgery: a potentially misleading risk classificationInfect Control Hosp Epidemiol 1992 13(8):457-52. [Google Scholar]
[12]. CJ Walter, JC Dumville, CA Sharp, T Page, Systematic review and meta-analysis of wound dressings in the prevention of surgical-site infections in surgical wounds healing by primary intentionBr J Surg 2012 99:1185-94. [Google Scholar]
[13]. A Quirinia, A Viidik, The influence of dressing on the healing of normal and ischaemic wounds and flap survivalScand J Plast reconstruct Surg Hand Surg 2001 35:1-6. [Google Scholar]
[14]. SA McGarry, JJ Engemann, K Schmader, DJ Sexton, KS Kayen, Surgical-site infection due to Staphylococcus aureus among elderly patients: mortality, duration of hospitalization, and costInfect Control Hosp Epidemiol 2004 25:461-7.doi: 10.1086/502422 [Google Scholar]