Introduction
It has long been recognized that vitamin D is a hormone and were many studies reporting that patients in periodontal maintenance programs taking vitamin D and calcium supplementation had a trend for better periodontal health compared to patients not taking supplementation.
Aim
To evaluate the effect of vitamin D and calcium supplementation in reducing gingival inflammation, using clinical parameters like gingival index (GI), oral hygiene index-simplified (OHIS), probing pocket depth (PPD), clinical attachment level (CAL) and bone density (BD). Also, to assess whether calcium and vitamin D oral supplementation influences alveolar Bone Density (BD).
Design and Settings
A nonrandomised clinical trial done in Amrita School of dentistry, Kochi, India.
Materials and Methods
Group A taking vitamin D (250IU/day) and calcium (500 mg/day) supplementation, and Group B were not taking oral supplementation. All subjects had at least one or more teeth with chronic moderate periodontitis. Digital Orthopantomogram images were taken to assess bone density. Data were collected at baseline and three months.
Statistical Analysis used
OHI-S, GI, PPD, CAL, and Bone Densities (BD) were calculated per group. Karl Pearson Coefficient of correlation was used to test correlation of bone density with GI and OHI -S. Intergroup comparison of parameters were done using Independent two Sample t-test. Intragroup comparison of parameters at recall interval was done using Paired sample t-test. The results were considered statistically significant when p-value was <0.05.
Results
Both Groups showed significant change in the periodontal parameters and bone density after three months and intragroup comparison showed highly significant results for vitamin D group in relation to GI, OHI S and bone density.
Conclusion
Calcium and vitamin D supplementation has got a positive effect on periodontal health and it can be used as an adjunct to non surgical periodontal therapy.
Introduction
Periodontitis is an inflammatory disease of the supporting tissues of the teeth caused by group of specific microorganisms, resulting in progressive destruction of periodontal ligament and alveolar bone loss with increased pocket depth, recession, or both [1,2].
Vitamin D is secosteroid hormone thought to be potentially influencing risk of periodontal disease through three mechanisms: maintenance of oral bone health, anti inflammatory activity and anti microbial activity. It is essential for consumption of calcium from the gut and re-absroption of calcium from kidneys and bone formation in order to maintain adequate plasma calcium concentrations for calcium homeostasis, bone mineralisation [3,4] and immunity [5]. There is biologic surmise that multiple actions of vitamin D are potentially appealing for the management of chronic periodontitis, whose pathogenesis is based on bacterial driven inflammation. It is speculated that status of vitamin D could modify the risk of perioodontitis [6] by preventing alveolar bone loss [7] or by mediation of host’s immune response to infection. Thus, there is evidence pointing to the potential role of calcium and vitamin D intake on dental health; however, there are controversies regarding the role of calcium and vitamin D supplementation in chronic periodontitis and its management. Definition regarding the use of optimum levels of vitamin D for maintenance of bone health has been a matter of debate [8].
Vitamin D synthesis in body is influenced by various factors like environmental (pollution, location), local factors (duration and time of exposure in sunlight, diet, job) and genetic factors. Even though a majority of Indian population inhabit in places receiving ample sunlight all year long, vitamin D deficiency is quite common in age groups even now in India [9,10]. The Indian Council of Medical Research (ICMR) recommends daily intake of 600 mg of calcium in adults and 800 mg of calcium in post menopausal age group. Yet the typical Indian diet fails [11,12] to ensure even 10% of daily vitamin D requirement and continues to recommend 400 IU per day of oral vitamin D [9,13–15]. Hence, the present study was designed to find any influence of calcium and vitamin D supplementation in periodontitis treatment outcome in otherwise healthy subjects whose serum calcium and vitamin D levels are in normal range. Primary objective of the study was to evaluate the effect of vitamin D and calcium supplementation in management of periodontitis. Secondary objective was to assess whether calcium and vitamin D oral supplementation influences alveolar bone density.
Materials and Methods
The study was conducted for a period of one year in the Department of Periodontics, Amrita School of Dentistry, Kochi,India from November 2012 and De-cember 2013.
The ideal sample size to ensure adequate power for this study was calculated based on the results from the study conducted by Miley et al., [16].
Inclusion Criteria
Age group ≥35 and ≤55 years, ≥ 20 number of natural teeth.
One or more teeth with chronic moderate periodontitis, attachment loss of 3-4mm.
Bone loss in the mandibular molar (except third molars) with mandibular furcation area with at least 1x1mm square area were selected in OPG as standard reference points for density analysis.
Exclusion criteria
Periodontal therapy within the past 6 months.
History of any systemic diseases.
Subjects with behavioural eating disorders.
History of antibiotic therapy in last six months.
Continuous exposure to direct sunlight for more than three hours a day.
Intake of any other nutrient supplements.
Subjects filled out a personalised questionnaire about food, job and duration of direct exposure to sunlight per day. So if the patient is taking any other nutrient supplement were excluded from the study. No special instructions were given about diet. A written informed consent was obtained from subjects.
Study design
In this non randomised clinical trial, 82 subjects were assessed, 40 were allocated into Group A, subjects who received full mouth oral prophylaxis, subgingival scaling, root planing and curettage along with calcium and vitamin D sup-plementation (Shelcal-D 500 mg calcium+250 IU vitamin D once daily) for three months and 42 in Group B, subjects who received full mouth oral prophylaxis, subgingival scaling, root planing and curettage. Four subjects from Group A and one subject from Group B were lost during follow up. Finally, there were 36 subjects in Group A and 41 subjects in Group B. SRP and curettage was done to reduce inflammation and standardize both groups.
We decided to give a minimum dosage of calcium and vitamin D supplementation for a shorter time period as per physician’s consultation. Recent study by Hiremath [17] et al., had specified in his study that a lower dosage of vitamin D will take atleast three months to be present in the serum.According to Marwaha [18] et al., and Malhotra [19] et al., Vitamin D requirement of 60,000-120,000 IU per month to achieve Vitamin D level > 30 ng/ml, level at which calcium absorption from the gut is maximum. Serum calcium and vitamin D recorded just to make sure that it was within normal limits. Three ml blood was drawn from participants and serum vitamin D level checked with direct Elisa kit (Immunotek; Bensheim, Germany) and serum calcium using Calcium detection kit (Abcam) in Amrita laboratory, AIMS, Kochi, India.
Periodontal examination at baseline involved recording clinical parameters like Oral Hygiene Index – Simplified (OHI-S) [20], Gingival Index (GI) [21], Probing Pocket Depth (PPD) and Clinical Attachment Level (CAL). Probing Pocket Depth and Clinical Attachment Level were measured using University of Michigan “O” probe with Williams’ markings at six sites per tooth (mesio-buccal/labial, mid-buccal/labial, disto-buccal/labial, mesio-lingual/palatal, mid-lingual/palatal, disto-lingual/palatal) at all teeth, excluding third molars, using a customized acrylic stent.
Subjects in the Group A were given special instructions to have more than two litres of water daily since they were taking oral supplement with calcium and vitamin D to prevent possible side effects like precipitation of calcium in the urine, gall bladder or kidney and manifested as colic pain. Bone density was recorded using software named SIDEXIS [22] in the digital OPG machine for both groups at baseline as well as at the end of three months.
Statistical Analysis
OHI-S, GI, PPD, CAL, and Bone Densities (BD) were calculated per group. Karl Pearson Coefficient of correlation was used to test correlation of bone density with GI and OHI -S. Intergroup comparison of parameters were done using Independent two Sample t-test. Intragroup comparison of parameters was done using Paired sample t-test. The results were considered statistically significant when p-value was <0.05.
Results
Baseline Comparison given in [Table/Fig-1].
Intergroup comparison of parameters at baseline
| Variable | Group A (36) | Group B (41) | p-value |
|---|
| GI | Baseline | 2.08 ± 0.37 | 2.05 ± 0.44 | 0.707 |
| OHI-S | Baseline | 4.01±0.20 | 3.74±0.26 | 0.001* |
| PPD(mm) | Baseline | 6.26 ±0.45 | 5.93 ± 0.39 | 0.001* |
| CAL(mm) | Baseline | 6.29 ± 0.74 | 5.94 ± 0.39 | 0.016* |
| BD(%) | Baseline | 40.75± 4.08 | 41.37± 2.98 | 0.458 |
*indicates significant p-value
Post intervention comparison of parameters
The intragroup comparison of clinical parameters in Group A [Table/Fig-2] and group B [Table/Fig-3] showed that there was statistically significant difference after three months.
Intragroup comparison of parameters of Group A
| Variable | Group A (36) | p-value |
|---|
| Baseline | 3 months |
|---|
| GI | 2.08 ± 0.37 | 0.33 ± 0.39 | 0.001* |
|---|
| OHI-S | 4.01±0.20 | 0.79 ±0.37 | 0.001* |
| PPD (mm) | 6.26 ±0.45 | 4.25 ± 0.31 | 0.001* |
| CAL (mm) | 6.29 ± 0.74 | 4.45 ± 0.64 | 0.001* |
| BD (%) | 40.75± 4.08 | 49.33 ± 4.72 | 0.001* |
*indicates significant p-value
Intragroup comparison of parameters of Group B
| Variable | Group B(41) | p-value |
|---|
| Baseline | 3 months |
|---|
| GI | 2.05 ± 0.44 | 1.09± 0.15 | 0.001* |
| OHI-S | 3.74±0.26 | 2.25 ±0.28 | 0.001* |
| PPD (mm) | 5.93 ± 0.39 | 4.39 ± 0.35 | 0.001* |
| CAL (mm) | 5.94 ± 0.39 | 4.52 ± 0.37 | 0.001* |
| BD (%) | 41.37± 2.98 | 45.63 ±0.267 | 0.001* |
*indicates significant p-value
[Table/Fig-4] represents the intergroup comparison of clinical parameters at the end of three months. There was statistically significant difference in OHI-S (p<0.05), GI (p<0.05), and BD (p<0.05) but in case of PPD (p<0.05) and CAL (p>0.05) there was no statistically significant difference.
Intergroup comparison of parameters after 3 months
| Variable | Group A (36) | GroupB (41) | p-value |
|---|
| GI 3 months | 0.33 ± 0.39 | 1.09± 0.15 | 0.001* |
| OHI-S 3 months | 0.79 ±0.37 | 2.25 ±0.28 | 0.001* |
| PPD(mm)3months | 4.25 ± 0.31 | 4.39 ± 0.35 | 0.057 |
| CAL(mm)3months | 4.45 ± 0.64 | 4.52 ± 0.37 | 0.558 |
| BD(%)3 months | 49.33 ± 4.72 | 45.63 ±0.267 | 0.001* |
*indicates significant p-value
Correlation of bone density with OHI-S and GI after three months in Group A [Table/Fig-5] showed negative correlation. The results showed that there is slight increase in Serum Calcium and vitamin D in group A after three months [Table/Fig-6].
Correlation of bone density at 3 months with GI and OHI-S at 3 months
| Variable n=36 | Group A (BD) (n=77) |
|---|
| GI Pearson Correlation | -0.390 |
| p-value | 0.001* |
| OHI–S Pearson Correlation | -0.358 |
| p value | 0.001* |
*indicates significant p-value
Mean serum calcium and vitamin D levels at baseline and after 3 months
| Groups | Serum Calcium Baseline Mean ± SD (mg/dl) | Serum Calcium 3months Mean ± SD (mg/dl) | p-value | Serum Vitamin D Baseline Mean ± SD (ng/ml | Serum Vitamin D Baseline Mean ± SD (ng/ml) | p-value |
|---|
| A | 9.21 ±0.17 | 9.86 ±0.19 | 0.001 | 25.97 ±1.31 | 36.01 ±1.23 | 0.001 |
| B | 9.28 ±0.16 | 9.35 ±0.15 | 0.001 | 25.53 ±0.24 | 25.62 ±0.22 | 0.001 |
| p-value | 0.043 | 0.001 | | 0.056 | 0.001 | |
Discussion
In the present study, the subjects in Group A received oral supplementation of calcium and vitamin D (a combined dose of 500mg calcium and 250 IU Vitamin D) once daily for three months. All the clinical parameters assessed in both groups showed that both interventions were effective in restoring periodontal health. Our results also showed as the bone density increased; gingival index and OHI-S were decreasing. All the clinical parameters were significant, which is in accordance to the results of Miley et al., [16] and Garcia et al., [23]. But the difference is that they had been giving higher doses of vitamin D supplementation for longer time period.
The study of Hiremath et al., [17] evaluated the anti-inflammatory effect of vitamin D on gingivitis at various doses which revealed that there was a dose-dependent anti-inflammatory effect of vitamin D on gingivitis and concluded that vitamin D was a safe and effective anti-inflammatory agent in doses ranging from 500 IU to 2000 IU. But in their study, subjects were found to be having only gingivitis; hence their analysis did not describe any effects of vitamin D on clinical parameters and effects on periodontitis. But in this study we have included subjects with periodontitis and analysed effect of calcium and vitamin D on clinical parameters and bone density. The increase in bone density may be due to the slight increase in serum calcium and vitamin D levels. A slight positive effect is seen on group A in our study.
Krall et al., [24] reported that vitamin D may have beneficial effects on periodontal disease and tooth loss, possibly because of its anti inflammatory effects. However, other studies [11] have shown that the anti inflammatory effect of vitamin D is evident only at doses of 500 IU and above. The present study shows that Group A, demonstrated an anti-inflammatory effect at the third month.
Our results show that even though SRP resulted in significant reduction in PPD and CAL, leading to an improvement in their periodontal status, a complete elimination of PPD and the resultant gain in CAL could not be obtained. Various factors are responsible for this as periodontitis is a multifactorial disease caused by tissue invading organisms, which can recolonize or reinfect [25] not only from periodontal pockets but also from other oropharyngeal habitats (mucous membranes, tongue, tonsils and saliva). Other studies by Fentoglu [26] et al., also reported a significant reduction in levels of serum TNF-α, IL1-β, and IL-6 in subjects with periodontitis at 3 months follow up after completion of non surgical periodontal treatment that included scaling and root planing. However, non surgical periodontal therapy cannot bring about complete elimination of all subgingival bacteria since re-colonisation [27] occurs over a period of time.
The slight improvement in clinical parameters and bone density in Group A may be because of the molecule LL-37 present in vitamin D has broad spectrum activity against Gram positive and Gram negative microorganisms, including those associated with periodontal disease [28]. Role of these peptides in the natural defence against colonisation by periodontal pathogens such as A. actinomycetemcomitans is proved in many studies [29]. Since bacteria do not develop resistance to antimicrobial peptides such as LL-37, it is postulated that vitamin D supplementation prevents anti microbial resistance as well as recolonization.
Recent studies reveal that there are three main mechanisms through which vitamin D and calcium supplementation are effective in reducing periodontitis which has been given in [Table/Fig-7].
Adjunctive effects of calcium and vitamin D supplementation in periodontitis [30–35]
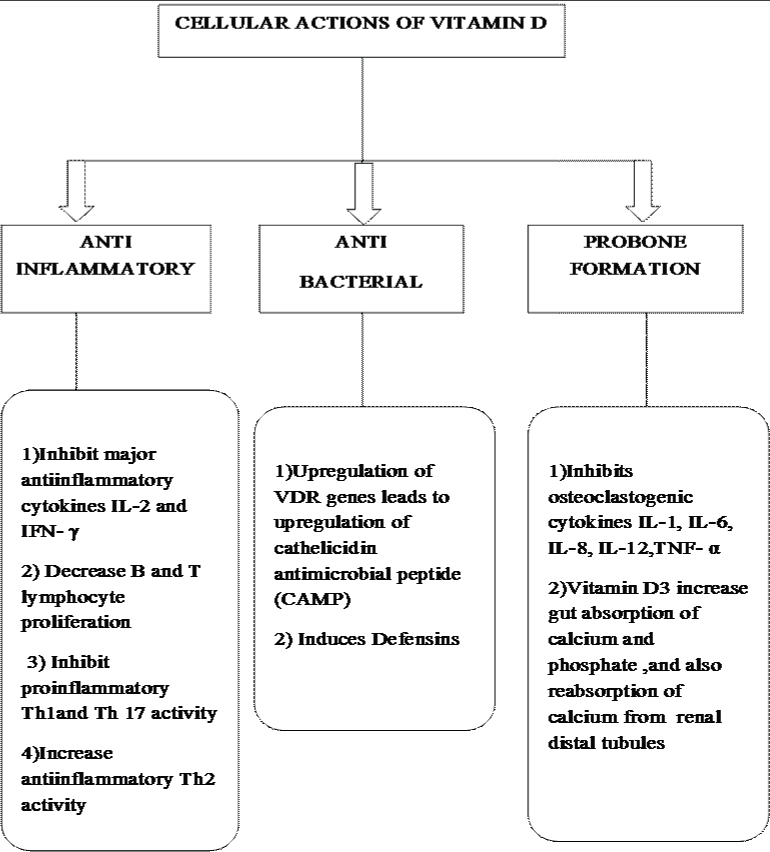
All these mechanisms together must have contributed to better periodontal status in group A subjects.
In short, as periodontal disease is associated with colonization of pathogenic bacteria in gingival epithelium, resulting in gingival inflammation, it is speculated that vitamin D may have a profound effect in prevention of this colonization with direct antimicrobial activity, as well as enhancement of the natural innate immune response without any antibiotic resistance. These results of the study strongly recommend that calcium and vitamin D can be given as an adjunct to SRP for better periodontal outcomes.
Limitations
Limitations of the study were we didn’t include medically compromised subjects with periodontitis and time period was only three months.
Conclusion
According to our study, we got superior results on periodontal parameters by oral supplementation of low dose of calcium and vitamin D. No side effects like colic pain were reported by any of the subjects in the time period of three months. Gingival inflammation reduced as the bone density increased. So, it can be concluded that vitamin D and calcium supplementation has got a slight positive effect in the periodontal treatment and it can be used as an adjunct to SRP for a better treatment outcome.
*indicates significant p-value
[1]. Hinrichs JE, Novak MJ, Classfication of Diseases and Conditions Affecting the Periodontium. In, Carranza FA(ed)Carranza’s Clinical Peridntology 2012 11th editionNew DelhiReed Elsevier India Private Limited:41 [Google Scholar]
[2]. Sreedevi M, Ramesh A, Dwarakanath C, Periodontal Status in Smokers and Nonsmokers: A Clinical, Microbiological, and Histopathological StudyInternational Journal of Dentistry 2012 :1-10. [Google Scholar]
[3]. Millen AE, Hovey KM, LaMonte MJ, Swanson M, Andrews CA, Kluczynski MA, Plasma 25-hydroxyvitamin D concentrations and periodontal disease in postmenopausal womenJ Periodontol 2013 84(9):1243-56. [Google Scholar]
[4]. Hayes CE, Nashold FE, Spach KM, Pedersen LB, The immunological functions of the vitamin D endocrine systemCell Mol Biol Noisy–Gd Fr 2003 49(2):277-300. [Google Scholar]
[5]. Bashutski JD, Eber RM, Kinney JS, Benavides E, Maitra S, Braun TM, The impact of vitamin D status on periodontal surgery outcomesJ Dent Res 2011 90(8):1007-12. [Google Scholar]
[6]. Amano Y, Komiyama K, Makishima M, Vitamin D and periodontal diseaseJ Oral Sci 2009 51(1):11-20. [Google Scholar]
[7]. Hildebolt CF, Effect of vitamin D and calcium on periodontitisJ Periodontol 2005 76(9):1576-87. [Google Scholar]
[8]. Dietrich T, Joshipura KJ, Dawson-Hughes B, Bischoff-Ferrari HA, Association between serum concentrations of 25-hydroxyvitamin D3 and periodontal disease in the US populationAm J Clin Nutr 2004 80(1):108-13. [Google Scholar]
[9]. Londhey V, Vitamin D Deficiency: Indian ScenarioJournal of The Association Physicians of India 2011 59:695-99. [Google Scholar]
[10]. Hodgkin P, Hine PM, Kay GH, Lumb GA, Stanbury SW, Vitamin-D deficiency in Asians at home and in BritainLancet 1973 2(7822):167-71. [Google Scholar]
[11]. Bhatia V, Dietary calcium intake - a critical reappraisalIndian J Med Res 2008 127(3):269-73. [Google Scholar]
[12]. Nutrient Requirements and Recommended Daily Allowances for Indians: A Report of the Expert Group of the Indian Council of Medical Research. Available from: http://www.icmr.nic.in/final/RDA-2010.pdf. [Last accessed on 2012 May 26] [Google Scholar]
[13]. Goswami R, Kochupillai N, Gupta N, Goswami D, Singh N, Dudha A, Presence of 25(OH) D deficiency in a rural North Indian village despite abundant sunshineJ Assoc Physicians India 2008 56:755-57. [Google Scholar]
[14]. Agarwal N, Mithal A, Dhingra V, Kaur P, Godbole MM, Shukla M, Effect of two different doses of oral cholecalciferol supplementation on serum 25-hydroxy-vitamin D levels in healthy Indian postmenopausal women: A randomized controlled trialIndian J Endocrinol Metab 2013 17(5):883-89. [Google Scholar]
[15]. Paul TV, Thomas N, Seshadri MS, Oommen R, Jose A, Mahendri NV, Prevalence of osteoporosis in ambulatory postmenopausal women from a semiurban region in Southern India: relationship to calcium nutrition and vitamin D statusEndocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol 2008 14(6):665-71. [Google Scholar]
[16]. Miley DD, Garcia MN, Hildebolt CF, Shannon WD, Couture RA, Anderson Spearie CL, Cross-sectional study of vitamin D and calcium supplementation effects on chronic periodontitisJ Periodontol 2009 80(9):1433-39. [Google Scholar]
[17]. Hiremath VP, Rao CB, Naik V, Prasad KV, Anti-inflammatory effect of vitamin D on gingivitis: a dose-response randomised control trialOral Health Prev Dent 2013 11(1):61-69. [Google Scholar]
[18]. Marwaha RK, Tandon N, Garg MK, Kanwar R, Narang A, Sastry A, Vitamin D status in healthy Indians aged 50 years and aboveJ Assoc Physicians India 2011 59:706-09. [Google Scholar]
[19]. Malhotra N, Mithal A, Gupta S, Shukla M, Godbole M, Effect of vitamin D supplementation on bone health parameters of healthy young Indian womenArch Osteoporos 2009 4(1-2):47-53. [Google Scholar]
[20]. Greene JC, Vermillion JR, The Simplified Oral Hygeine IndexJ Am Dent Assoc. 1939 1964 68:7-13. [Google Scholar]
[21]. Löe H, The Gingival Index, the Plaque Index and the Retention Index SystemsJ Periodontol 1967 38(6:Suppl):610-16. [Google Scholar]
[22]. (2D) SIDEXIS XG | Sirona Dental [Internet]. www.sirona.com/en/products/imaging-systems/2d-sidexis-xg/. [cited 2014 Sep 21]. Available from: http://www.sirona.com/en/products/imaging-systems/2d-sidexis-xg/ [Google Scholar]
[23]. Garcia MN, Hildebolt CF, Miley DD, Dixon DA, Couture RA, Spearie CLA, One-year effects of vitamin D and calcium supplementation on chronic periodontitisJ Periodontol 2011 82(1):25-32. [Google Scholar]
[24]. Krall EA, Wehler C, Garcia RI, Harris SS, Dawson-Hughes B, Calcium and vitamin D supplements reduce tooth loss in the elderlyAm J Med 2001 111(6):452-56. [Google Scholar]
[25]. Teughels W, Dekeyser C, Van Essche M, Quirynen M, One-stage, full-mouth disinfection: fiction or reality?Periodontol 2000 2009 50:39-51. [Google Scholar]
[26]. Fentoglu O, Kirzioğlu FY, Ozdem M, Koçak H, Sütçü R, Sert T, Proinflammatory cytokine levels in hyperlipidemic patients with periodontitis after periodontal treatmentOral Dis 2012 18(3):299-306. [Google Scholar]
[27]. Sbordone L, Ramaglia L, Gulletta E, Iacono V, Recolonization of the subgingival microflora after scaling and root planing in human periodontitisJ Periodontol 1990 61(9):579-84. [Google Scholar]
[28]. Ji S, Hyun J, Park E, Lee BL, Kim KK, Choi Y, Susceptibility of various oral bacteria to antimicrobial peptides and to phagocytosis by neutrophilsJ Periodontal Res 2007 42(5):410-19. [Google Scholar]
[29]. McMahon L, Schwartz K, Yilmaz O, Brown E, Ryan LK, Diamond G, Vitamin D-mediated induction of innate immunity in gingival epithelial cellsInfect Immun 2011 79(6):2250-56. [Google Scholar]
[30]. Bhalla AK, Amento EP, Krane SM, Differential effects of 1,25-dihydroxyvitamin D3 on human lymphocytes and monocyte/macrophages: inhibition of interleukin-2 and augmentation of interleukin-1 productionCell Immunol 1986 98(2):311-22. [Google Scholar]
[31]. Boonstra A, Barrat FJ, Crain C, Heath VL, Savelkoul HF, O’Garra A, 1alpha,25-Dihydroxyvitamin d3 has a direct effect on naive CD4(+) T cells to enhance the development of Th2 cellsJ Immunol Baltim Md. 1950 2001 167(9):4974-80. [Google Scholar]
[32]. Yuk JM, Shin DM, Lee HM, Yang CS, Jin HS, Kim KK, Vitamin D3 induces autophagy in human monocytes/macrophages via cathelicidinCell Host Microbe 2009 6(3):231-43. [Google Scholar]
[33]. Wang TT, Nestel FP, Bourdeau V, Nagai Y, Wang Q, Liao J, Cutting edge: 1,25-dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expressionJ Immunol Baltim Md 1950 2004 173(5):2909-12. [Google Scholar]
[34]. Nonn L, Peng L, Feldman D, Peehl DM, Inhibition of p38 by vitamin D reduces interleukin-6 production in normal prostate cells via mitogen-activated protein kinase phosphatase 5: implications for prostate cancer prevention by vitamin DCancer Res 2006 66(8):4516-24. [Google Scholar]
[35]. Anderson PH, Sawyer RK, Moore AJ, May BK, O’Loughlin PD, Morris HA, Vitamin D depletion induces RANKL-mediated osteoclastogenesis and bone loss in a rodent modelJ Bone Miner Res Off J Am Soc Bone Miner Res 2008 23(11):1789-97. [Google Scholar]