Spontaneous Chest Wall Interstitial Emphysema Secondary to Chronic Empyema Thoracis
Venkatraman S Bhat1, Manjunath Poojaramuddanahalli2, Natarajan Rajagopalan3, Karthik Gadabanahalli4
1 Director of Imaging Services, Department of Radiology, Narayana Health, Bangalore, Bommasandra, India.
2 Resident, Department of Pulmonology, Narayana Health, Bangalore, Bommasandra, India.
3 Senior Consultant, Department of Pulmonology, Narayana Health, Bangalore, Bommasandra, India.
4 Consultant, Department of Radiology, Narayana Health, Bangalore, Bommasandra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Venkatraman S Bhat, 309, Greenwoods Apt, Royal Gardenia, Bommasandra, Bangalore-560099, India. E-mail : bvenkatraman@gmail.com
Spontaneous extension of air from the pleural space to the chest wall, also referred to as pneumothorax necessitans (PN), is a rare occurrence. Few of such cases have been reported in the literature, some appear to have a pattern of extension from pleural cavity to chest wall. Clinical conditions known to predispose to this complication are pneumothorax, empyema thoracis and tuberculosis of the pleural space or rib. We report a case of PN arising as complication of postpneumonectomy empyema (PPE) secondary to broncho-pleural fistula. Imaging features are highlighted emphasizing the likely pattern of spread.
Emphysema necessitans, Empyema, MDCT, Tuberculosis complication
Case Report
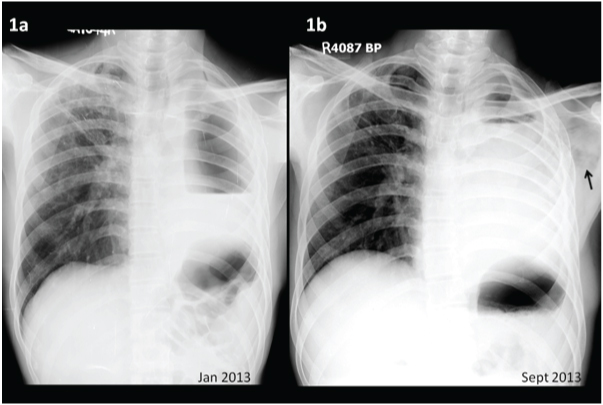
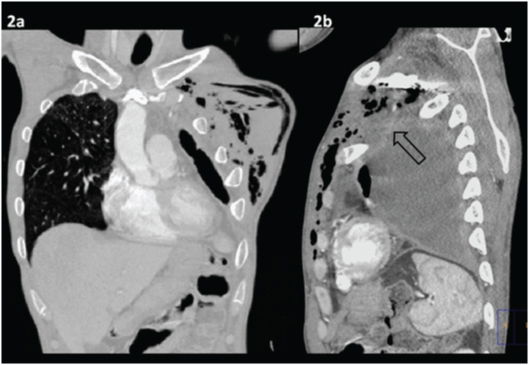
A 34-year-old male had left sided tubercular pleural effusion in 2008, for which he was treated with anti-tubercular medication. He was irregular on treatment and developed pyopneumothorax. After initial management by intercostal drainage, patient subsequently had undergone pneumonectomy. After remaining asymptomatic for 2 years, he presented again with cough associated with foul smelling expectoration. Fiberoptic bronchoscopy showed a small hole in the left bronchial stump representing a broncho-pleural fistula. Chest radiograph showed a large hydro-pneumothrax on left side [Table/Fig-1a], He was on conservative treatment for about 6 months, after which he presented again with exacerbation of spasmodic cough, expectoration, fever and left sided sever chest pain. On clinical evaluation, he was febrile, had tachycardia and tachypnea. There was tense, tender bulge with crepitus at left anterior hemithorax. Repeat bronchoscopy revealed increase in size of the broncho-pleural fistula. Radiograph revealed small air-fluid level in the left upper chest with complete opacification of rest of hemithorax [Table/Fig-1b]. There was speckled air-lucency in the soft tissues of the left upper chest. Right lung demonstrated the fibrotic parenchymal lesions at the upper zone. On multidetector computed tomography (MDCT) of the chest, a large pneumonectomy cavity was demonstrated, containing fluid [Table/Fig-2a]. Irregular contour of the wall of the cavity was observed at the superior aspect, adjacent to the first rib [Table/Fig-2b]. Small pockets of air were noted in the vicinity and extensive interstitial emphysema involving chest wall. Small lymph nodes were noted in the chest wall and supraclavicular region. On diagnostic aspiration foul smelling thick pus was drained, which on culture revealed growth of Burkholdheria pseudomalliei. He was treated with intravenous antibiotics ( meropenem, metronidazole) for 21 days. Empyema was drained with an intercostal chest tube and subsequently the cavity was irrigated with betadine. Patient responded well clinically. Chest tube was discontinued and patient was discharged home.
(a) Chest radiograph 6 month before presentation shows fibrotic lesions at right upper lobe and left hydropneumothorax. (b) Chest X ray at presentation shows persistent left hydropneumothorax and small pockets of air lucencies ( black arrow) in left upper chest
(a). Coronal CT image demonstrates extensive interstitial air in chest wall (b). Sagittal CT showing likely site of breach (Black arrow head)
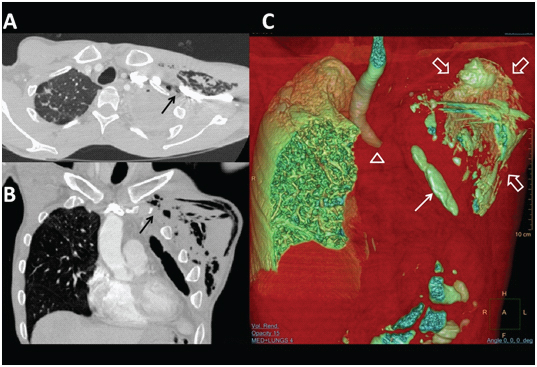
(a,b) Axial and coronal CT images illustrates likely point of breach in pleural boundary, around the first rib (black arrows). (c) Volume rendered images showing left bronchial stump (arrow head). Air pockets in pleural cavity (arrow) and chest wall (open arrows) are also demonstrated
Discussion
Pneumothorax necessitans (PN) is a rare condition [1,2]. Previous reports have described cases of pneumothorax, communicating with extrathoracic tissue planes (often subcutaneous) through a defect in the thoracic wall. Breach in the chest wall boundary was often due to the chronic inflammatory process, such as that caused by an abscess, empyema, osteomyelitis, and tuberculosis with prolonged thoracostomy [3], causing erosion and subsequent destruction of the bone or soft tissue separating the pleural cavity from the extrathoracic space. Chest wall emphysema is also known to occur around chest drainage tube sites [4]. Our patient had a longstanding empyema as a complication of pneumonectomy. Chest radiographs had demonstrated large air-fluid level in the immediate postoperative period which persisted in the subsequent 6 month follow-up. Patient also had intermittent episodes of spasmodic cough. Along with predisposing factors mentioned above, additional mechanical pressure due to cough likely to have caused disruption of pleural boundary and subsequent extension to left supraclavicular fossa, inter-muscular and soft tissue planes of the thorax. In our patient breach in the integrity of the pleural space occurred at the superior aspect just around the first rib, quite similar to observation in a previous study [1]. MDCT appears to be the best choice for evaluating the chest lesion as well as for demonstrating the likely point of extension to extra thoracic soft tissues [Table/Fig-3a-c]. PPE is an extremely serious complication because it is impossible to eliminate the space containing the infection and difficult to sterilize the pleural space. Approximately 60% to 80% of patients with PPE have a bronchopleural or an oesophago-pleural fistula. Therefore, all patients suspected of this complication should undergo a chest CT and a bronchoscopy. Delayed intervention is known to result in extension to the brachial plexus and result in neurological deficits.
Conclusion
This case highlights the rare complication of PPE resulting in PN, with an insight to the possible mechanism. There is a definite role of tuberculosis in delayed resolution of cavity and the subsequent complication of extra-thoracic rupture. In the right clinical context, careful attention should be paid to plain radiographic observations of small pockets of air in chest wall in order to pursue more specific information on MDCT. Special attention should be paid to the interface between first rib and superior pleural margin, sometimes supplemented with oblique reconstructions, to illustrate defect in pleural cavity.
[1]. Kuan YC, How SH, Yeen WC, Ng TH, Fauzi AR, Empyema thoracis complicated by pneumothorax necessitans manifesting as lobulated, localized subcutaneous emphysematous swellingsAnn Thorac Surg 2011 91(6):1969-71.doi: 10.1016 [Google Scholar]
[2]. Tripathi SP, Massad MG, Mehta VK, Benedetti E, Geha AS, Pneumothorax necessitans presenting as a presternal pneumothoracoceleAnn Thorac Surg 2000 69:266-67. [Google Scholar]
[3]. Garg R, Singhal S, Srivastava P, Pneumothorax necessitans as a complication of closed tube thoracostomyThe Internet Journal of Radiology 2007 7:2 [Google Scholar]
[4]. Paramasivam E, Bodenham A, Air leaks, pneumothorax, and chest drainsContin Educ Anaesth Crit Care Pain 2008 8(6):204-9.doi:10.1093 [Google Scholar]