Introduction
Involvement of the skeletal system accounts for nearly one to three percent of all cases of tuberculosis [1] and isolated involvement of clavicle is rare [2]. Diagnosis of osteoarticular tuberculosis often poses difficulty due to non-availability of ‘simple’ and reliable disease marker, and gold standard for making diagnosis is still mycobacterial culture, though histopathology can suggest diagnosis in >90% of cases [3]. Procurement of specimen for microbiological and tissue diagnosis is ‘a recondite treatise’ due to local anatomy, the precision of technique involved and type of tissue (bone) required for study. The diagnosis of osteoarticular tuberculosis is clinico-radiological, especially in endemic regions, and most importantly in absence of any ambiguity between patient’s history, clinical findings, and supportive and radiological investigations including computed tomography/magnetic resonance imaging findings [4]. We are presenting this study highlighting a differential diagnosis based clinico-radiological approach for diagnosis of a rare case of clavicle tuberculosis.
Case Report
An average built female of 41 years of age, from moderate socioeconomic status, presented to Orthopaedic OPD (outpatient department) with complaints of insidious onset, gradually increasing swelling and pain of the inner aspect of her right collarbone for about 6 months. There was no history of trauma, fever, chest complaint or recent sore throat, loss of weight or appetite, night sweats or any other constitutional symptom. Neither was any history of joint pain, back pain, or swelling in any other part of the body. It was not related to posture, respiration or coughing. There was no past history of any tubercular infection or antitubercular treatment, but there was history suggestive of possible exposure to tuberculosis as one of her close friend recently treated for pulmonary tuberculosis.
One month before reporting to us, patient was treated elsewhere and radiograph of both the clavicles were interpreted as normal by the treating physician, and was managed symptomatically with analgesics and broad spectrum empirical antibiotic for 3 weeks. As no improvement in symptoms was noted, computed tomography (CT) of right clavicle was done followed by FNAC (fine needle aspiration cytology). Patient was told about trivial nature of the lesion and was sent back with reassurance and analgesics, but the pain kept on increasing, and presently only barely relieved by usual doses of analgesics.
Clinical examination revealed a 3 × 2 cm globular swelling, tender on palpation, firm to hard in consistency, fixed to underlying bone, arising from the region of medial end of right clavicle and sternoclavicular joint [Table/Fig-1], largely in relation to the clavicle as the swelling was merging imperceptibly with the clavicle. Overlying skin was free and normal looking. Local temperature was not raised. Terminal abduction and flexion of right shoulder elicited pain in the swelling. Distal neurovascular status of the right upper limb was intact. There was no clinical evidence of cervical or axillary lymphadenopathy. The lung fields were clear on auscultation. Blood investigations revealed haemoglobin 12 g/dl, total leucocyte count of 10,000 cells/mm3 with neutrophils 60% and lymphocytes 37%. The erythrocyte sedimentation rate (ESR) was 40 mm in 1st hour. Her renal and liver function tests were within normal limits. Serum rheumatoid factor and ANA (Anti-nuclear antibody) results were negative. Anteroposterior radiograph of both the clavicles was repeated this time and was again found to be normal.
CT and FNAC reports were reviewed. CT reported a 14 × 12 mm well defined sclerotic lesion at the sternal end of right clavicle antero-inferiorly with no evidence of any cortical breech or overlying soft tissue swelling, with intact musculofascial planes and sternoclavicular joint, and with differential diagnosis of osteoma/bone island [Table/Fig-2]. FNAC revealed inconclusive cytology, with no bacteria on Gram’s staining, negative aerobic bacterial culture and negative AFB smear examination. As there was history of possible exposure to tuberculosis, Mantoux (tuberculin) skin test was ordered and the report came as reactive with 24 × 23 mm induration at 72 hours. Her sputum smear for AFB examined on three consecutive days was negative. Chest X-ray (PA) view was also normal. Presently, we do not order serological tests for the diagnosis of tubercular infection.
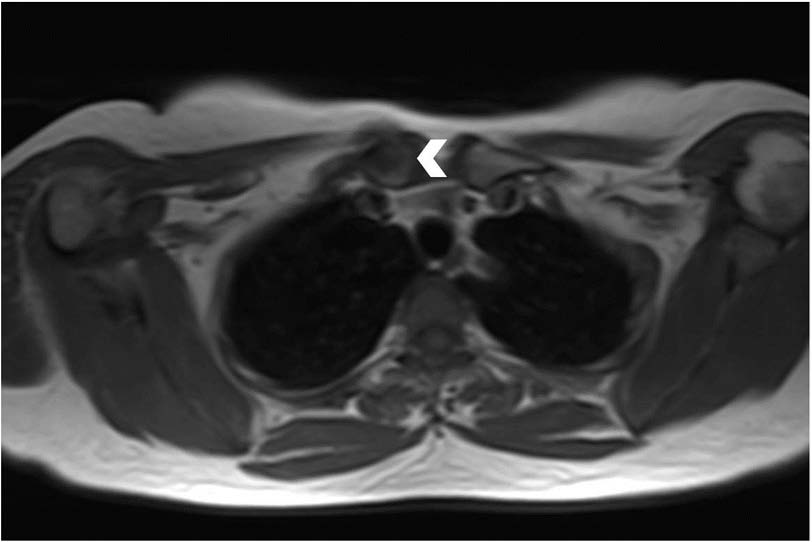
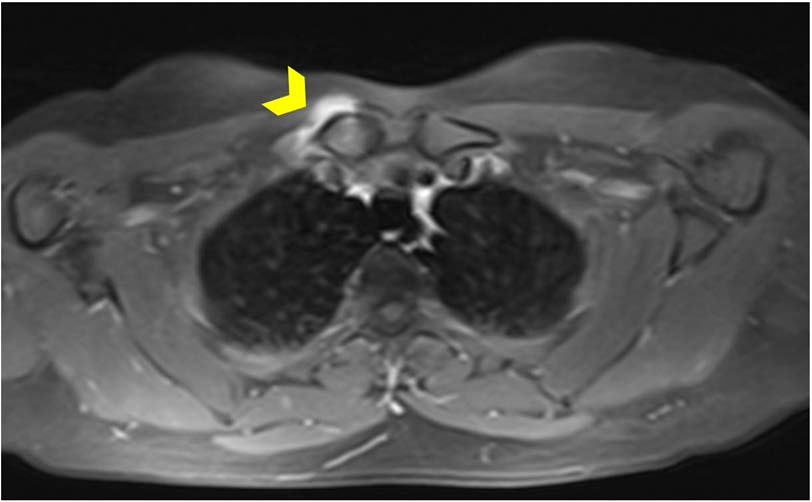
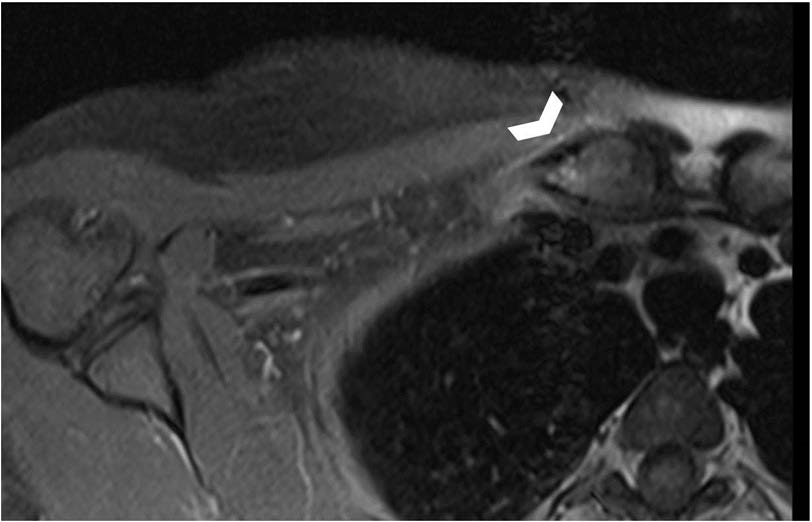
The differential diagnosis considered, after excluding traumatic conditions, were subacute and chronic forms of osteomyelitis including tubercular osteomyelitis as there was history of her possible exposure to tuberculosis. As there was poor correlation of her symptoms with the reported CT findings, we also considered tumour or tumour like conditions, rheumatological affections including degenerative and idiopathic disorders. Magnetic resonance imaging (MRI) of right clavicle was ordered to further elucidate the disease process, and it revealed focal periosteal reaction and thickening involving medial end of right clavicle with sparing of adjacent sternoclavicular joint. T1-weighted MR images showed low signal replacement of normal marrow fat signal [Table/Fig-3], high signal intensities on T2-weighted images [Table/Fig-4], and contrast enhancement on T1-weighted images [Table/Fig-5]. There was sparing of sternoclavicular joint.
Showing globular swelling arising from the region of medial end of right clavicle

CT image with sclerotic lesion at the sternal end of right clavicle with no evidence of any cortical breech or overlying soft tissue swelling and with intact musculofascial planes

Transverse T1-weighted MR image showing low signal replacement of the normal marrow fat signal
Coronal T2-weighted MR image showing heterogenous hyperintensity in the medial end of right clavicle

Fat suppressed, T1-weighted transverse MR image with contrast showing marked periosteal enhancement (arrow head) with heterogenous enhancement in the medial end of right clavicle
In view of the historical facts and clinico-radiological correlation including MRI findings, working diagnosis of tuberculosis of medial end of right clavicle was made and patient was started on anti-tuberculous chemotherapy. Patient received isoniazid (INH), rifampicin (RMP), pyrazinamide (PYZ) and ethambutol (EMB) for two months, followed by INH, RMP and EMB for next 4 months, and INH and RMP for next 6 months.
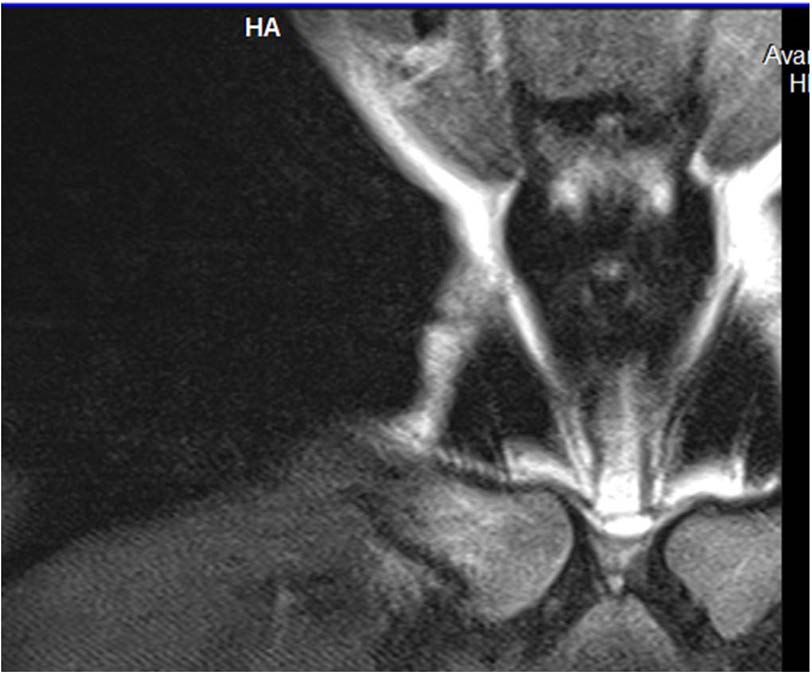
Non steroidal anti-inflammatory medication was stopped after about three weeks, and was advised on ‘as and when required basis.’ Patient reported complete cessation of pain in about 3 months, though near-total subsidence of swelling took about 6 months. Patient did not need to take analgesics after 3 months. After 9 months of anti tuberculous therapy, MRI of right clavicle repeated and it showed significant resolution of initial findings [Table/Fig-6,7]. At two years of follow-up, patient was completely symptom free.
Post treatment, T2-weighted coronal MR image showing significant resolution of the lesion at the medial end of right clavicle
Post-treatment, transverse T1-weighted MR image with contrast showing subsidence of the initial periosteal reaction at the medial end of right clavicle (arrow head)
Discussion
Involvement of the skeletal system accounts for less than 3% of all cases of extrapulmonary tuberculosis [1] and isolated involvement of sternum and clavicle is rare [5,6]. Tuberculosis of the clavicle without involvement of the adjacent joint accounts for <1% of all osteoarticular tuberculosis [2]. Conventional radiography is the first imaging study undertaken, but may be difficult to interpret because of artifacts from the underlying superior mediastinal structures [7], especially in early cases, as we observed in our patient.
The differential diagnosis considered for atraumatic, chronic, insidious onset, firm to hard, painful swelling arising from the medial end of the clavicle unilaterally in this middle aged immunocompetent female included affections of medial end of clavicle proper or of sternoclavicular joint or combination of these two groups. Chronic osteomyelitis with or without sternoclavicular joint involvement, either due to tuberculosis or non-specific pyogenic infection was the initial consideration. Pyogenic osteomyelitis or arthritis of around 6 month’s duration generally produces more destruction [8]. Besides, historically, patient had no symptomatic improvement with antibiotics. Patient did not have constitutional symptoms of tuberculosis, but she did have positive history of exposure to tuberculosis and reactive Mantoux skin test.
As a rule, reactive Mantoux skin test to be interpreted with caution in endemic areas, as most of the individuals in endemic areas are exposed to the infection either from natural sources or due to bacille Calmette-Guérin immunization with booster effect of repeated subclinical infections. Hence, Mantoux skin test to be approached with wisdom of a sage and not with calculations of a mathematician. We considered 24 X 23 mm induration as strongly corroborative in view of her recent possible exposure. Recently, Quantiferon-TB Gold test (QFT-G) is proposed to be a more reliable marker than Mantoux skin test with higher sensitivity as well as specificity and a better correlation with exposure to mycobacterial tuberculosis [9]. S Sollai et al., reported that Interferon gamma release assays (IGRAs) showed no better performance than tuberculin skin test in children in low income countries [10]. As stated earlier, we do not advocate serodiagnostic tests for tuberculosis due to inconsistent and imprecise results. In July 2011, WHO recommended that serological tests should not be used in individuals suspected of active pulmonary or extra-pulmonary TB, irrespective of their HIV status [11]. Government of India, too, in June 2012, has imposed a ban on manufacture, sale, distribution, use and import of the sero-diagnostic test kits for diagnosis of tuberculosis [12]. Regarding systemic clinical symptoms or constitutional symptoms, around just over 50% may have at least one systemic symptoms, and remaining may have none [13]. Our patient had no constitutional symptoms.
Most of the authors have described lytic lesion or erosion of the articular ends of the clavicle in radiography, if present [2,6]. Periosteal reaction, as observed in conventional radiography, is not a prominent feature of tuberculous osteomyelitis [14,15], CT reveals destructive changes in bone better, particularly on bone window settings but marrow changes are difficult to identify. CT features of sterno-clavicular tuberculosis are bone and cartilage destruction, soft tissue masses crossing fascial planes with rim (abscess) and diffuse enhancement (granulation tissue), calcifications and underlying pleuro-parenchymal tubercular involvement [5,6]. Nuclear medicine imaging can provide significant information in the diagnosis and follow up of osteoarticular tuberculosis. Recently, 99mTC-labeled ciprofloxacin bone scan reported to be a promising tool for monitoring drug response in extra-spinal skeletal tuberculosis, almost akin to sputum microscopy for pulmonary tuberculosis [16].
More recently, FDG PET/CT is proposed to be helpful for detecting asymptomatic and abnormal lesions, and specifically for monitoring of therapeutic response in select cases of extrapulmonary tuberculosis where sputum culture is unavailable [17–19]. But, in a developing country, affordability and cost as well as availability of this diagnostic modality remains an important matter of contention. On MR imaging, osteomyelitis is characterized by [6] low signal replacement of the normal marrow fat signal on T1-weighted images, with high signal intensities on T2-weighted images and enhancement on T1-weighted images. Our patient revealed all these characteristic MR findings. Furthermore, devitalized areas of the bone show increased SI on T2-weighted images with lack of central enhancement and Bony destruction is demonstrated as a defect in the hypointense cortical rim [6]. In this patient, disease process had not progressed enough to cause any apparent bony destruction as noted on the radiological investigations. Marrow SI (signal intensity) changes and periosteal reaction were the dominant MRI findings.
Marrow SI changes may represent the earliest change. T2 weighted images in sterno-clavicular tuberculosis may show hyperintensity due to tubercular joint effusion or hypointensity due to internal debris, septations, loose bodies, calcifications and hemosiderin deposits because of bleeding [6]. Changes of cellulitis (seen as replacement of subcutaneous fat signal on T1-weighted images with oedema and enhancement) and myositis (showing hyperintensities of the involved muscles on T2-weighted images with their enlargement) may be seen. Follow up MRI was done following 9 months of anti-tubercular treatment showed marked resolution of marrow signal changes and post-contrast periosteal enhancement.
We did not consider fungal osteomyelitis, as this disease is not endemic in India and there was no history of any penetrating trauma [20], or any other risk factor for fungal osteomyelitis [21,22]. The most common organism causing mycotic infections are Candida and mainly present as discitis or osteomyelitis of the spine [23]. Candida osteomyelitis generally involves 2 or more sites. Gamaletsou MN et al., while analysing 207 cases of adult and paediatric candida osteomyelitis cases reported only two cases of costoclavicular joint affection with no isolated clavicle involvement. They observed that systemic inflammatory response is usually absent and the infection was found to be more frequent in nonimmunosuppressed patients. Infection of vertebrae in adults, and femur and humerus in children are more likely. It exhibits non-specific signs in diagnostic imaging with decreased signal intensity on T1-weighted images, as well as increased signal intensity on T2-weighted images on MRI [24].
Neoplastic involvement of the clavicle is a rare occurrence and most commonly reported site varies from lateral end to more or less equal distribution [25,26], Clinically, osteoid osteoma would have been a neoplastic differential diagnosis in our case due a few points in initial presentation, but this is a rare diagnosis too. However, further elaboration of symptomatology and radiological evidence could not support it. Classic symptomatology of osteoid osteoma includes [27] nocturnal pain which is promptly relieved by salicylates, such as aspirin, usually in less than half an hour. This presentation is typical in greater than 75% of patients and provides an important clue to the diagnosis. Local swelling and point tenderness are present in some patients. Technetium 99m bone scan is useful if osteoid osteoma is suspected but the lesion is not clearly demonstrated on plain radiographs, and once the general area of the lesion has been localized with bone scan, cross-sectional imaging with CT best demonstrates the well-circumscribed area representing the nidus, but, the reliability of CT diminishes when the nidus is in a cancellous location because of the lack of perinidal density alteration [28]. Because nidus of the osteoid osteoma have highly heterogeneous and variable appearance on MRI [29], its characterization is generally difficult. Nidus is typically seen as low signal on T2-weighted images and as intermediate signal on T1-weighted images. Due to the accompanying soft tissue mass, bone marrow oedema and presence of joint effusion, MRI can result in deceptive images and wrong diagnoses.
Diagnostic dilemma between fibrous dysplasia and chronic osteomyelitis has been described [30]. The radiographic features of fibrous dysplasia vary widely. The normal bone is replaced by tissue that is more radiolucent, with a grayish “ground-glass” pattern that is similar to the density of cancellous bone but is homogeneous, with no visible trabecular pattern. Often, the diameter of the bone is increased by growth of the lesion, but the lesion continues to be bounded by the shell of reactive bone [31]. Most of the authors have reported malignant tumours to be more common than benign ones [25]. As reported by Basarir K et al., there is significant correlation between the age of the patient and malignancy risk, and the best cut-off is 50 years of age, including metastasis, and with the exception of paediatric sarcomas such as Ewing’s sarcoma or osteosarcoma. Clavicle is also unusual site for metastasis, with a reported incidence between 0% and 15% [32]. Bone island or enostosis [33,34] is the differential diagnosis for typically asymptomatic, incidentally diagnosed, ovoid or round homogenously dense sclerotic lesion on radiography. It may be found anywhere in the skeleton but pelvis, femur, and other long bones are preferential sites. On CT a bone island appears as a low-attenuation focus, exhibiting (as on radiography) its characteristic brush borders. On MRI, it exhibits low signal intensity on all sequences. The clavicle is an unusual location for a bone island.
The sternoclavicular joint is a true diarthrodial synovial joint and hence prone to the abuses of rheumatological inflammatory processes. The important rheumatological diseases involving sternoclavicular joint are rheumatoid arthritis, the seronegative arthropathies (ankylosing spondylitis, Reiter’s syndrome, psoriatic arthritis) and crystal arthropathies (gout and pseudogout). Some other rheumatological conditions with overlapping features are Friedreich’s disease, condensing osteitis, and uncommon to rare conditions like neuropathic arthropathy, hemophilic pseudotumour, brown tumour of hyperparathyroidism, polymyalgia rheumatica and amyloid deposits in chronic systemic inflammatory disorders. The most common clinical presentation of these rheumatological and related disorders is pain and swelling in the area of sternoclavicular joint. Conventional anteroposterior radiographs may show subchondral sclerosis, osteophytes, narrowing of the joint space, hyperostosis and calcification of the surrounding tissues, but may be difficult to interpret because of artifacts from the underlying superior mediastinal structures. General inflammatory markers (white cell count, ESR and the level of CRP), the level of rheumatoid factor and antinuclear antibodies and tissue antigen tests for HLA-B27 are useful initial screening tests [7]. On MR imaging [35], T1 weighted sequences demonstrate sternocostoclavicular joint involvement and degenerative alterations; while T2 weighted sequences and fat suppression sequences better showed articular space, articular cartilage, erosions and soft tissue swelling, T1 weighted with fat suppression sequences after Gd-DTPA administration allowed the detection of inflammation signs like bone marrow oedema, soft tissue involvement and intraarticular effusion. CT/MRI may help in the early diagnosis of erosions and differentiation from osteomyelitis and bone tumours [35]. We did not order HLA-B27 typing as there was no clinicohistorical evidence of any axial spondyloarthropathy.
Ischemic necrosis of medial end of the clavicle [33,36] is a rare disorder of unknown etiology as was suggested by Friedrich in 1924. Necrosis of the bone is the hallmark of this disorder. Clinically, it may present as swelling and tenderness at medial end of clavicle, usually of weeks to years duration. Radiographs (tomograms) usually reveal bone destruction with irregularity and some deformity of sternal end of clavicle. Finding on MRI consist of low signal intensity in both T1 & T2 weighted images corresponding to the sclerotic areas due to bone necrosis, and a rim of high to intermediate signal intensity consistent with deposition of fat [37].
Osteitis condensans of medial end of clavicle [38] is a rare degenerative condition affecting women of late child bearing age. Non-specific signs of inflammation in haematology report, like ESR or leucocyte counts, may be raised but markers of bone metabolism, like serum alkaline phosphatase is within normal limits. Radiographically, enlargement and sclerosis of the medial one-third of the clavicle, especially inferior margin of the head, are seen without associated changes in the sternoclavicular joint. CT may show sclerosis and obliteration of marrow cavity. Periosteal reaction is absent in radiography, but may be present histopathologically [33]. MRI [39] is the diagnostic modality which differentiates it from osteomyelitis. The TI weighted images showed an area of low signal intensity and an area with a complete lack of signal at the medial end of the clavicle. The T2 weighted images showed low signal intensities in this region.
Tietze’s syndrome [40] is a diagnosis of exclusion, of known etiology, presenting with sudden or gradual onset non-suppurative painful swelling in the region of anterior chest wall, most commonly involving the costochondral junction of 2nd rib, but the sternoclavicular joint and costochondral junction of 1st through 9th rib may be involved. Pain often exacerbated by deep inspiration, coughing, sneezing, bending forward or lying prone. Examination reveals firm tenderness. Local temperature may be raised, but there is no local redness [41]. Conventional radiological methods (standard x-rays, conventional tomography) help to exclude bone lesions, but they are not able to show cartilage damage. The spectrum of CT findings includes focal cartilage enlargement, ventral angulations of the costal cartilage and normal anatomic features. The specific MR findings include focal cartilage enlargement, oedema of the cartilage and the subchondral bone, vivid and rapid contrast enhancement of the cartilage and peri-articular structures involved [42].
After clinicohistorical and radiological correlation including MRI findings, diagnosis of tuberculosis of medial end of right clavicle without involvement of sternoclavicular joint was made and patient was started on anti-tubercular chemotherapy. It has been frequently stressed that the diagnosis of osteoarticular tuberculosis is clinico-radiological in endemic areas, but microbiological/tissue diagnosis should be obtained if any doubt in establishing diagnosis persists [4]. As yet, there is no standardized anti-tuberculosis chemotherapy regimen, though several formulae have been recommended. First-line therapy for M. tuberculosis should include a combination of INH, RMP, PYZ and either EMB or streptomycin [43].
Conclusion
Meticulous clinico-radiological correlation can avoid biopsy and is an important aspect of treatment of osteoarticular tuberculosis, and is true for endemic regions. Repeat CT/MRI during course of therapy establishes the efficacy of chemotherapy. This study doesn’t advocate imprudent omission of necessary diagnostic modality like biopsy for culture and histopathology, to arrive at a potentially curable serious disease, but gives consideration for clinico-radiological approach if no diagnostic dilemma exists between historical facts, clinical findings and radiological reports, and with support of advanced imaging modalities like CT and MRI. If decision is made for clinico-radiological approach, the clinician should scrupulously follow response to treatment, and on slightest doubt should plan for biopsy. This study may serve as a template for further prospective studies to determine optimum and efficient diagnostic workup resulting in complete cure with minimum scars, literally or figuratively.
[1]. Tuli SM, Tuberculosis of the skeletal system: bone, joints, spine and bursal sheaths 2008 4th ednNew DelhiJaypee Brothers Medical PublishersChapter 1, epidemiology and prevalence; p.4 [Google Scholar]
[2]. Aggarwal AN, Dhammi IK, Singh AP, Kumar S, Goyal MK, Tubercular osteomyelitis of the clavicle: a report of four casesJournal of Orthopaedic Surgery 2009 17(1):123-26. [Google Scholar]
[3]. Agrawal V, Patgaonkar PR, Nagariya SP, Tuberculosis of spineJ Craniovertebr Junction Spine 2010 1(2):74-85. [Google Scholar]
[4]. Jain AK, Jena SK, Singh MP, Dhammi IK, Ramachadran VG, Dev G, Evaluation of clinico-radiological, bacteriological, serological, molecular and histological diagnosis of osteoarticular tuberculosisIndian J Orthop 2008 42(2):173-77. [Google Scholar]
[5]. Bezza A, Niamane R, Benbouazza K, Tuberculosis of the sternoclavicular joint: report of two casesRev Rhum Engl Ed 1998 65:791-94. [Google Scholar]
[6]. Shah J, Patkar D, Parikh B, Parmar H, Varma R, Patankar T, Tuberculosis of the sternum and clavicle: imaging findings in 15 patientsSkeletal Radiol 2000 29:447-53. [Google Scholar]
[7]. Robinson CM, Jenkins PJ, Markham PE, Beggs I, Disorders of the sternoclavicular jointJ Bone Joint Surg Br 2008 90(6):685-96. [Google Scholar]
[8]. Resnick D, Osteomyelitis, septic arthritis, and soft tissue infections: organisms. In: Resnick D, editorDiagnosis of bone and joint disorders 2002 4th edPhiladelphiaSaunders:2511-2624. [Google Scholar]
[9]. Kashyap RS, Nayak AR, Gaherwar HM, Husain AA, Shekhawat SD, Jain RK, Latent TB infection diagnosis in population exposed to TB subjects in close and poor ventilated high TB endemic zone in IndiaPLoS One 2014 9(3):e89524 [Google Scholar]
[10]. Sollai S, Galli L, de Martino M, Chiappini E, Systematic review and meta-analysis on the utility of Interferon-gamma release assays for the diagnosis of Mycobacterium tuberculosis infection in children: a 2013 updateBMC Infect Dis 2014 14(Suppl 1):S6 [Google Scholar]
[11]. Commercial serodiagnostic tests for diagnosis of tuberculosis. Policy Statement. Geneva: World Health Organization; 2011. [accessed on June 8, 2014]. World Health Organization. WHO/HTM/TB/2011.5. Available from:http://www.tbevidence.org/documents/policies/WHO%20Policy%20Statement%20on%20Commercial%20TB%20Serodiagnostic%20Tests%202011.pdf [Google Scholar]
[12]. Government of India Gazette Notification Nos. G.S.R. 432 (E) and G.S.R. 433 (E) dated 7th June 2012(Annexure-B). [accessed on June 8, 2014] Available from:http://www.egazette.nic.in/WriteReadData/2012/E_264_2012_029.pdf [Google Scholar]
[13]. Hee Jung Yoon, Young Goo Song, Woo Il Park, Jae Pil Choi, Kyung Hee Chang, June Myung Kim, Clinical Manifestations and Diagnosis of Extrapulmonary TuberculosisYonsei Med J 2004 45(3):453-61. [Google Scholar]
[14]. Peter Renton, Periosteal reaction; bone and joint infections; sarcoid. In:Davis Sutton, editorTextbook of Radiology and Imaging 2003 7th edEdinburghChurchill Livingstone:1166 [Google Scholar]
[15]. Kao HK, Yang WE, Shih HN, Chang CH, Physeal change after tuberculous osteomyelitis of the long bone in childrenChang Gung Med J 2010 33(4):453-60. [Google Scholar]
[16]. Agrawal M, Bhardwaj V, Tsering W, Sural S, Kashyap R, Dhal A, Use of Technetium 99m–ciprofloxacin scan in Pott’s spine to assess the disease activityInt Orthop 2012 36(2):271-76. [Google Scholar]
[17]. Go SW, Lee HY, Lim CH, Jee WH, Wang YP, Yoo IeR, Atypical disseminated skeletal tuberculosis mimicking metastasis on PET-CT and MRIIntern Med 2012 51(20):2961-65. [Google Scholar]
[18]. Heysell SK, Thomas TA, Sifri CD, Rehm PK, Houpt ER, 18-fluorodeoxyglucose positron emission tomography for tuberculosis diagnosis and management: a case seriesBMC Pulm Med 2013 13:14doi: 10.1186/1471-2466-13-14 [Google Scholar]
[19]. Martinez V, Castilla-Lievre MA, Guillet-Caruba C, Grenier G, Fior R, Desarnaud S, (18) F-FDG PET/CT in tuberculosis: an early non-invasive marker of therapeutic responseInt J Tuberc Lung Dis 2012 16(9):1180-85. [Google Scholar]
[20]. Uppin SG, Sundaram C, Umamahesh M, Chandrashekar P, Rani YJ, Prasad VB, Lesions of the bones of the hands and feet: a study of 50 casesArch Pathol Lab Med 2008 132(5):800-12. [Google Scholar]
[21]. Frazier DD, Campbell DR, Garvey TA, Wiesel S, Bohlman HH, Eismont FJ, Fungal infections of the spine. Report of eleven patients with long-term follow-upJ Bone Joint Surg Am 2001 83-A(4):560-65. [Google Scholar]
[22]. Mihalko MJ, Tuberculosis and other unusual infections. In: S. Terry Canale, James H. Beaty, editorsCampbell’s operative orthopaedics 2013 12th edPhiladelphia, PAElsevier Mosby:784-86. [Google Scholar]
[23]. Sethi S, Siraj F, Kalra KL, Chopra P, Aspergillus vertebral osteomyelitis in immunocompetent patientsIndian J Orthop 2012 46(2):246-50. [Google Scholar]
[24]. Gamaletsou MN, Kontoyiannis DP, Sipsas NV, Moriyama B, Alexander E, Roilides E, Candida osteomyelitis: analysis of 207 pediatric and adult cases (1970-2011)Clin Infect Dis 2012 55(10):1338-51. [Google Scholar]
[25]. Kapoor S, Tiwari A, Kapoor S, Primary tumours and tumourous lesions of clavicleInt Orthop 2008 32(6):829-34. [Google Scholar]
[26]. Ren K, Wu S, Shi X, Zhao J, Liu X, Primary clavicle tumours and tumourous lesions: a review of 206 cases in East AsiaArch Orthop Trauma Surg 2012 132(6):883-89. [Google Scholar]
[27]. Adam G, Gernot J, Wolfgang R, Bone-Forming (Osteogenic) LesionsIn: Differential Diagnosis of Orthopaedic Oncology 2006 2nd edPhiladelphiaLippincott Williams & Wilkins:60 [Google Scholar]
[28]. Herring John A, Benign Musculoskeletal TumoursIn: Tachdjian’s Pediatric Orthopaedics 2013 5th edPhiladelphiaSaunders Elsevier:1114 [Google Scholar]
[29]. Gokce E, Ayan E, Celikyay F, Acu B, Radiological imaging findings of a case with vertebral osteoid osteoma leading to brachial neuralgiaJ Clin Imaging Sci 2013 3:54 [Google Scholar]
[30]. Weerasuriya T, Nashi S, Morgan A, Ebizie A, A dilemma of fibrous dysplasia versus chronic osteomyelitis of the clavicleBMJ Case Rep 2012 2012:bcr1220115319 [Google Scholar]
[31]. DiCaprio MR, Enneking WF, Fibrous dysplasia. Pathophysiology, evaluation, and treatmentJ Bone Joint Surg Am 2005 87(8):1848-64. [Google Scholar]
[32]. Basarir K, Polat O, Saglik Y, Yildiz Y, Bone tumours of the clavicle: risk of malignancy in the elderly and safe needle biopsyOrthopedics 2010 33(6):397 [Google Scholar]
[33]. Greenspan A, Gerscovich E, Szabo RM, Matthews JG 2nd, Condensing osteitis of the clavicle: a rare but frequently misdiagnosed conditionAJR Am J Roentgenol 1991 156:1011-15. [Google Scholar]
[34]. Adam G, Gernot J, Wolfgang R, Bone-Forming (Osteogenic) LesionsIn: Differential Diagnosis of Orthopaedic Oncology 2006 2nd edPhiladelphiaLippincott Williams & Wilkins:51-59. [Google Scholar]
[35]. Guglielmi G, Cascavilla A, Scalzo G, Salaffi F, Grassi W, Imaging of sternocostoclavicular joint in spondyloarthropathies and other rheumatic conditionsClin Exp Rheumatol 2009 27(3):402-08. [Google Scholar]
[36]. Levy M, Goldberg I, Fischel RE, Friedrich’s disease: Aseptic necrosis of the sternal end of the clavicleJ Bone Joint Surg Br 1981 63:539-41. [Google Scholar]
[37]. Jurik AG, Noninflammatory sclerosis of the sternal end of the clavicle: a follow-up study and review of the literatureSkeletal Radiol 1994 23(5):373-78. [Google Scholar]
[38]. Kruger GD, Rock MG, Munro TG, Condensing osteitis of the clavicle. A review of the literature and report of three casesJ Bone Joint Surg Am 1987 69(4):550-57. [Google Scholar]
[39]. Vierboom MA, Steinberg JD, Mooyaart EL, van Rijswijk MH, Condensing osteitis of the clavicle: magnetic resonance imaging as an adjunct method for differential diagnosisAnn Rheum Dis 1992 51(4):539-41. [Google Scholar]
[40]. Tietze syndrome. The National Organization for Rare Disorders (NORD); updated 2008 April 16. [accessed on June 8,2014]. Available from: http://www.rarediseases.org/rare-disease-information/rare-diseases/byID/637/viewFullReport [Google Scholar]
[41]. Aeschlimann A, Kahn MF, Tietze’s syndrome: a critical reviewClin Exp Rheumatol 1990 8:407-12. [Google Scholar]
[42]. Volterrani L, Mazzei MA, Giordano N, Nuti R, Galeazzi M, Fioravanti A, Magnetic resonance imaging in Tietze’s syndromeClin Exp Rheumatol 2008 26(5):848-53. [Google Scholar]
[43]. Moon MS, Tuberculosis of spine: current views in diagnosis and managementAsian Spine J 2014 8(1):97-111. [Google Scholar]