Introduction
Lumbar Spondylolisthesis is a common cause for lower-back pain, radiculopathy, and neurogenic claudication among the adult population. The nonoperative treatment modalities of degenerative spondylolisthesis have remained relatively unchanged during the past two decades; the number of surgical options has increased rapidly over that same period. Lumbar fusion technique using pedicle screw and rods fixation increases the bony union rate and guarantees early mobilization of patients and reduces the need for heavy orthosis. The purpose of this study was to evaluate the clinical and radiological outcome in cases of posterolateral fusion with instrumentation for lumbar spondylolisthesis.
Materials and Methods
This retrospective study analyses the influence of lumbar decompression (laminectomy) and transpedicular instrumentation using titanium pedicle screws and intertransverse process iliac crest graft on patients with degenerative lumbar spondylolisthesis and spinal stenosis. Data was analysed from the case records for the duration from January 2010 to March 2014.
A retrospective clinical study consisting of 56 patients of posterolateral fusion was undertaken to study the effectiveness of the used surgical technique (Lumbar decompression (laminectomy) and transpedicular instrumentation) in improving the clinical outcome and fusion rate, compare the preoperative and postoperative pain and disability, to look for reduction/progression of listhesis [Table/Fig-1], evidence of bony/fibrous fusion and complications of the procedure, to compare and correlate postoperative clinical and radiological outcome. All patients included in the study had undergone lumbar decompression (laminectomy) and transpedicular instrumentation Sectionusing titanium pedicle screws and inter transverse process iliac crest graft. The patients were recommended for surgical procedure after failing non-operative treatment. All patients included, were those having significant back and leg pain with a significant restriction of daily activities due to radicular pain or neurogenic claudication.
Informed written consent was obtained from each participant. The diagnosis of spinal stenosis was established by computed tomography (CT) or MRI. Preoperative plain radiographs of the lumbosacral spine were obtained for all patients. Radiographs were evaluated before surgery for the type of spondylolisthesis and severity of slip for each patient. These included standing anteroposterior and lateral images. All patients were subjected to preoperative CT Lumbosacral spine to document pedicle thickness, degree of bone mineralization and to rule out defect in pars interarticularis.
A self-administered questionnaire was used to assess the postoperative outcome. This questionnaire has been shown to be reproducible, internally consistent, valid, and highly responsive. Three categories were assessed via the questionnaire: symptom severity, physical function status and patient satisfaction.
The self-administered questionnaire was completed by the patients in a return trip to the hospital. Those patients who were unable to return to the hospital were administered the questionnaire through a telephone interview. The duration of follow-up was constant i.e., about six months from date of surgery. Final clinical and radiographic assessments were performed at follow up six months postsurgery. Postoperative radiographs were evaluated for progression/reduction of slip, instrumentation complications and evidence for fusion. Fusion was considered to have occurred if there was a trabeculated mass between the transverse processes of the cephalad and caudad segments. Pseudarthrosis was present if there was no continuity in the fusion mass. Descriptive statistical analysis was carried out in the present study. Results on continuous measurements are presented on Mean ± SD (Min-Max) and results on categorical measurements are presented in Number (%). Significance is assessed at 5% level of significance. Student t-tests (two tailed, dependent) was used to find the significance of study parameters between preoperative and postoperative. Paired proportion test was used to find the significance for evaluation of clinical features between preoperative and postoperative [1,2].
Significant figures
+ Suggestive significance 0.05<p<0.10
* Moderately significant 0.01<p 0.05
** Strongly significant p 0.01
Statistical Analysis
The Statistical software namely SPSS 15.0, Stata 8.0, Med Calc 9.0.1 and Systat 11.0 were used for the analysis of the data and Microsoft word and Excel were used to generate graphs, tables etc.
Results
The ages of the patients ranged from 24 to 74 y (mean 52.48 y). There were 34 (60.7%) women and 22 (39.3%) men. Out of 56 patients, 24 had comorbid conditions. Out of 24 patients, 12 (21.4%) had hypertension, 7 (12.5%) had diabetes mellitus, 2 (3.6%) had coronary artery disease, 2 (3.6%) had bronchial asthma and 1 (1.8%) had hypothyroidism. The duration of symptoms was upto 12 months in 29 (51.8%) of patients. In 18 (32.1%) patients it was 12 to 36 months. Only in 9(16.1%) patients, the duration of symptoms was more than 36 months.
Preoperatively pain was present in back as well as both lower limbs in 24 (42.9%) of patients, 20 (35.7%) patients had back and left lower limb pain whereas 12 (21.4%) patients had back as well as right lower limb pain. Postoperatively, all patients had significant pain relief at 6 monthly follow-up. The intensity of pain as measured by Visual Analog Scale was in the range of 7 to 9 (Mean value 7.52) preoperatively. Postoperatively, it was in the range of 0 to 3 (Mean value 0.3), which was statistically strongly significant (p< 0.001) [Table/Fig-2]. Postoperatively, at 6 monthly follow-up, there was reduction in symptoms of paraesthesia (p-value 0.005, strongly significant), numbness/hypoesthesia (p-value 0.088, suggestive significance) and lower limb stiffness and weakness (p-value 0.046 and 0.015, moderately significant). Although there was significant reduction in urinary symptoms postoperatively, one patient had 18fresh urinary and bowel incontinence, which was not present preoperatively.
Out of 56 patients, 36(64.3%) patients had spondylolisthesis at L4-5 level followed by 14 patients at L5-S1 level (25%). 3 (5.4%) patients had listhesis at 2 levels. Preoperatively 39(69.6%) patients had Grade I listhesis whereas 17(30.4%) had Grade II listhesis. Postoperatively only 1 patient became grade II to grade I listhesis. This was statistically not significant. However, when we compared the mean percentage of spondylolisthesis, there was a statistically strongly significant reduction from 23.11% preoperatively to 15.19% postoperatively (p<0.001).
Adjacent level degeneration was found maximum at L4-5 and L5-S1 levels (5.4% each).This might be attributed to the more number of cases with listhesis at this level. Thirty five (62.5%) patients underwent fusion at L4-5 level followed by 12(21.4%) at L5-S1 level. Two patients underwent 2 level fusion. In one patient, as the L4 pedicles were small because of which L3-5 fusion was done. Out of 56 patients, 53 (94.6%) had good bony fusion demonstrated on postoperative X-ray L-S spine A-P view. Only 3 (5.4%) had pseudoarthrosis at 6 monthly follow-up X-ray.
The preoperative symptom severity score ranged from 14 to 30 (Mean 24.77). The preoperative physical function score ranged from 6 to 18 (Mean 11.79). The postoperative satisfaction score ranged from 5 to 15 (Mean 6.96). All patients required regular pain medications preoperatively. Postoperatively, there was a statistically strongly significant reduction (p<0.001) in number of patients requiring regular pain medications {3 patients (5.4%)}. Out of the 3 (5.4%) patients who had significant postoperative complications, one had wound infection (which resolved with a course of 5 days IV antibiotics), one developed deep vein thrombosis. one patient developed Cauda equine syndrome postoperatively (due to inadvertent retraction of dural tube intraoperatively). None of the patients had implant related complications. The presence of pre-existing comorbid conditions like DM, Hypertension, Coronary Artery Disease, Bronchial Asthma and Hypothyroidism does not seem to contribute towards inadequate bony fusion.
At 6 monthly follow-up, all patients irrespective of Pseudoarthrosis or bony fusion on postoperative X-ray demonstrated significant pain relief. Clinical improvement of pain relief seems to be independent of radiological picture of bony fusion atleast in the short term, whether this pain relief is well sustained, needs to be documented by long-term follow-up of these patients.
The reduction in Mean VAS was from 7.51 to 0.25 in the bony fusion group, which was comparable (7.67 to 1.33) to that in the pseudoarthrosis group. Postoperatively, all the clinical symptoms (paraesthesia, numbness, lower limb weakness, lower limb stiffness and urinary symptoms) were less compared to preoperative status in the bony fusion group. These findings were however statistically not significant. Only one patient in the bony fusion group had reduction in grade of listhesis from grade II to grade I. The reduction in the mean percentage of listhesis was comparable in the bony fusion group (preoperatively 22.46% to postoperatively 14.99%) and pseudoarthrosis group (preoperatively 25.7% to postoperatively 18.83%).
The mean symptom severity score was 24.92 in bony fusion group and 22 in pseudoarthrosis group, which are comparable [Table/Fig-3]. The mean physical function score was 11.74 in bony fusion group and 12.67 in pseudoarthrosis group, which is again comparable [Table/Fig-4].
The mean satisfaction score at 6 monthly follow-up was much better (6.75) in the bony fusion group compared to the pseudoarthrosis group (10.67). The solid fusion group scored statistically significantly better in the postoperative satisfaction scale (p-value 0.004) at 6 monthly follow-up [Table/Fig-5,6].
There was no statistically significant difference discovered between the two groups with respect to the major influencing variables of age, sex, levels fused or diabetes. Clinical outcome was good to excellent in 100% of the patients with solid fusion as well as pseudoarthrosis. Back and lower limb pain scores were statistically significantly improved as well. In short review, good to excellent results have been reported in patients despite a pseudoarthrosis. These results, as shown in the current study, have to be followed up to see if they are maintained over time.
The clinical results of the operation and radiographic findings were then subjected to statistical analysis. Outcome was measured in success of bony fusion and clinical result. The clinical result was excellent if the patients were pain free.
All patients required regular pain medications preoperatively. Postoperatively, only 2 (3.8%) required regular pain medications at 6 monthly follow-up in the bony fusion group, whereas 1 (33%) patient required regular postoperative analgesics in the pseudoarthrosis group. The significance of this finding is questionable due to the small number of patients in the pseudoarthrosis group.
At 6 monthly follow-up, all patients irrespective of Pseudoarthrosis or bony fusion on postoperative X-ray demonstrated significant pain 19relief. Clinical improvement of pain relief seems to be independent of radiological picture of bony fusion atleast in the short term, whether this pain relief is well-sustained, needs to be documented by long-term follow-up of these patients.
Discussion
Traditionally, the surgical management of degenerative lumbar spondylolisthesis consisted of decompressive laminectomy alone. In patients who had a radical decompressive laminectomy in which all of the facet joints were removed, the outcome was poor. In patients who have had a decompressive laminectomy with preservation of a majority of the facet joints, the outcome was dramatically better. The best outcome occurred in those patients who had undergone a decompressive laminectomy combined with a posterolateral intertransverse process arthrodesis.
The assumption that a solid radiographic fusion is associated with a better result is usually valid. The use of instrumentation, although not clearly helpful in improving outcomes, remains a common adjunct to fusion. We generally use instrumentation in all fusions with the exception of patients with osteoporosis.
The use of instrumentation in arthrodesis for lumbar spinal stenosis with degenerative spondylolisthesis remains controversial, but increasing evidence supports the benefits of immediate fixation. Pedicle-screw fixation has been shown to improve the rate of fusion and the clinical outcome after decompression and arthrodesis for degenerative lumbar spondylolisthesis [3]. Early postoperative relief of back pain often is attributed to the immediate stabilization provided by the instrumentation. Internal fixation also reduces the prevalence of postoperative progression of the spondylolisthesis, which can occur even after arthrodesis without instrumentation. Rigid constructs have been associated with a better clinical result than semi-rigid constructs, which allow motion between the fixation screws and the rod or the plate.
Better clinical result has been seen with rigid constructs than the semi-rigid constructs which allow motion between the fixation screws and the rod or the plate. The addition of spinal instrumentation has been advocated by some authors in the operative management of degenerative spondylolisthesis with spinal stenosis [4-6]. The clinical and the radiographic outcome of 41 cases of degenerative spondylolistthesis treated with decompression and instrumented posterior fusion was reported by Booth et al. The satisfaction rate at final clinical evaluation was 83%.This was a retrospective review with a minimum 5-year follow-up (mean 6.5 y). No control group was available for comparison with the study cohort. Back and leg pain questions were grouped together rather than assessed apart. Eight patients had multiple-level fusions for adjacent segment subluxations. This study was one of the longest follow up of patients treated operatively. It showed that approximately, 85% of patients treated like this, who had a solid fusion maintained a stisfactory outcome even after 5 years.Instrumentation has been recommended to increase the fusion rate, decrease the rehabilitation time, and improve patient outcome [7]. However, based on the results of short to intermediate range studies, fusion status does not affect clinical outcome [6,7]. Sufficient stabilization and pain relief of back and lower extremities is provided by a fibrous union.
In a prospective, randomised study by Fischgrund et al., the results of decompression and arthrodesis alone were compared to those of decompression and arthrodesis combined with instrumentation. The results showed that the addition of spinal instrumentation improves the fusion rate (83% vs. 45%) Although pseudoarthrosis developed in 55% of the non-instrumented group, the clinical outcome was still noted to be excellent or good in 15 of 18 patients (83%) [7]. However, based on the results of short to intermediate range studies, fusion status does not affect clinical outcome [6,7]. A fibrous union appears to provide sufficient stabilization and to provide pain relief of the back and lower extremities.
Fischgrund et al., published a prospective, randomized study comparing the results of decompression and arthrodesis alone with those of decompression and arthrodesis combined with instrumentation. The results of this study demonstrated that the addition of spinal instrumentation will improve the fusion rate (83%vs. 45%). Although pseudoarthrosis developed in 55% of the non-instrumented group, the clinical outcome was still noted to be excellent or good in 15 of 18 patients (83%) [7].
The results of this study demonstrated an improved fusion rate in the instrumented fusion group (87% vs. 30%) when compared with the non-instrumented fusion group. Current series is the study of degenerative spondylolisthesis treated with decompression and arthrodesis. All patients were treated with single-level decompression and bilateral pedicle screw fixation for degenerative spondylolisthesis with concurrent spinal stenosis. In our study, the incidence of pseudoarthrosis was 5.4%, which was much better compared to other studies. In our study, all patients had significant postoperative pain relief. In other comparative studies the pain relief ranged from 83% to 93%.
Clinical outcome was good to excellent in 100% of the patients with solid fusion as well as pseudarthrosis. Back and lower limb pain scores were statistically significantly improved as well. In short review, good to excellent results have been reported in patients despite a pseudoarthrosis. These results, as shown in the current study, have to be followed up to see if they are maintained over time. Long-term clinical benefits of an arthrodesis over pseudoarthrosis, with respect to back and lower leg symptomatology, would be realized on long-term follow-up of these patients.
A successful arthrodesis correlates with better radiologic parameters as well as an improved clinical outcome. In this study, the solid fusion and pseudoarthrosis groups had similar preoperative demographics. Preoperative radiographs were analysed in an attempt to identify radiographic measures of spondylolisthesis severity, which may influence fusion outcome. The initial spondylolisthesis was not predictive of radiographic fusion. In 94.6% patients, in whom a solid fusion was achieved, the preoperative mean listhesis was 22.46% whereas mean listhesis in the 5.4% patients in whom a pseudoarthrosis developed was 25.7%. The post-operative mean listhesis in the bony fusion and pseudoarthrosis group were 14.99% and 18.83% respectively. This difference was statistically not significant.
Numerous studies have outlined the difficulty in determining fusion status from radiographs, and methods for evaluating the fusion mass vary widely. The only accurate method is visual inspection, which is usually not practical. In the current study, the fusion mass was evaluated as critically as possible, using plain radiographs-hence, the 94.6% reported fusion rate, which is contrary to the high clinical success rate (100% in our study).
Showing preoperative and postoperative imaging with postoperative reduction in spondylolisthesis. There is also significant reduction in postoperative pain intensity as per VAS (Visual analogue scale)
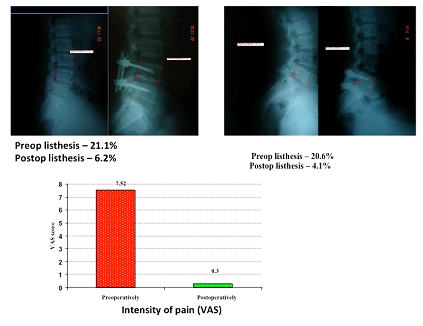
Shows preoperative and postoperative pain intensity (VAS) with significant reduction in postoperative pain
| Intensity of pain | VAS score |
|---|
| Range | Mean ± SD | Median |
|---|
| Preoperatively | 7-9 | 7.52±0.68 | 7.0 |
| Postoperatively [ at 6 monthly followup ] | 0-3 | 0.30±0.74 | 0.0 |
| Inference | Intensity of pain is significantly reduced postoperatively with Z=6.444; p<0.001** |
Shows the comparison of preoperative symptoms between the 2 groups (bony fusion and pseudoarthrosis)
| Symptom Severity scale - Preoperative | Bony fusion(n=53) | Pseudoarthrosis(n=3) |
|---|
| Range | Mean±SD | Range | Mean±SD |
|---|
| 1.The pain you have had on average including pain in your back, buttocks and pain that goes down the legs ? | 4-5 | 4.91±0.29 | 3-5 | 4.33±1.16 |
| 2.How often have you had back, buttock, or leg pain? | 3-5 | 3.74±0.66 | 1-4 | 2.67±1.53 |
| 3.The pain in your back or buttocks? | 3-5 | 4.60±0.79 | 3-5 | 4.33±1.16 |
| 4.The pain in your legs or feet? | 3-5 | 4.13±0.79 | 3-4 | 3.33±0.58 |
| 5.Numbness or tingling in your legs or feet? | 1-5 | 3.60±1.28 | 1-4 | 3.00±1.73 |
| 6.Weakness in your legs or feet? | 1-4 | 2.74±0.86 | 2-3 | 2.67±0.58 |
| 7.Problems with your balance? | 1-3 | 1.30±0.72 | 1-3 | 1.67±1.16 |
| Total | 19-30 | 24.92±2.69 | 14-27 | 22.00±7.00 |
Shows the comparison of preoperative physical functions between the 2 groups (bony fusion and pseudoarthrosis)
| Physical Function scale -preoperative | Bony fusion(n=53) | Pseudoarthrosis(n=3) |
|---|
| Range | Mean±SD | Range | Mean±SD |
|---|
| 1.How far have you been able to walk? | 2-4 | 2.64±0.83 | 2-4 | 3.00±1.00 |
| 2.Have you taken walks outdoors or in malls for pleasure? | 1-4 | 2.49±1.05 | 2-4 | 3.00±1.00 |
| 3.Have you been shopping for groceries or other items ? | 1-4 | 2.51±0.95 | 2-3 | 2.67±0.57 |
| 4.Have you walked around the different rooms in your house or apartment? | 1-3 | 2.09±0.56 | 2-2 | 2.00±0.00 |
| 5.Have you walked from your bedroom to the bathroom? | 1-3 | 2.00±0.52 | 2-2 | 2.00±0.00 |
| Total | 6-18 | 11.74±3.50 | 10-15 | 12.67±2.52 |
Shows the comparison of postoperative satisfaction scale between the 2 groups (bony fusion and pseudoarthrosis)
| Satisfaction scale - Postoperative | Bony fusion(n=53) | Pseudoarthrosis(n=3) |
|---|
| Range | Mean±SD | Range | Mean±SD |
|---|
| 1.The overall result of back operation? | 1-2 | 1.23±0.42 | 1-4 | 2.33±1.53 |
| 2.Relief of pain following the operation? | 1-3 | 1.34±0.65 | 1-4 | 2.67±1.53 |
| 3.Your ability to walk following the operation? | 1-2 | 1.23±0.42 | 1-3 | 2.00±1.00 |
| 4.Your strength in the thighs, legs, and feet? | 1-2 | 1.74±0.45 | 2-3 | 2.33±0.58 |
| 5.Your balance, or steadiness on your feet? | 1-2 | 1.23±0.42 | 1-2 | 1.33±0.58 |
| Total | 5-11 | 6.75±2.06 | 6-15 | 10.67±4.51 |
Shows the comparative value of the 2 preoperative and 1 postoperative scales between the two groups (bony fusion and pseudoarthrosis). There is a significant difference in the postoperative satisfaction scale when compared between the 2 groups
| Study parameters | Bony fusion (n=53) | Pseudoarthrosis (n=3) | p value |
|---|
| Symptom Severity scale –Preoperative | 24.92±2.69 | 22.00±7.00 | 0.103 |
| Physical Function scale - Preoperative | 11.74±3.50 | 12.67±2.52 | 0.652 |
| Satisfaction scale - Postoperative | 6.75±2.06 | 10.67±4.51 | 0.004** |
Limitations Of Study
For lumbar spondylolisthesis, the most stenotic area is generally located at the unstable motion segment, where image study shows slippage. However, coexistent stenosis at the adjacent motion segments owing to degeneration is not uncommon. If the decompressed area exceeds the fused level, then the incidence of developing adjacent instability increases significantly. This aspect, which was not considered in our study, needs to be looked into in long-term follow-up studies. Smoking is an important factor adversely affecting bony fusion. This aspect was not looked into in this study.
Lateral flexion-extension radiographs of lumbosacral spine obtained preoperatively and compared with similar study postoperatively are useful to demonstrate angular motion between the adjacent end plates or sagittal motion at the location of the spondylolisthesis. However, due to resource constraints, only neutral erect X-rays of lumbosacral spine were included in our study.
Outcome of pseudoarthrosis cases deteriorates over time and solid fusion produces better long-term outcome. As the mean duration of follow-up was only six months, these aspects could not be ascertained in this study. A relatively significant percentage of patients had a health insurance scheme, and this may have influenced the clinical results and also may not be readily generalizable to practices with higher percentages of self-funding patients.
Conclusion
Based on the findings and analysis of our study we recommend that:
1. Initial treatment for degenerative lumbar spondylolisthesis must be conservative.
2. Surgical intervention is necessary for managing disabling symptoms inspite of adequate conservative measures, progressive neurologic deficit, and poor quality of life.
3. As surgical fusion has been demonstrated to have the potential to improve the patients’ symptoms sufficiently to make an important subjective and objective (measurable) difference, we recommend “Decompressive laminectomy with posterolateral instrumentation (pedicle screws) and intertransverse process arthrodesis with autogenous bone graft” as the procedure of choice for management of lumbar spondylolisthesis.
Degenerative lumbar spondylolisthesis most often occurs in women older than 40 years. Surgical intervention is indicated for managing leg pain, progressive neurologic deficit, and poor quality of life. The surgical procedure of choice is decompressive laminectomy with posterolateral instrumentation (pedicle screws) and intertransverse process arthrodesis with autogenous bone graft. Decompression primarily relieves radicular symptoms and neurogenic claudication whereas fusion primarily relieves back pain by elimination of instability. The addition of posterolateral instrumentation (pedicle screws) enhances the ability to obtain a solid arthrodesis. A successful fusion correlates with an improved functional outcome, better patient satisfaction and less back and lower limb symptomatology. Posterolateral instrumentation enables improved functional outcome, better patient satisfaction and less back and lower limb symptomatology. This is irrespective of bony arthrodesis or pseudoarthrosis, atleast in the short term followup. The amount of preoperative spondylolisthesis did not correlate with radiographic fusion status. Restoring a patient with chronic low back pain to normalcy is beyond the expectation of surgical fusion, regardless of technique used. The goal instead is to improve the patients’ symptoms sufficiently to make an important subjective and hopefully also objective (measurable) difference, as compared with the effects of natural history, placebo or other nonsurgical treatment options. Surgical fusion has been demonstrated to have this potential.