An Unusual Traumatic Lamellar Laceration of Cornea
Rakesh K Barot1, Amar Karkhanis2, Satish C Shitole3
1Associate Professor and HOD, Department of Ophthalmology, Rajiv Gandhi Medical College and CSMH, Kalwa, Thane, Maharashtra, India.
2Honorary Ophthalmologist, Department of Ophthalmology, Rajiv Gandhi Medical College and CSMH, Kalwa, Thane, Maharashtra, India.
3Assistant Professor, Department of Ophthalmology, Rajiv Gandhi Medical College and CSMH, Kalwa, Thane, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rakesh K Barot, 12, Jyoti Nagar, Near RTO, Four Banglows, Andheri West, Mumbai 400053, India.
E-mail: rakesh_barot23@yahoo.com
Lamellar laceration of the cornea may occur following ocular trauma. The management of lamellar laceration will depend on whether the lacerated corneal flaps are displaced or undisplaced. We hereby report an unusual case of large traumatic lamellar corneal laceration in right eye in a 14-year-old girl presenting with diminution of vision. Slit lamp biomicroscopic examination showed partial thickness corneal flap of 11.5mm X 7mm from 11o’clock to 6 o’clock position with 3 mm superonasal displacement associated with stromal folds and shifting of inferior limbus and conjunctiva. Surgery was the appropriate option which included visualization of inferior limbus by incising conjunctiva, repositioning of displaced corneal flap and securing it with sutures. Immediate examination and proper surgical management of lamellar corneal injuries results in good visual outcome and prevention of complications like fibrous ingrowth and infection.
Closed globe injury, Displaced flap, Partial thickness laceration of cornea
Case Report
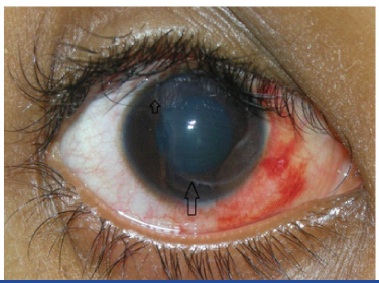
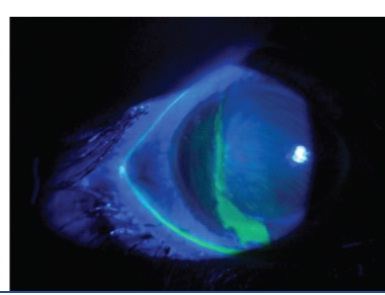
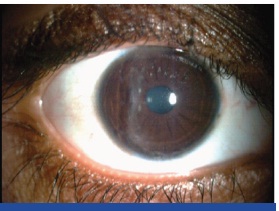
A 14-year-old girl presented at Ophthalmology department of Rajiv Gandhi Medical College and Chatrapati Shivaji Maharaj Hospital, Thane with recent history of accidental trauma (six hours ago) to the right eye with geyser pipe followed by sudden decrease in vision. Patient’s written informed consent was obtained prior writing this case report. On examination her vision in right eye was 2/60 with accurate projection and perception of light. Slit lamp examination revealed a partial thickness corneal flap which started close to 11 o’ clock limbus and extended to 6 o’ clock limbus without crossing the visual axis [Table/Fig-1a,1b]. The flap was 11.5 mm x 7 mm in size approximately with stromal folds and ill defined and sloping edges. It was displaced 3mm supero nasally as evidenced by shifting of the inferior limbus and conjunctiva. The anterior chamber was normal in depth and contents. Flurescein staining revealed the extent of displacement of flap [Table/Fig-2]. Seidel’s test was negative. The flap-stroma interface showed blood pigments and foreign body particles. Multiple small subconjunctival haemorrhages were noticed in nasal and inferior bulbar conjunctiva.
The injury was clinically diagnosed as large traumatic lamellar laceration of cornea with displaced flap. According to The Ocular Trauma Classification Group [1], it was classified as: a closed-globe injury, type B, grade 4 visual acuity and negative Relative Afferent Pupillary Defect. The rest of the right and left eye examination was otherwise normal. Repair of partial thickness corneal laceration was done under peribulbar block with intravenous sedation. Corneal flap was separated and elevated with iris repositor. The bed and undersurface of the displaced flap were irrigated with balanced salt solution to clean off debris, blood and foreign body particles to prevent epithelial ingrowth. The displaced conjunctiva was incised from the corneal flap to identify the limbus at 6o‘clock. The displaced flap was repositioned and secured with 10-0 nylon interrupted sutures. The first suture was placed at 7 o’clock to form the limbus as it is one of the landmarks in suturing corneoscleral laceration. The sutures were partial thickness through the surrounding stroma. The tightness and number of sutures were just enough to hold the flap in place [Table/Fig-3a].
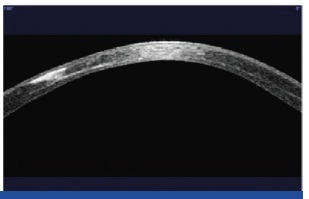
Postoperatively patient was advised topical antibiotic and steroid eye drops for four weeks with tapering dose and frequent application of lubricating eye drops for six weeks. Proper hygiene of both eyes along with use of dark glasses was advised to prevent contamination of corneal wound. On 3rd postoperative day her vision was 6/36 and 6/18 with pinhole. At four weeks, the best corrected visual acuity (BCVA) was 6/12 with -2 D/ -1.5 x120. Alternate suture removal was done at 4th and 6th week. At 8 weeks, her BCVA was 6/12 with -2.5 D -3.5 x 100 and a healed corneal scar was noted [Table/Fig-3b]. Follow up at one year, the BCVA was 6/12 with -4.0 D-2.5 x120. Slit lamp examination revealed a well healed corneal scar without any evidence of epithelial ingrowth and vascularisation [Table/Fig-4a]. The anterior Optical Coherence Tomography (OCT) study showed well healed scar and proper apposition of corneal flaps [Table/Fig-4b].
Discussion
The external location of cornea predisposes it to a variety of sight threatening insults. Corneal injury is a very common entity associated with ocular trauma and one of the most important causes of unilateral vision loss in developing countries [2]. Traumatic lamellar lacerations of cornea are of two types depending upon whether the flap is displaced or undisplaced. Corneal laceration with undisplaced flap is treated with either bandage contact lens or fibrin glue or both. The displaced flap is repositioned and secured with sutures.
Review of literature has revealed only four cases of lamellar corneal laceration which were of undisplaced corneal flap. A case of lamellar corneal injury by bamboo splinters and their removal by making corneal incisions is reported [3]. Second report describes a novel use of fibrin glue in the treatment of partial thickness corneal laceration that had failed to heal spontaneously over one year [4]. Other two reports have described the complications of traumatic lamellar laceration such as epithelial ingrowth and infectious keratitis [5,6]. Grade 2 Epithelial ingrowth after primary conservative management of traumatic lamellar laceration in a 45-year-old woman has occurred two months following injury which resulted in severe visual impairment [5]. Hyperacute infectitious keratitis with Plesiomonas shigelloids following traumatic lamellar laceration by rock is reported in a 13-year-old girl who developed scarring of cornea with neovascularization and associated poor visual outcome inspite of adequate medical treatment [6].
Corneal trauma in domestic setting is common but injury due to geyser pipe is unusual. In present case the geyser pipe trauma resulted in penetration of the cornea with a large displaced flap without perforation. The possible explanation for this phenomenon may be that the combination of enough rigidity of the pipe along with sufficient flexibility avoided the perforation of the cornea.
A remarkable feature of this case was flap size (11.5 mm x 7 mm) and supero nasal displacement of flap without causing serious injury to other parts of the eyeball. The postoperative BCVA was 6/12 and complications like infection and epithelial ingrowth did not occur. The contributory factors for good visual recovery in the present case are: scar in non visual axis area, identification of true extent of the lamellar laceration, irrigation of the bed and undersurface of the flap and proper flap alignment. To the best of our knowledge this is the first report of management of large traumatic lamellar laceration of cornea with displaced flap.
Day-1 showing displaced corneal and conjunctival flap with blood pigments in the interface
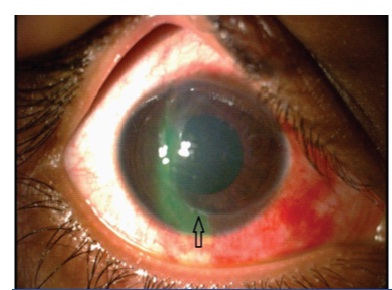
Day-2 showing reduced inflammation
Extent of displacement of corneal flaps after Fluorescein staining
Slit lamp microscopic photographs day-1 after surgery

Slit lamp microscopic photographs at 8th week after surgery
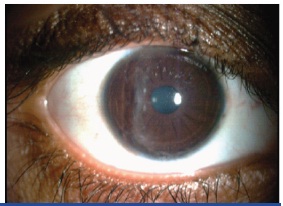
Slit lamp microscopic photographs at one year after surgery
Anterior OCT one year after surgery showing proper apposition of corneal flaps
Conclusion
Proper primary management of large traumatic lamellar laceration of cornea with displaced flap can provide good visual outcome and prevent complications.
[1]. DJ Pieramici, P Sternberg, TM Aaberg, A system for classifying mechanical injuries of the eye.Am J Ophthalmol 1997 123:820-31. [Google Scholar]
[2]. R Dandona, L Dandona, Corneal blindness in a southern Indian population: need for health promotion strategiesBr J Ophthalmol 2003 87(2):133-41. [Google Scholar]
[3]. M Kawashima, T Kawakita, C Shigeyasu, J Shimazaki, Lamellar corneal injury by bamboo splinters: a case reportJournal of Medical Case Reports 2009 3:7226 [Google Scholar]
[4]. C Kiire, S Srinivasan, M Stoddart, Novel use of fibrin glue in the treatment of a partial thickness corneal lacerationBr J Ophthalmol 2010 94(6):810-11. [Google Scholar]
[5]. R Bansal, AK Jain, J Sukhija, Epithelial ingrowth within the interface following traumatic corneal lamellar laceration.Ophthalmic Surgery, Lasers and Imaging 2008 39(3):217-20. [Google Scholar]
[6]. JM Klatte, MH Dastjerdi, K Clark, CJ Harrison, F Grigorian, ED Stahl, Hyperacute infectious keratitis with Plesiomonas shigelloides following traumatic lamellar corneal LacerationPediatr Infect Dis J 2012 31(11):1200-01. [Google Scholar]