Variant Branching Pattern of Superior Thyroid Artery and Its Clinical Relevance: A Case Report
Rohini Motwani1, Saroj Kaler Jhajhria2
1 Senior Resident, Department of Anatomy, All India Institute of Medical Sciences, New Delhi, India.
2 Assistant Professor, Department of Anatomy, All India Institute of Medical Sciences, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Saroj Kaler Jhajhria, Assistant Professor, Department of Anatomy, All India Institute of Medical Sciences, New Delhi, India. E-mail : sarojkaler@gmail.com
Thyroid surgeries are most common neck surgeries; hence thorough knowledge of the blood supply of this gland to the surgeons is of immense importance to prevent any alarming haemorrhage. We report a rare unilateral branching pattern of superior thyroid artery (STA) on right side during routine dissection on an adult male cadaver in the Department of Anatomy, A.I.I.M.S, New Delhi. Left superior thyroid artery was normal. The common trunk (CT) arose from anterior surface of right external carotid artery (ECA) just above the bifurcation of common carotid artery (CCA) soon dividing into five branches i.e., infrahyoid, superior laryngeal, superior thyroid, cricothyroid and sternocleidomastoid artery. This variant branching pattern of STA is very rare. The inferior thyroid arteries did not show any unusual distribution. Knowledge of such arterial variations related to the thyroid gland is immensely helpful to the surgeons to avoid damage of the vital organs in this region.
Surgical anatomy, Thyroid gland, Variations
Case Report
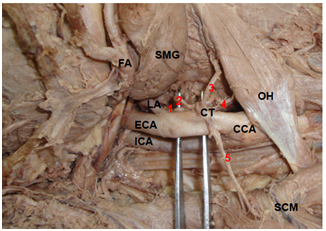
During the routine dissection, the unilateral variation in right superior thyroid artery (STA) was dissected in an adult male cadaver. Skin and fascia were dissected to view the contents of the anterior triangle of the neck. Muscles were retracted. A common trunk (CT) was observed, arising from anterior surface of right external carotid artery (ECA) just above the bifurcation of common carotid artery (CCA), which soon divided into five b`ranches i.e., infrahyoid, superior laryngeal, cricothyroid, superior thyroid, and sternocleidomastoid artery [Table/Fig-1,2].
Dissection of anterior triangle of neck showing Common Trunk (CT) arising from right External carotid artery (ECA), 1: Infrahyoid, 2: Superior laryngeal, 3: Superior thyroid, 4: Cricothyroid, 5: Sternocleidomastoid artery. SCM: Sternocleidomastoid, ICA: Internal carotid artery, CCA: Common carotid artery, LA: Lingual artery, FA: Facial artery, SMG: Sub-mandibular gland, OH: Omohyoid
Dissection of anterior triangle of neck after cutting omohyoid muscle (Right side) showing superior laryngeal artery (2) accompanying internal laryngeal nerve (arrow), 1: infrahyoid artery, 3: Superior thyroid artery,4: Sternocleidomastoid artery, ECA: External carotid artery, CCA:Common carotid artery, IJV:Internal jugular vein, SCM: Sternocleidomastoid, TG: Thyroid gland, SH: Sternohyoid (cut ends)
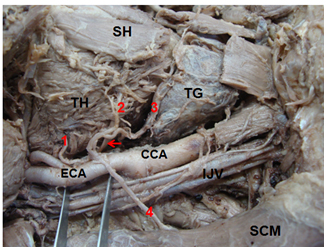
Unusually STA arose from the CT along with other branches and was thinner in calibre than the normal artery. The infrahyoid artery was a small branch running along the lower border of the hyoid bone deep to supply the infrahyoid strap muscles. The superior laryngeal artery accompanied the internal laryngeal nerve [Table/Fig-2,arrow]. Deep to The thyroid muscle it was seen piercing the lower part of the thyrohyoid membrane to supply the tissues of the upper part of the larynx. Cricothyroid branch ran towards the cricothyroid muscle. The sternocleidomastoid artery descended laterally across the carotid sheath and supplied the middle region of sternocleidomastoid (SCM). Superior thyroid branch was running along the medial side of lateral lobe of TG [Table/Fig-2], and upper border of isthmus to anastomose with its opposite fellow and supplied TG as usual. Thus we observed a rare branching pattern of STA. The inferior thyroid arteries did not show any unusual distribution. Studies indicate that in 20-45% of cases, the superior parathyroid glands (SPTG) also receive significant Vascular supply from the STA. Thus knowledge of variant vasculature of thyroid gland (TG) and SPTG is of immense importance for some surgical procedures such as radical neck dissection, reconstruction of aneurysm and interventional radiology [Table/Fig-1,2].
Discussion
Vascular supply of the thyroid gland is of immense importance to the clinicians dealing with the neck region. Variations in the thyroid vasculature are frequently documented in classical anatomical, surgical and radiological text books. The STA is the main source of Blood supply to the TG, upper part of the larynx and neck region. It arises from anterior surface of ECA just below the level of greater cornu of the hyoid bone. It descends along the lateral border of thyrohyoid to reach the apex of the lobe of the TG. Occasionally it may issue directly from the common carotid artery [1]. The artery has the following named branches: infrahyoid, superior laryngeal, sternocleidomastoid and cricothyroid.
The present case, reports a CT arising from anterior surface of right ECA just above the bifurcation of CCA soon dividing into five branches i.e., infrahyoid, superior laryngeal, superior thyroid, cricothyroid and sternocleidomastoid artery [Table/Fig-1,2]. The left STA did not show any variations. Lucev et al., [2] reported that STA arises more often from the CCA in 47.5% of cases and in 35.14% of cases by Sanjeev et al., [3] Morriggl et al., [4] reported a case of complete absence of left superior thyroid artery which was replaced by thyroid ima artery. In an Indian study by Anitha et al., STA origin from CCA bifurcation was noted in 19% of cases [5] [Table/Fig-3].
Comparison of present observations with previous studies on the basis of origin of Superior Thyroid Artery (STA)
| Studies Done | Lucev et al., [2] | Sanjeev et al., [3] | Morriggl et al., [4] | Anitha et al., [5] | Present study |
|---|
| Origin of STA | From the CCA in 47.5% of cases | From the CCA in 35.14% of cases | Complete absenceof left STA which was replaced by thyroid ima artery | From CCA bifurcation in 19% of cases | A CT, arising from right ECA just above the bifurcation of CCA |
In contrast to the data concerning the origin of STA, very few literature is available regarding the branching pattern of STA. Pankaj Gupta et al., [6] in an angiographic study categorized the branching patterns of STA into three types: Type I (bifurcation), type II (trifurcation), and type III (non-bifurcation, non-trifurcation). Type I pattern was defined as the one in which the STA divided to give two major branches with rest of the branches arising from these branches. Similarly, type II pattern was said to be present when the STA gave three major branches. In type III pattern, there was random origin of the branches, not conforming to either of the former two patterns. Ozgur et al., classified STA into six types depending on the branching pattern [7]. Hu et al., reported similar branching pattern [8]. Thus, we report a very rare unilateral variation of STA as a CT, which in our knowledge has never been reported [Table/Fig-4].
Comparison of present observations with previous studies on the basis of branching pattern of Superior Thyroid Artery (STA)
| Studies Done | Pankaj Gupta et al., [6] | Ozgur Z et al., [7] | Hu KS et al., [8] | Present study |
|---|
| Branching Pattern of STA | In an angiographic study, categorized into three types | Classified into six types | Same as Ozgur Z et al., | Unilateral CT soon dividing into five branches |
The variations might be related to changes in the transformation of the aortic arch system in the embryo [9]. The ECA and its branches are formed after a complicated process of angiogenesis [10]. It includes annexation and regression of the vessels with some remodelling. Deviation in the normal stages of annexation and regression during angiogenesis leads to the anomalous structures [10]. Knowledge of surgical anatomy of the STA ensures maintaining a bloodless field during major radical neck dissection surgeries to minimize postoperative complications.
Conclusion
Profound knowledge of the anatomy and variations of STA is of immense importance for clinicians to avoid iatrogenic injuries and postoperative complications in various procedures such as radical neck dissection, thyroidectomy, reconstruction of aneurysm and intervention radiology. Description of arterial and venous variations, especially if they are of rare occurrence is important for interpretation within the scope of modern imaging techniques.
Knowledge of this variation would be helpful for the clinicians planning surgeries in this region to minimize the complications.
[1]. Standring S, Ellis H, Healy JC, Johnson D, William A, Collins P, Gray’s Anatomy: The Anatomical Basis of Clinical Practice 2005 39th EdLondonElsevier, Churchill Livingstone:543-47. [Google Scholar]
[2]. Lucev N, Babinac D, Maric I, Drescik I, Variations of the great arteries in the carotid triangleOtolaryngol Head and Neck Surg 2000 122:590-91. [Google Scholar]
[3]. Sanjeev IK, Anita H, Aswini M, Mahesh U, Rairam GB, Branching pattern of external carotid artery in humansJournal of Clinical and Diagnostic Research 2010 4:3128-33. [Google Scholar]
[4]. Morriggl B, Sturm W, Absence of three regular thyroid arteries replaced by an unusual lowest thyroid artery (Arteria thyroidea ima): A case reportSurg Radio Anatomy 2001 23:135-37. [Google Scholar]
[5]. Anitha T, Dombe D, Asha K, Kalbande S, Clinically relevant variations of the superior thyroid artery: An anatomic guide for neck surgeriesInt J Pharm Biomed Sci 2011 2:51-54. [Google Scholar]
[6]. Gupta Pankaj, Bhalla Ashu Seith, Thulkar Sanjay, Kumar Atin, Mohanti Bidhu Kalyan, Variations in superior thyroid artery: A selective angiographic studyIndian Jr of Radio 2014 4(1):66-71. [Google Scholar]
[7]. Ozgur Z, Govsa F, Celik S, Ozgur T, Clinically relevant variation of the superior thyroid artery: An anatomic guide for surgical neck dissectionSurg Radiol Anat 2009 31:151-59. [Google Scholar]
[8]. Hu KS, Song WC, Kim SH, Choi SW, Han SH, Paik DJ, Branching patterns of the arterial branches supplying the middle vascular pedicle of the sternocleidomastoid muscle: A topographic anatomical study with surgical applications for the use of pedicles osteomuscular flapsSurg Radiol Anat 2006 28:7-12. [Google Scholar]
[9]. Eid N, Ito Y, Otsuki Y, Anomalous branching pattern of external carotid artery: Clinical relevance to cervicofacial surgeryClin Anat 2011 24:953-55. [Google Scholar]
[10]. Mahendrakar MA, Variation in the branching pattern of external carotid artery; a case reportJ Anat Soc India 2007 56:47-51. [Google Scholar]